The question of whether Obsessive Compulsive Disorder (OCD) falls under the category of neurodivergence is something people are asking me about more and more as mental health issues are increasingly common amongst children and adults. For three decades, I have supported the neurodivergent and those with mental health issues across a variety of settings.
This topic, while intriguing, is not black and white and opens up a realm of debate and discussion in the mental health community.
The Debate: Is OCD Considered Neurodivergent?
The question of whether OCD is neurodivergent lies at the intersection of evolving understandings of brain function, mental health, and the neurodiversity movement. Neurodivergence typically includes conditions like autism, ADHD, and dyslexia, recognized for their distinct neurological make-up.
OCD, traditionally viewed as an anxiety disorder due to its hallmark obsessions and compulsions, poses a unique case. Its inclusion as a form of neurodivergence is debatable and hinges on broader definitions and perceptions of neurodiversity and whether or not mental health conditions should be included due to so many root causes.
Exploring the Layers of Neurodiversity and OCD
By understanding the diverse spectrums of brain function and mental health conditions, we can gain insights and guidance for parents navigating these waters with their children.
Instead of only thinking about life long conditions, we are moving toward empowerment and using neurodivergent strengths to help individuals find success. It may mean school or work accommodations that allow for equity.
What Does Neurodivergent Mean?
Neurodivergence meaning refers to variations in the human brain regarding sociability, learning, attention, mood, and other mental functions.
The neurodiversity definition is often used in the neurodiversity movement, which advocates for the acceptance of neurological differences as natural human variations. This perspective includes conditions like autism, ADHD, dyslexia, and potentially, OCD, which can be thought as by some as ‘neurodivergent disorders.'
With the rise in neurodivergence, it is harder to even determine what makes someone neurotypical today! The neurodivergent brain is increasingly the norm.
Understanding the Core Features of Neurodiversity
As we delve into the intricate relationship between Obsessive Compulsive Disorder and neurodivergence, it's essential to first understand what neurodiversity entails.
So, what does it mean to be neurodivergent? Neurodiversity has become a concept that's reshaping our understanding of neurological differences.
By exploring these core features, we'll gain a clearer perspective on how conditions like OCD might fit within the broader neurodiverse spectrum.
Neurodiversity celebrates the idea that there's no single “normal” or “right” type of brain or mind. It isn't about neurodivergent symptoms but rather variations. You may wonder, “What is neurodivergent?,” “What is neurodivergence?” or “what is neurodiverse?” and be confused about neurodiversity meaning.
Neurodivergent core features include:
- Variation and Individuality: Recognizing that every brain functions uniquely.
- Acceptance and Inclusivity: Promoting acceptance of diverse neurological conditions.
- Understanding and Adaptation: Encouraging a deeper understanding of different neurotypes and adapting environments to be more inclusive.
Are People With OCD Considered Neurodivergent?
The classification of OCD as a form of neurodivergence is debated. While OCD involves unique brain function and challenges similar to other neurodivergent conditions, it's traditionally viewed more as an anxiety disorder (although distinctly different). However, the neurodiversity movement's inclusive approach opens up conversations about whether OCD should be considered under this umbrella.
OCD: Key Features and Definitions
What does OCD stand for and what does it mean? OCD stands for Obsessive Compulsive Disorder, which is a complex mental health condition that extends far beyond the common misconceptions of mere cleanliness or orderliness. It's characterized by a pattern of unwanted thoughts and fears (obsessions) that lead to repetitive behaviors (compulsions). These symptoms go deeper into the psychological fabric of an individual, significantly affecting their daily life and overall well-being.
Is OCD on a spectrum as commonly portrayed in the media? Yes and no. OCD symptoms vary from person to person and can wax and wane depending on a variety of factor. It also co-occurs with other conditions. While many wonder if OCD is a sign of autism, it isn't. OCD and ASD do co-occur at a high rate and behaviors such as OCD stimming can be overlapping.
To learn more about what's the difference between autism and neurodivergent brain, listen to my It's Gonna Be OK! podcast series on OCD.
Understanding Obsessions
- Nature of Obsessions: These are intrusive, persistent thoughts, images, or urges that trigger intensely distressing feelings. Unlike everyday worries about real-life problems, obsessions are excessive and not proportionate to the actual risk involved.
- Common Obsessions: They can include fears of contamination, intense worry about safety or harm (to oneself or others), and deeply ingrained fears of making mistakes or acting against personal morals or religious beliefs.
- Impact on the Individual: Obsessions often cause significant anxiety or discomfort. The individual usually tries to ignore or suppress these thoughts or neutralize them with some other thought or action, leading to compulsions.
Understanding Compulsions
- Nature of Compulsions: Compulsions are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession. The behaviors typically aim to prevent or reduce anxiety related to the obsessions or prevent some dreaded event or situation; however, these acts are not connected in a realistic way with what they are designed to neutralize or prevent, or they are clearly excessive.
- Common Compulsions: These can range from physical behaviors like handwashing, checking, or arranging objects in a particular way, to mental acts like praying, counting, or repeating certain words silently.
- The Compulsive Cycle: Engaging in these compulsions provides temporary relief from the anxiety caused by the obsessions, but this relief is short-lived. This often leads to a reinforcing cycle, where the more the individual performs these compulsions, the more they feel the need to continue doing so.
The Impact of OCD on Daily Life
- Disruption in Daily Activities: The intensity of the obsessions, compulsions and rituals can consume hours of a person's day, significantly interfering with their daily activities, social interactions, work, and family responsibilities.
- Emotional and Physical Toll: The chronic nature of this cycle can lead to a range of emotional challenges, including feelings of shame, guilt, or frustration. Physically, it can lead to exhaustion or even manifest as physical symptoms related to the compulsive behaviors (like skin irritation from excessive washing).
- Need for Control and Certainty: A hallmark of OCD is the overwhelming need for control and certainty in the face of their obsessions. This often leads to a paradox where the more control they seek, the less in control they feel and the more they ruminate. This can especially impact relationships.
Understanding these key features and definitions of OCD is crucial in recognizing its complexity and the profound impact it has on those who suffer from it. This comprehension forms the foundation for exploring how OCD relates to the concept of neurodiversity and what this means for treatment and support for individuals with OCD.
What are the Types of OCD?
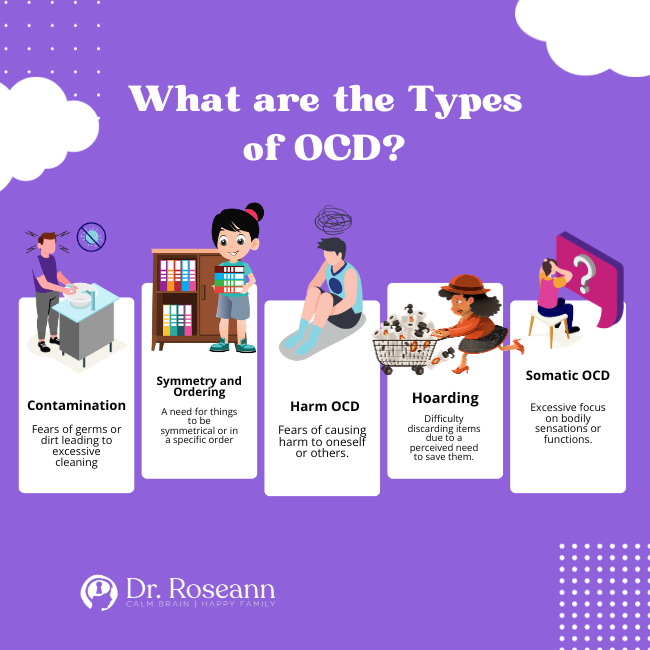
OCD manifests in various forms, each with its own set of obsessions and compulsions. Internal OCD is common and outwards manifestations often take time to develop.
Common types of OCD include:
- Contamination: Fears of germs or dirt leading to excessive cleaning.
- Symmetry and Ordering: A need for things to be symmetrical or in a specific order.
- Harm OCD: Fears of causing harm to oneself or others.
- Hoarding: Difficulty discarding items due to a perceived need to save them.
- Somatic OCD: Excessive focus on bodily sensations or functions.
Expanding the Scope: Mental Health Conditions as Forms of Neurodivergence
The concept of what is considered neurodivergent has traditionally associated with developmental disorders like autism and ADHD, is increasingly being applied to a range of mental health conditions, including Obsessive Compulsive Disorder. This broadened perspective reflects a growing understanding and acceptance of the diverse ways in which the human brain can function.
Neurodivergence and Mental Health: A Closer Look
Unique Brain Functioning
Mental health conditions like OCD are characterized by distinct patterns of thought and behavior, indicative of unique brain functioning.
So, what is a neurodivergent brain? neurodivergent brain meaning is as varies a a neurodivergent brain! Neurodivergent brains have strengths and differences. This aligns with the neurodiversity paradigm, which emphasizes variations in neurological functioning as part of the human experience.
Breaking Down Stigmas
By viewing mental health conditions as forms or signs of neurodivergence, there's an opportunity to challenge and reduce the stigma often associated with these conditions. It promotes a view of mental health differences and neurodivergent traits not as deficits, but as variations that need understanding and support.
Holistic Understanding
This perspective encourages a more holistic understanding of individuals, recognizing that their experiences and behaviors are deeply intertwined with how their brain processes information and emotions.
The Evolving Conversation About Neurodivergence and Mental Health
There has been a shift in perception about what constitutes a neurodivergent brain. As our understanding of the brain and mental health continues to evolve, so too does the conversation around neurological divergence. Mental health conditions like OCD are increasingly being seen through the lens of neurodiversity, enriching our understanding of these experiences.
We want to empower individuals and move away from the stigma of mental health. By recognizing the neurodivergent nature of these conditions, individuals are empowered to embrace their unique experiences. This can lead to increased self-acceptance and a reduction in the internalization of negative societal attitudes. It also has many wondering, “Am I neurodivergent?”
Can You Become Neurodivergent?
Neurodivergence is generally seen as an inherent aspect of one’s neurological makeup. While one cannot become neurodivergent in the traditional sense, conditions like OCD can emerge due to a combination of genetic, biological, and environmental factors, highlighting the complex nature of brain function and mental health.
How Does Neurodiversity Impact Treatment?
Being neurodivergent does impact treatment and requires a higher level of practitioner training and compassionate care. Using natural solutions that calm and regulate the brain can help the child or individual be more connected and confident.
Implications for Treatment and Support
Personalized Approaches
Recognizing mental health conditions as neurodivergent necessitates more personalized and empathetic approaches to treatment. This can lead to more effective support that addresses root causes and also respects the individuality of each person's mental health journey, such as supplements like magnesium, PEMF, neurofeedback and specific types of therapy.
Beyond Traditional Labels
Moving away from traditional pathological models of mental health to a neurodiversity framework can help in developing strategies that focus on strengths and coping mechanisms, rather than solely on eliminating symptoms. When we broaden our definition of neurodiversity, we move toward greater understanding and acceptance of neurodiverse conditions.
Community and Advocacy
This understanding fosters a sense of community among individuals with various mental health conditions. It also strengthens advocacy efforts for better resources, support systems, and public policies that accommodate neurodiverse individuals.
Does Having Multiple Forms of Neurodiverse Impact Treatment?
When an individual exhibits multiple forms of neurodiversity, such as having both OCD and being autistic, it can influence treatment approaches. Determining if it is mental illness vs neurodivergent can lead to better outcomes. Personalized treatment plans that consider the unique combination of challenges and strengths of each individual are crucial.
This might include tailored cognitive-behavioral therapy, specialized exposure and response prevention (ERP) techniques, neurofeedback, PEMF, parent groups and supportive environments that cater to their specific needs.
Final Words OCD and Neurodivergence
The discussion of OCD within the context of neurodiversity opens up new pathways for understanding and supporting individuals with this condition. Recognizing OCD as potentially part of the neurodivergent spectrum can help in developing more effective, empathetic, and personalized approaches to treatment, as well as understand how it affects the parent-child relationship.
For parents of children with OCD, embracing a neurodiversity perspective can provide a more inclusive and compassionate framework for supporting their child's unique brain and needs
Citations:
Chapman, R., & Botha, M. (2023). Neurodivergence-informed therapy. Developmental medicine and child neurology, 65(3), 310–317. https://doi.org/10.1111/dmcn.15384
Heasman, B., & Gillespie, A. (2019). Neurodivergent intersubjectivity: Distinctive features of how autistic people create shared understanding. Autism : the international journal of research and practice, 23(4), 910–921. https://doi.org/10.1177/1362361318785172
Kornblau, B. L., & Robertson, S. M. (2021). Special Issue on Occupational Therapy With Neurodivergent People. The American journal of occupational therapy : official publication of the American Occupational Therapy Association, 75(3), 7503170010. https://doi.org/10.5014/ajot.2021.753001
Mellifont, D. (2021). A Qualitative Study Exploring Neurodiversity Conference Themes, Representations, and Evidence-Based Justifications for the Explicit Inclusion and Valuing of OCD. The International Journal of Information, Diversity, & Inclusion, 5(2), 111–138. https://www.jstor.org/stable/48645276
Dr. Roseann is an OCD mental health expert who frequently is in the media:
- Insider: What is OCD?
- Single Care Controlling the uncontrollable: Living with OCD during a pandemic
- MomsCove How to Help a Child with Anxiety and OCD
- Holistic Counseling Podcast: Effective Treatments for OCD
- Epidemic Answers: Neurofeedback for ADHD, anxiety, OCD and mood
- BCIA: Calming the OCD Brain with Neurofeedback and ERP Therapy
- Integrative Practitioner: Integrative Approaches to Treating OCD
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023