When you have a child with OCD, you feel like your family life has been hijacked by an irrational tyrant. It is because that is what OCD does.
Children and teens with OCD struggle mightily with intrusive thoughts and compulsions that take over their rational thinking and cause them to get caught in a fear cycle. And like most parents of a child with OCD, you accidentally get caught up in helping to soothe your child’s worries.
Often years go by before you get the right diagnosis and maybe even more years go by before the right help for your child. It is a scary place to be when you just want the right solutions. That is why understanding the signs and symptoms of OCD can help get your child on the right path.
What is Obsessive-Compulsive Disorder (OCD)?
An OCD diagnosis incorporates unreasonable thoughts and fears (obsessions) leading to compulsive behaviors. Children and adults with OCD engage in compulsive behaviors attempting to end the obsessions, decrease distress and anxiety, or stop perceived bad things from happening. They perform both mental and behavioral rituals to reduce feelings associated with anxiety disorder.
What is OCD Behavior?
OCD symptoms range in type and intensity. Fear of death, germ and contamination concerns, cleanliness fixations, religious over-observations (Scrupulosity), aggressive or sexual impulses, and symmetrical or organization obsessions are common. Children may also repeatedly ask questions and seek reassurance. Common compulsions include checking, washing/cleaning, and arranging.
If left untreated, OCD can be chronic and involve multiple obsessions and compulsions, ultimately interfering with schoolwork, family, or social activities.
Typical OCD onset occurs between ages 8 and 12. Despite OCD often being treatment resistant, early intervention is key to break the behavioral pattern. So, when you see obsessive-compulsive behaviors in your child, don’t wait to seek help from a psychotherapist who specializes in OCD treatment.
What are Obsessive Thoughts?
Obsessions are uncontrollable thoughts, images, impulses, and fears that kids with OCD can't stop thinking about. For example, they may fear that they or someone else will get sick, hurt, or die. Some commonly seen irrational fears include choking or vomiting while others present with perfectionist behaviors.
Children may realize their OCD intrusive thoughts don't make sense, but they can’t seem to stop them. The thoughts lead to uncomfortable feelings, such as anxiety, fear, disgust, or doubt.
Sometimes, children feel that things have to be executed in a way that is “just right.” Obsessions make it hard to concentrate, socialize, and participate in daily life. For some, obsessive thinking can be quite debilitating.
You also may notice that they have to repeat certain phrases or request you to repeat certain phrases in a certain way. They are also prone to a high rate of repetitive questioning that often reflect worry. Sometimes this type of behavior can start out subtle but then parents start to question the obsessive need for it.
What are Compulsions?
Compulsions are behaviors that kids with OCD feel compelled to do repeatedly. They are repetitive behaviors or thoughts that a person engages in to neutralize, counteract, or make their obsessions go away. So, things have to be clean, safe, in order, even, or just right.
OCD causes kids to feel they have to do rituals to do things in a certain way to make them feel less anxious. These children have to do things in a certain way and will start over if interrupted, which can be most observable in their play.
For kids (and adults) with OCD, rituals stop bad things from happening. Common rituals include washing and cleaning, erasing things, rewriting, redoing, or rereading, repeating a word, phrase, or question much more than necessary, counting, checking, touching or tapping.
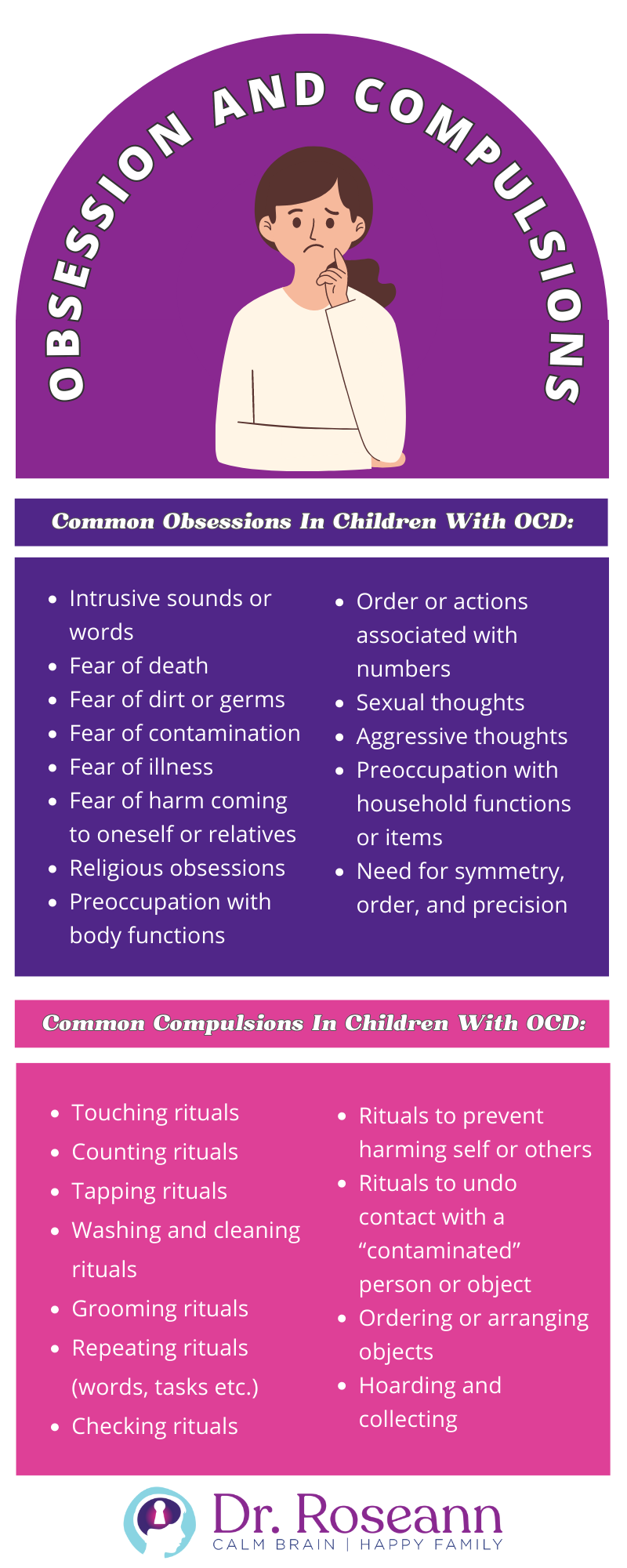
Common Obsessions In Children With OCD:
- Intrusive sounds or words
- Fear of death
- Fear of dirt or germs
- Fear of contamination
- Fear of illness
- Fear of harm coming to oneself or relatives
- Religious obsessions
- Preoccupation with body functions
- Order or actions associated with numbers
- Sexual thoughts
- Aggressive thoughts
- Preoccupation with household functions or items
- Need for symmetry, order, and precision
Common Compulsions In Children With OCD:
- Touching rituals
- Counting rituals
- Tapping rituals
- Washing and cleaning rituals
- Grooming rituals
- Repeating rituals (words, tasks etc.)
- Checking rituals
- Rituals to prevent harming self or others
- Rituals to undo contact with a “contaminated” person or object
- Ordering or arranging objects
- Hoarding and collecting
What are Signs of OCD in Children and Teens?
All children and adolescents have worries and negative thoughts at times, but children no matter what children with OCD try, they can't stop their disturbing thoughts, images, and urges, no matter what they try. They experience intrusive, unwanted thoughts.
Early signs of obsessive thinking or compulsive behaviors may be more subtle in children. In very young children, OCD behaviors can appear, but go unnoticed since they lack the communication skills to express their feelings. Instead, what you see is our behaviors that reflect compulsions and obsessions.
For example, children may display rigid bedtime rituals such as having to do the same behavior routinely or make a parent have to repeat a phrase every night for they get distressed. I recall one girl who made her parents go through an elaborate morning routine in order for her to eat and get on the bus. Her parents believed that if they didn’t participate, then she wouldn’t eat.
For most children, OCD related behaviors come on gradually, but for some, a sudden onset can occur. Whenever there is a sudden abnormal onset of OCD (or any mental health issue), PANS/PANDAS needs to be considered. PANS/PANDAS stems from an infectious trigger (such as Lyme or tick-borne Disease or strep throat) combined with environmental factors or other possible triggers that create a misdirected immune response resulting in a sudden onset of psychiatric symptoms.
Children with obsessive thoughts may show an excessive preoccupation with germs, dirt, illness, or with symmetry, order, and exactness. Additionally, they may focus on something bad happening or on aggressive thoughts and urges.
Compulsive behaviors may present as excessive hand washing or showering, repeated checking, counting, preoccupation with sequencing or grouping objects, or repeatedly and excessively asking the same questions, repeating words spoken by self or others or sounds.
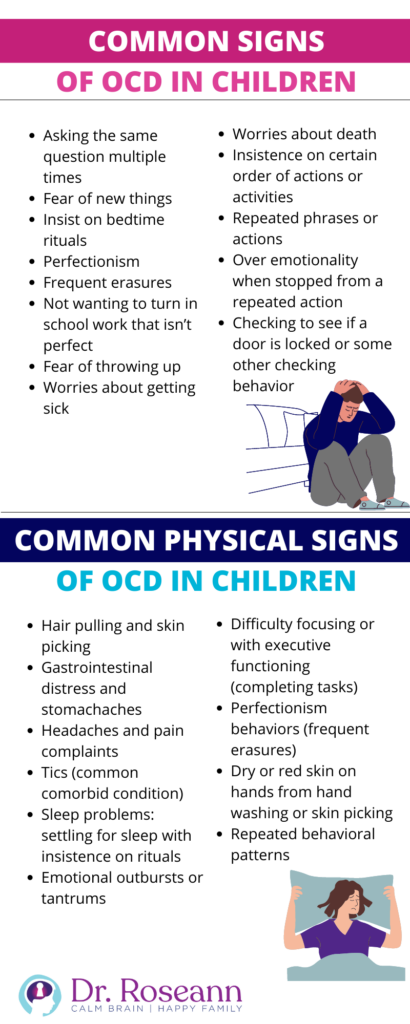
Common Signs of OCD in Children
- Asking the same question multiple times
- Fear of new things
- Insist on bedtime rituals
- Perfectionism
- Frequent erasures
- Not wanting to turn in school work that isn’t perfect
- Fear of throwing up
- Worries about getting sick
- Worries about death
- Insistence on certain order of actions or activities
- Repeated phrases or actions
- Over emotionality when stopped from a repeated action
- Checking to see if a door is locked or some other checking behavior
Common Physical Signs of OCD in Children
- Hair pulling and skin picking
- Gastrointestinal distress and stomachaches
- Headaches and pain complaints
- Tics (common comorbid condition)
- Sleep problems: settling for sleep with insistence on rituals
- Emotional outbursts or tantrums
- Difficulty focusing or with executive functioning (completing tasks)
- Perfectionism behaviors (frequent erasures)
- Dry or red skin on hands from hand washing or skin picking
- Repeated behavioral patterns
What Causes OCD in a Child?
There are many reasons why one develops obsessions and compulsions but for most the nexus starts with anxiety that morphs into an irrational fear. OCD is all about the belief that if they do x, y, or z, then the bad thing won’t happen. Their fear doesn't have to make sense and usually doesn’t.
Having a first degree relative, tic disorder, another clinical condition, a strep infection, or PANS/PANDAS puts you at a greater risk than if you don’t have these factors.
What Factors Influence a Child’s OCD?
At our Ridgefield, CT center we support preschoolers to young adults with OCD all over the world. There are many reasons why children can do well with OCD treatment especially when they have a family who is willing and able to take on obsessions and compulsions head on. The right attitude will win every time over a complex problem!
It is a parent’s belief that the child will overcome their OCD and willingness to tackle it that is the greatest determinant of treatment success.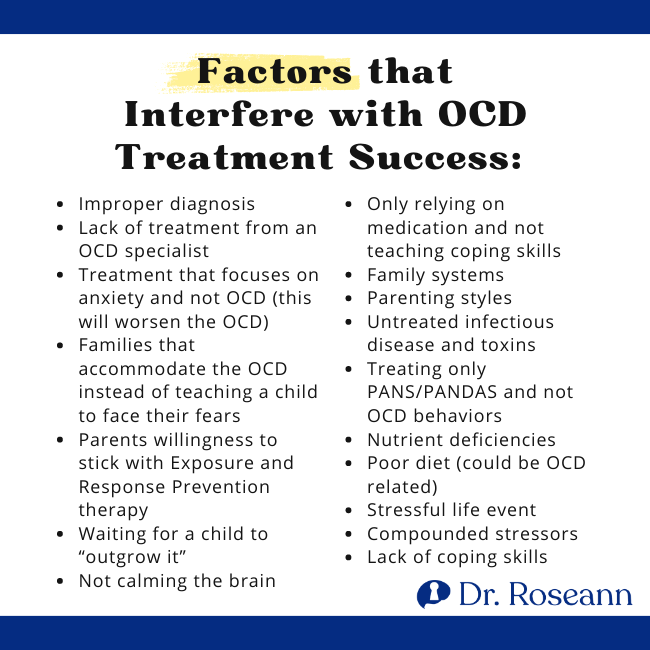
Factors that Interfere with OCD Treatment Success:
- Improper diagnosis
- Lack of treatment from an OCD specialist
- Treatment that focuses on anxiety and not OCD (this will worsen the OCD)
- Families that accommodate the OCD instead of teaching a child to face their fears
- Parents willingness to stick with Exposure and Response Prevention therapy
- Waiting for a child to “outgrow it”
- Not calming the brain
- Only relying on medication and not teaching coping skills
- Family systems
- Parenting styles
- Untreated infectious disease and toxins
- Treating only PANS/PANDAS and not OCD behaviors
- Nutrient deficiencies
- Poor diet (could be OCD related)
- Stressful life event
- Compounded stressors
- Lack of coping skills
How is OCD Diagnosed?
Through the clinical interview process, OCD is diagnosed by a mental health professional. During intake, the clinician is trained to assess whether obsessive or compulsive behaviors are present as well as their impact on that child's or individual's life and functioning. An OCD specialist will use the diagnostic and statistical manual to see if a child meets the clinical criteria for a diagnosis.
For diagnosis, these behaviors have to have a significant impact on daily functioning, occupy a lot of time (typically more than one hour per day), and cause distress. No specific psychological or laboratory OCD test exists which often causes frustration.
Can my Child Outgrow OCD?
Children don't outgrow OCD; rather, they learn to overcome it through the use of therapy and a variety of treatments. Symptoms can increase during periods of stress, as well as hormone and developmental change.
There can also be a waxing and waning of symptoms, which can confuse parents but it often is part of the disorder. Getting support early in a child's life is key to successfully managing obsessions and compulsions.
Are OCD and Autism Related?
A high rate of individuals with Autism also have OCD. According to a Danish study of more than 850,000 people, compared with their typical peers, people with Autism are twice as likely to receive a diagnosis of OCD and people with OCD are four times as likely also to have Autism.
The Danish study also found that there is a connection between OCD and Autism at the genetic level. They found that when at least one parent had OCD, their offspring had a higher risk of Autism.
Similarities between OCD and Autism include reliance on repetitive behaviors to calm anxiety, which suggests a genetic overlap. For example, autistics display stimming behaviors (hand flapping) and children with OCD display rituals and compulsions which both fulfill the same emotional need. However, as children with Autism always have social issues and social communication issues, children with OCD do not always have these, differentiating the two diagnoses.
What is OCD Treatment?
OCD is treated using a variety of traditional and holistic therapies. Some people benefit from medication, and others don't. A consistently proven effective treatment for OCD is Cognitive Behavioral Therapy (CBT) and Exposure Therapy (and more specifically Response and Prevention Therapy (E/RP).
Holistic therapies, such as Neurofeedback, Biofeedback, Reiki, EFT/Tapping, and massage can also be good adjunctive therapies to help align the nervous system. Before a person can fully move forward in clinical therapy, they need to get the Central Nervous System (CNS) regulated.
How Does CBT and Exposure (ERP) Therapy Help OCD?
Cognitive Behavioral Therapy (CBT) is a type of psychotherapy that works at the conscious level. CBT presumes that how individuals perceive a situation is more connected to their reaction than to the situation itself thus working through those misperceptions brings relief. CBT combines talk and behavioral therapy to reframe negative thinking patterns into positive thoughts. Research has found CBT to be more effective than medication in reducing symptoms (59.9 % vs. 33.4%) and widely considered to be the first line of treatment in OCD.
Exposure Therapy, a type of CBT, specifically called Response and Prevention Therapy (ER/P), exposes the person to their trigger so they learn how to be uncomfortable to the point where they can ignore their trigger.
First, the person identifies all the triggers. Next, the therapist exposes the person to the situations that trigger his or her obsessions and compulsions (sometimes starting gradually and other times addressing more moderate triggers).
The therapy emphasizes learning how to deal with the uncomfortableness rather than avoiding it, as the latter leads to negative reinforcement. Patients learn that with exposure, their anxiety increases, but it also decreases.
Over time, through psychoeducation and cognitive behavioral therapy, the person's response to triggers changes, leading to a decrease in the frequency of compulsions and the intensity of obsessions. OCD treatment and anxiety expert, Kimberly Morrow, LCSW explains “We have to teach clients that they are “feeding the dog” with negative thinking and they have to understand that OCD is a bully that they can overcome”.
Therapeutic exposures repeated over time decrease associated anxiety because the individual learns that nothing bad happens when they stop performing rituals. They can stop OCD from bullying them.
Cognitive restructuring is part of the process, so they learn to evaluate perceived threats associated with each obsession and then test limits. Upon completion of ER/P therapy, the OCD symptoms often diminish or disappear.
How is Pediatric OCD Treatment Different From Adult OCD Treatment?
Treatment for children and adolescents with OCD isn't that different from adult OCD treatment. What is different is that the brain of an adult with OCD has habituated much longer than that of child. That means that there is a stronger subconscious behavioral component for adults simply because the behavior has been there longer.
That doesn't mean that the obsessions and compulsions found in adults vs children are any less treatable, rather, it means that they are habits that will take longer and more effort to break. With OCD, it is all about talking back to that OCD and showing it who is boss.
Kids are more willing and open to getting rid of their “habit” (the negative reinforcement cycle) because it hasn't been there as ong. In addition, kids are more willing to push themselves in new learning areas because they do that everyday at school.
How Does OCD Impact School?
Obsessions and compulsions can interfere with learning and processing in a variety of ways. Typically, these children display slow processing and perfectionistic tendencies. They also can display difficulties with focus because they are often performing mental rituals. Finally, children may display OCD as increased emotionality or rigidity.
Although signs and symptoms may be obvious, most are more subtle and misinterpreted as a focus, behavioral or processing problem. For those with sudden onset of OCD due to PANS/PANDAS, their behavior can change overnight and come on with such a frightening intensity. These children need immediate medical care from a PANS/PANDAS specialist.
How Can I Help My Child or Teen With OCD?
The best thing you can do is to get help early. Obsessions and compulsions often appear between ages 7 and 12 and shouldn’t be ignored because childhood-onset OCD isn’t a mental health disorder that just goes away. The longer they occur, the more behaviorally ingrained they become and therefore harder to break the “habit.”
Children can become habituated toward obsessive and compulsive behaviors as a way to cope with stress. Breaking those behaviors before they become ingrained can lessen the severity and, in some cases, stop the progression of OCD.
Even when treatment has not begun until obsessions and compulsions have become more ingrained and debilitating, forms of treatments, including exposure therapy (ERP), PEMF, and neurofeedback can help. You have to calm the brain and treat the behaviors and that is exactly with we do in our program
Parent psychoeducation and participation in the ERP therapy sessions and process is critical for supporting a child with OCD. Parents need to help with the exposure process by not allowing a child to suppress the obsessions and compulsions and instead learn to tolerate them. This process helps to lessen, if not extinguish, obsessions and compulsions.
Calling a therapist who is trained to do ERP is an important step to getting your child help. You can find a therapist through the International OCD Foundation (IOCDF) or apply to work with us at www.drroseann.com/apply
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.