Having a child with emotional and behavioral challenges can be exhausting and bewildering. You may see a hair trigger temper over seemingly nothing or “big” emotional reactions. It's common for parents to hear terms like Disruptive Mood Dysregulation Disorder (DMDD) and Oppositional Defiant Disorder (ODD) thrown around, but these concepts leave them with more questions than answers.
For those parents that seek out support from me through my Self Regulation Mastery Blueprint or one-to-one program, they all want to understand why this is happening and what to do about it. Calming the nervous system and gaining coping skills are key in breaking this reactive cycle.
Let’s shed light on these disorders' characteristics and possible diagnoses and dig into self-regulation tips to offer clarity and support to parents.
What is DMDD?
Disruptive Mood Dysregulation Disorder (DMDD) is a relatively new diagnosis that was introduced in the DSM-5 to address the needs of children who exhibit severe, recurrent temper outbursts. These outbursts are always out of proportion to the situation at hand.
Children with DMDD often experience persistent irritability and frequent episodes of explosive rage. These aren’t typical tantrums because they last for long periods of time, occur at a high frequency and the child takes a long time to recover. It's important to note that these symptoms must be present for at least 12 months and occur in more than one setting to meet the criteria for DMDD diagnosis.
What is ODD?
Oppositional Defiant Disorder (ODD) is a behavioral disorder observed in children and adolescents, characterized by a persistent pattern of angry, argumentative, and defiant behavior. Children with ODD often display frequent temper tantrums, refusal to comply with rules or requests, and a tendency to annoy others deliberately.
This behavior can significantly impact their relationships with family members, peers, and authority figures and their academic and social functioning. Differentiating ODD from typical childhood defiance is crucial, as the symptoms of ODD are more severe, persistent, and disruptive to daily life.
Disruptive Mood Dysregulation Disorder vs ODD
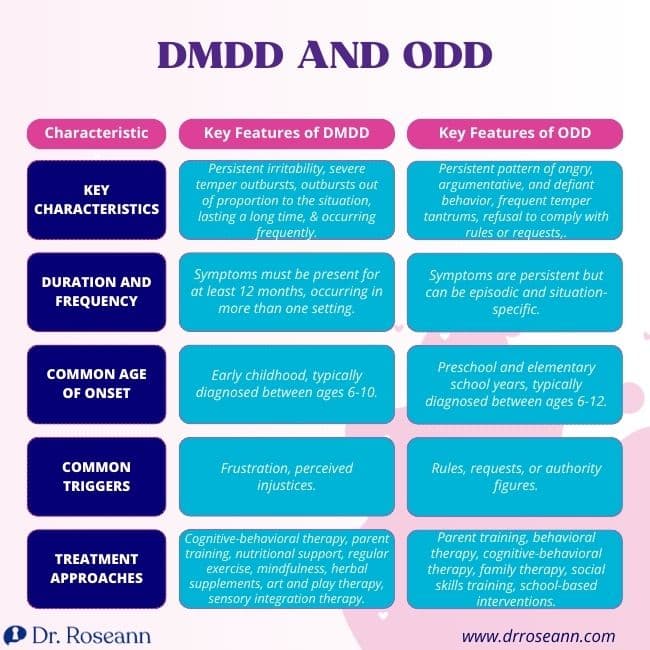
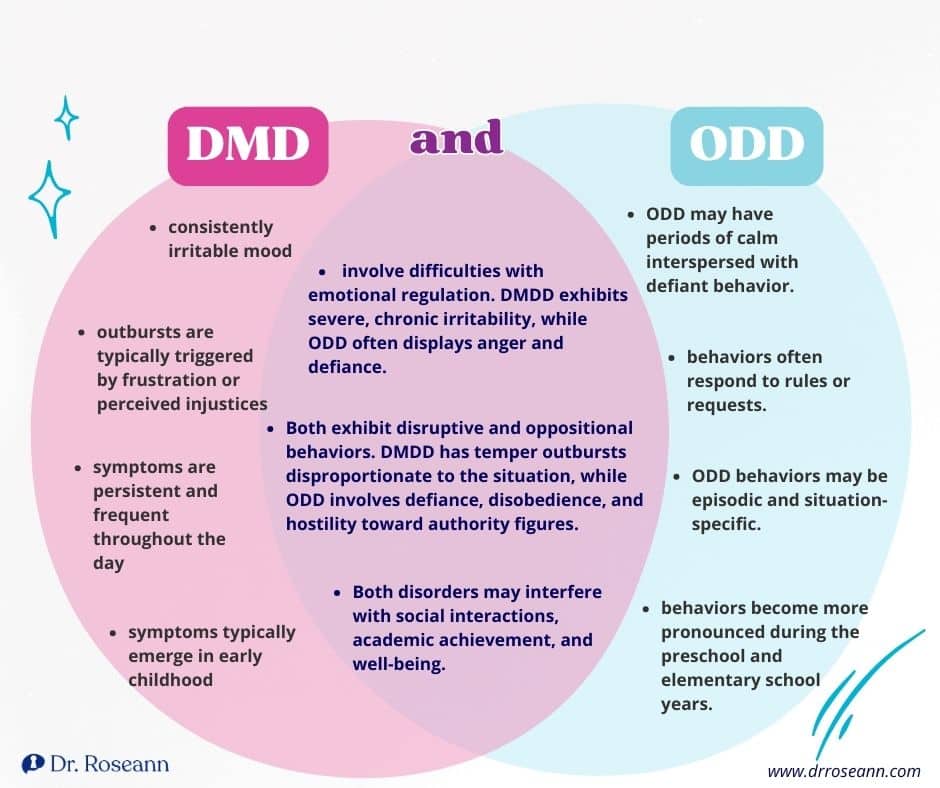
DMDD and ODD share some similarities, but they also have distinct differences. While both disorders involve difficulties with emotional regulation and oppositional behavior, DMDD is characterized by severe, chronic irritability and temper outbursts. In contrast, ODD primarily involves defiance and hostility toward authority figures.
Similarities of DMDD and ODD
- Emotional Dysregulation: DMDD and ODD involve difficulties with emotional regulation. Children with DMDD experience severe, chronic irritability, while those with ODD often display anger and defiance.
- Behavioral Challenges: Children with DMDD and ODD may exhibit disruptive and oppositional behaviors. While DMDD is characterized by temper outbursts disproportionate to the situation, ODD involves defiance, disobedience, and hostility toward authority figures.
- Impact on Functioning: DMDD and ODD can significantly impair children's functioning in various domains of life. Both disorders may interfere with social interactions, academic achievement, and well-being. Children with DMDD and ODD may struggle to follow rules and routines.
Key Differences DMDD vs ODD
There are differences between Disruptive Mood Dysregulation Disorder and Oppositional Defiant Disorder.
- Temperament: Children with DMDD often display a consistently irritable mood, while those with ODD may have periods of calm interspersed with defiant behavior.
- Triggers: DMDD outbursts are typically triggered by frustration or perceived injustices, whereas ODD behaviors may arise in response to rules or requests.
- Duration and Frequency: DMDD symptoms are persistent and occur frequently throughout the day, whereas ODD behaviors may be episodic and situation-specific.
- Age of Onset: DMDD symptoms typically emerge in early childhood, while ODD behaviors may become more pronounced during the preschool and elementary school years.
How to Treat DMDD without Medication

If you suspect that your child may have DMDD or ODD, it's essential to seek evaluation from a qualified mental health professional. A thorough assessment will gather information from parents, teachers, and other caregivers to determine the most appropriate diagnosis and treatment plan. Managing DMDD often requires a multifaceted approach that may include:
1. Cognitive-Behavioral Therapy
Cognitive-behavioral therapy (CBT) and parent-child interaction therapy (PCIT) can help children learn to regulate emotions and improve their coping skills. In a case study, a 9-year-old girl with DMDD, ADHD, and anxiety got better with CBT. She had therapy sessions for 12 weeks and then some follow-up sessions. After therapy, she showed fewer angry outbursts and aggressive behavior (Tudor et al., 2016).
2. Parent Training and Behavioral Therapy
Parent Training programs provide parents with valuable tools and strategies to navigate the complexities of raising a child with emotional and behavioral challenges. Through these programs, parents learn evidence-based techniques for fostering their child's emotional development and effectively managing challenging behaviors.
There should be a focus on behavioral support and training parents on how to manage the behaviors. Having spent the bulk of my three decades showing parents on how to manage behaviors, I know just how valuable therapist intervention can be. In my Self Regulation Mastery Blueprint, we give parents how-to’s and scripts showing them just how to manage dysregulated behaviors.
3. Nutritional Support
A balanced diet rich in nutrients such as omega-3 fatty acids, magnesium, and zinc may help support mood regulation and reduce irritability. Encourage consumption of foods like fatty fish, nuts, seeds, leafy greens, and whole grains. Consider consulting with a registered dietitian for personalized dietary recommendations.
4. Regular Exercise
Physical activity can help reduce stress, improve mood, and promote overall health. Encourage your child to exercise regularly through team sports, outdoor play, or structured activities like yoga or martial arts.
5. Mindfulness and Relaxation Techniques
Teaching children mindfulness techniques such as deep breathing, meditation, and progressive muscle relaxation can help them learn to manage stress and regulate their emotions more effectively. These practices can be incorporated into daily routines and bedtime rituals.
6. Herbal Supplements
Some herbal supplements, such as passionflower, chamomile, and valerian root, have calming properties and may help reduce anxiety and irritability. However, it's essential to consult with a healthcare professional before introducing any herbal remedies, especially in children, as they may interact with medications or have side effects.
7. Art and Play Therapy
Creative therapies such as art and play therapy can provide children with alternative outlets for expressing emotions and processing difficult experiences. Engaging in creative activities can promote self-expression, problem-solving skills, and emotional resilience.
8. Sensory Integration Therapy
For children who struggle with sensory processing difficulties, sensory integration therapy can help regulate their responses to sensory stimuli and improve self-regulation. This therapy typically involves structured activities designed to stimulate different sensory systems.
One study examined how kids with DMDD deal with sensory stuff like sounds and touch. They found that more than half of the kids with DMDD had trouble with sensory things, compared to about a third of other kids they looked at. Kids with DMDD might encounter challenges with loud noises or certain textures (Benarous et al., 2020).
Supporting Your Child and Yourself
Parenting a child with DMDD or ODD can be emotionally taxing, but it's essential to prioritize self-care and seek support when needed. Connecting with other parents facing similar challenges can provide validation and practical advice for managing day-to-day struggles.
If you’re looking for lasting solutions to help manage your child's impulsivity, flares, mood swings, and dysregulation without getting triggered or resorting to medication, download the Natural Mood And Behavior Regulation Kit.
What is DMDD diagnosis?
Disruptive Mood Dysregulation Disorder (DMDD) is diagnosed based on specific criteria outlined in the DSM-5, including severe recurrent temper outbursts, persistently irritable or angry mood, and symptoms that occur in multiple settings.
What is DMDD in children?
Disruptive Mood Dysregulation Disorder (DMDD) in children is a mental health condition characterized by severe, recurrent temper outbursts that are out of proportion to the situation, as well as persistently irritable or angry mood between outbursts. It typically emerges in childhood and can significantly impair a child's functioning in various areas of life, including home, school, and relationships.
What causes DMDD?
The exact cause of Disruptive Mood Dysregulation Disorder (DMDD) is not fully understood, but it's believed to result from a combination of genetic, biological, and environmental factors. These may include a family history of mood disorders, abnormalities in brain structure or function, and exposure to early-life stress or trauma.
Can adults have DMDD?
Disruptive Mood Dysregulation Disorder (DMDD) is primarily diagnosed in children and adolescents, typically between the ages of 6 and 18 years old. However, adults can experience symptoms similar to those seen in DMDD, such as chronic irritability and difficulty regulating emotions. In adults, these symptoms may be diagnosed and treated as other mental health conditions, such as mood disorders or personality disorders, rather than DMDD specifically.
What does DMDD turn into in adults?
There isn't enough research to definitively state what Disruptive Mood Dysregulation Disorder (DMDD) may develop into in adulthood. However, some studies suggest that children with DMDD may be at increased risk for developing mood disorders such as depression or anxiety disorders later in life. Regular monitoring and appropriate interventions can help mitigate potential long-term effects.
How to discipline a child with DMDD?
Disciplining a child with Disruptive Mood Dysregulation Disorder (DMDD) requires a patient and consistent approach. Set clear expectations, offer positive reinforcement for good behavior, and provide support and guidance in developing coping skills. Professional help may also be beneficial in tailoring strategies to meet the child's specific needs.
Can DMDD and ODD be diagnosed together?
Yes, DMDD and ODD can co-occur and be diagnosed together in the same individual. While they have distinct diagnostic criteria, some children may exhibit symptoms that meet the criteria for both disorders. A comprehensive assessment by a qualified mental health professional is essential to diagnose and address the individual's needs accurately.
Is ODD hereditary?
There is evidence to suggest that ODD may have a genetic component, meaning it can run in families. Children with a family history of ODD or other mental health conditions may be at increased risk of developing the disorder themselves. However, environmental factors and parenting styles also play significant roles in the development of ODD.
Is ODD learned or genetic?
ODD can have both genetic and environmental influences. While there may be a genetic predisposition to ODD, meaning it can run in families, environmental factors such as parenting styles, family dynamics, and exposure to stress or trauma can also contribute to the development of ODD. It's often a combination of genetic vulnerability and environmental factors that influence the onset and expression of ODD in children.
Can you outgrow bipolar disorder?
While some individuals may experience periods of symptom remission or stability, bipolar disorder typically requires ongoing management and treatment. With appropriate interventions, including medication, therapy, and lifestyle changes, many people with bipolar disorder can effectively manage their symptoms and lead fulfilling lives. However, it is not typically something that can be “outgrown” in the same way that some childhood disorders might be.
Can you be diagnosed with bipolar under 18?
Yes, it is possible to be diagnosed with bipolar disorder before the age of 18. While the onset of bipolar disorder often occurs in late adolescence or early adulthood, it can manifest in children and teenagers as well.
What does defiant mean?
Defiant refers to resisting or disobeying authority figures or rules. Defiant people may openly challenge or refuse to comply with instructions, regulations, or expectations. This behavior can manifest as opposition, rebellion, or refusal to follow orders or conform to societal norms.
What is dysregulation?
Dysregulation refers to the inability to regulate or control specific processes or functions correctly. In mental health, dysregulation often relates to difficulties in regulating emotions, behaviors, or physiological responses.
Citations
Benarous, X., Bury, V., Lahaye, H., Desrosiers, L., Cohen, D., & Guilé, J. M. (2020). Sensory Processing Difficulties in Youths With Disruptive Mood Dysregulation Disorder. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00164
Tudor, M. E., Ibrahim, K., Bertschinger, E., Piasecka, J., & Sukhodolsky, D. G. (2016). Cognitive-Behavioral Therapy for a 9-Year-Old Girl With Disruptive Mood Dysregulation Disorder. Clinical Case Studies, 15(6), 459–475. https://doi.org/10.1177/1534650116669431
Dr. Roseann is a mental health expert in Self-Regulation who frequently is in the media:
- Healthline Understanding Self-Regulation Skills
- Scary Mommy What Is Self-Regulation In Children, And How Can You Help Improve It?
- The Warrior Parent Podcast It's Gonna Be OK! Changing Behaviors and Responses (And The Magic of Magnesium)In Your Family with Dr. Roseann Capanna-Hodge
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024










