Pathological Demand Avoidance (PDA) is a lesser-known yet crucial aspect of the autism spectrum. To understand PDA, parents have to move beyond the commonly observed behaviors of refusal and resistance and examine PDA traits such as heightened anxiety, sensory issues, and social challenges.
Learning more about PDA can be immensely beneficial for parents as it provides them with a deeper understanding of their child's behavior and challenges. Armed with this knowledge, parents can foster a more positive and accommodating relationship with their child
Characteristics and Signs of PDA
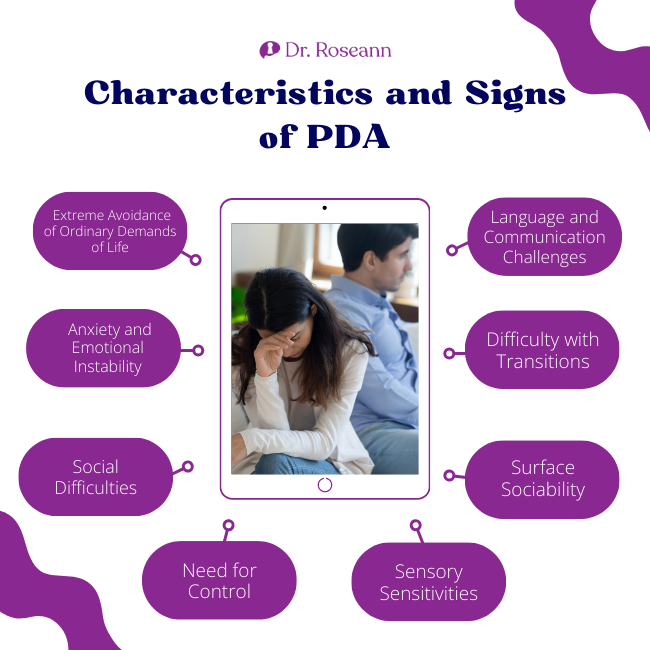
Pathological Demand Avoidance is characterized by a distinct set of behaviors and symptoms that go beyond the typical manifestations often associated with the profile of autism but can be a standalone issue too.
While each individual with PDA is unique, some common characteristics and symptoms may be observed:
1. Extreme Avoidance of Ordinary Demands of Life
Children with PDA exhibit an intense and pervasive avoidance of everyday demands. This avoidance is not merely a display of stubbornness. Instead, it represents an intense need to resist and avoid ordinary demands and escape social situations they perceive as challenging.
2. Anxiety and Emotional Instability
Heightened levels of anxiety are a hallmark of PDA, on top of resisting and avoiding the ordinary demands of life. Children may experience intense emotional responses, ranging from meltdowns to outbursts when faced with demands. Emotional instability is a key feature, and the anxiety associated with demands can be overwhelming.
3. Social Difficulties
Interpersonal relationships can be challenging for children with PDA. They may struggle with social cues, find it difficult to engage in reciprocal communication, and exhibit difficulties in forming and maintaining relationships with peers and family members.
4. Need for Control
Pervasive Developmental Disorder, or a pervasive need for control over their environment and routines, is a common trait in autistic people with PDA. This need for control is often linked to a deep-seated fear of unpredictability and an overwhelming desire to manage their surroundings.
5. Sensory Sensitivities
Sensory sensitivities are frequently observed in those with PDA. These sensitivities can manifest as heightened reactions to sensory stimuli, such as sounds, lights, textures, or smells, contributing to their overall discomfort in various environments.
6. Surface Sociability
While children with PDA may exhibit social behaviors, these are often described as “surface sociability.” They may engage in social interactions for strategic purposes, such as manipulating others to avoid demands or using social strategies to avoid demands rather than for genuine social interaction.
7. Difficulty with Transitions
Young people with PDA may struggle with transitions, whether they involve changes in routine, unexpected events, or shifts from one activity to another. Difficulty adapting to transitions can lead to increased stress and anxiety.
8. Language and Communication Challenges
Communication difficulties are common in individuals with PDA. This can include challenges in expressive and receptive language, as well as issues with understanding and using non-verbal communication cues.
Causes and Theories Behind PDA
Why does PDA rear its head? Theories abound, ranging from genetic predispositions to environmental factors. Elizabeth Newson's groundbreaking work paved the way as it emphasized the role of extreme demand avoidance (O’Nions, Christie, et al., 2013). Several theories offer insights into the potential origins of this neurodevelopmental condition:
Neurological Factors
PDA is often associated with atypical neurological functioning. Some researchers propose that there may be differences in the neural pathways and structures involved in emotional regulation, stress response, and executive functions. These neurological variations could contribute to the intense emotional reactions and difficulties in handling demands characteristic of PDA.
Genetic Influences
Genetic factors are thought to play a role in the development of PDA. Studies suggest a genetic predisposition, as individuals with a family history of Autism Spectrum Disorder (ASD) are more likely to exhibit traits associated with PDA (O’Nions et al., 2017). However, the genetic landscape of PDA autism is likely complex, involving multiple genes and gene-environment interactions.
Environmental Triggers
Environmental factors may contribute to the expression of PDA traits, particularly in individuals with a genetic predisposition. Adverse experiences during early development, such as trauma or chronic stress, could potentially influence the manifestation of demand avoidance behaviors. The interplay between genetic susceptibility and environmental factors is an area of ongoing investigation for pda mental health.
Cognitive and Behavioral Theories
Cognitive theories propose that individuals with PDA may have difficulty with certain cognitive processes, such as cognitive inflexibility (Goodson, 2018). These challenges can impact their ability to understand and respond appropriately to social cues and demands.
Behavioral theories highlight the role of reinforcement patterns, suggesting that avoidance behaviors may be reinforced over time due to their effectiveness in reducing perceived stress and anxiety (O’Nions et al., 2013).
Overlap with Other Conditions
PDA often coexists with other conditions within the autism spectrum, and the overlap of symptoms can complicate formal diagnosis and understanding. Some researchers explore whether PDA represents a distinct subtype within the broader spectrum or if it shares common features with other conditions.
Brain Functioning and Connectivity
Advances in neuroimaging techniques have allowed researchers to investigate the structural and functional connectivity of the brain in individuals with PDA. Differences in brain functioning, including areas associated with emotional processing and social cognition, are areas of interest in understanding the neural basis of PDA
The brain maps of those I see with demand avoidance often show slower brain wave activity in the areas associated with motivation.
How is a PDA Profile Recognized?
Diagnosing Pathological Demand Avoidance involves a comprehensive approach due to persistent demand avoidance. It starts with clinical observation of the child's behavior across various settings. Clinicians rely on a diagnostic interview and report from parents or caregivers, assessing communication skills and considering coexisting conditions within the autism spectrum.
The diagnostic process incorporates a thorough examination of adaptive functioning, including the ability to manage daily activities. Despite the absence of a specific diagnostic category for PDA in widely used manuals, clinicians utilize criteria from research and clinical guidelines. It often involves collaboration among psychologists, psychiatrists, speech therapists, and educators to ensure a holistic understanding of the individual's unique profile.
The aim is to identify persistent demand avoidance, extreme anxiety, social communication difficulties, and a need for complete control. This allows for the development of tailored interventions and support strategies for individuals grappling with the challenges of PDA and autism diagnosis.
Coping Mechanisms for Families and Caregivers
Navigating the challenges of living with and supporting individuals with Pathological Demand Avoidance can be emotionally taxing for families and caregivers. Implementing effective coping mechanisms is crucial for maintaining overall well-being. Here are coping strategies tailored for families and caregivers:
1. Education and Understanding
Invest time in learning about PDA, its characteristics, and how it manifests in daily life. Gaining a deep understanding of the condition can empower families and caregivers to navigate challenges more effectively.
2. Build a Support Network
Establish a support network by connecting with other families and caregivers who share similar experiences. Online forums, local support groups, or workshops can provide valuable insights, practical advice, and emotional support.
3. Open Communication
Foster open and honest communication within the family. Encourage family members to express their feelings, concerns, and experiences related to living with PDA. Open dialogue helps build a supportive and understanding environment.
4. Seek Professional Guidance
Pervasive Developmental Disorder, or a pervasive need for control over their environment and routines, is a common trait in autistic people with PDA. This need for control is often linked to a deep-seated fear of unpredictability and an overwhelming desire to manage their surroundings.
5. Respite Care
Arrange for respite care to provide caregivers with breaks when needed. Taking time for self-care is crucial for maintaining mental and emotional well-being, and respite care allows caregivers to recharge.
Prioritize self-care practices, including adequate sleep, healthy nutrition, and engaging in activities that bring joy and relaxation. Taking care of one's own physical and mental health is essential for sustained caregiving.
6. Flexible Planning
Embrace flexibility in planning and expectations. Recognize that each day may present different challenges, and having a flexible mindset helps in adapting to the dynamic nature of living with PDA. Clear boundaries can provide the necessary bumpers that make expectations explicit and cut down on friction.
7. Celebrate Small Victories
Acknowledge and celebrate small achievements and positive moments. Recognizing progress, no matter how small, reinforces a positive mindset and encourages older children with PDA, as well as their caregivers.
8. Mindfulness and Stress Reduction
Integrate mindfulness and stress reduction techniques into daily routines. Practices such as meditation, deep breathing exercises, or yoga can help manage stress and promote emotional well-being.
9. Advocate for Support Services
Advocate for necessary support services and accommodations in educational or community settings. Collaborate with professionals to ensure that the individual with PDA receives the appropriate resources and support.
10. Set Realistic Expectations
Establish realistic expectations for both the individual with PDA and the caregivers. Setting achievable goals helps in avoiding unnecessary stress and fosters a sense of accomplishment.
11. Promote Sibling Understanding
Facilitate discussions and activities that promote understanding among siblings. Educating siblings about PDA and involving them in support strategies can strengthen family bonds and encourage empathy.
12. Celebrate Diversity
Embrace the uniqueness of the individual with PDA. Celebrate their strengths and encourage their interests, fostering a positive and inclusive family environment.
Therapy and Interventions for People with PDA
Therapy and interventions for children with Pathological Demand Avoidance (PDA) are tailored to address the unique challenges associated with this neurodevelopmental condition. A multidisciplinary approach is often employed, involving various professionals to provide comprehensive support. Here, we explore the expanded landscape of therapeutic strategies and interventions for children with PDA:
Applied Behavior Analysis (ABA)
ABA is commonly utilized to address specific behaviors associated with PDA. This behavioral therapy focuses on understanding and modifying behaviors through positive reinforcement, shaping, and systematic desensitization. ABA can be adapted to the individual needs of children with PDA. It emphasizes flexibility and a person-centered approach.
Occupational Therapy (OT)
Occupational therapists work with children with PDA to enhance their daily living skills, sensory processing, and self-regulation. OT interventions may include sensory integration activities, fine and gross motor skill development, and strategies to improve adaptive behaviors for more effective engagement in daily activities.
Speech and Language Therapy
Speech and language therapists play a crucial role in addressing communication difficulties often associated with PDA. Therapy may focus on improving expressive and receptive language skills, social communication, and pragmatic language use. Visual supports and alternative communication methods may also be incorporated.
Cognitive Behavioral Therapy (CBT)
CBT is employed to address anxiety and emotional regulation in children with PDA. Therapists work collaboratively with the child to identify and challenge negative thought patterns, develop coping mechanisms, and enhance problem-solving skills. CBT aims to reduce anxiety-related avoidance behaviors.
Social Skills Training
Social skills training interventions target the challenges children with PDA may face in social interactions. Therapists guide children in understanding social cues, navigating relationships, and practicing appropriate social behaviors. They make kids comfortable in role play and pretending so as to enhance practical application.
Parent-Child Interaction Therapy (PCIT)
PCIT involves both parents and children in therapy sessions to focus on improving the parent-child relationship and enhancing parenting skills. Therapists guide effective communication, behavior management, and strategies to promote positive interactions within the family dynamic.
Individualized Education Plans (IEPs) in School Settings
Collaborative efforts with educators are essential to create individualized education plans that address the unique learning needs of children with PDA. IEP and 504 accommodations such as modified schedules, sensory-friendly environments, and personalized approaches to academic and social challenges may be incorporated.
Play Therapy
Play therapy offers a non-directive and expressive approach to help children with PDA communicate and process emotions. Therapists engage children in play activities, providing a safe space for expression, creativity, and the development of coping skills.
Neurofeedback
Studies in related autism spectrum disorders suggest that neurofeedback may enhance emotional regulation, attention, and executive functioning by targeting specific brain regions (Coben et al., 2009).
Through real-time feedback on brain activity, neurofeedback offers an individualized approach to address one's unique neurobiological PDA profile, potentially contributing to improved adaptive functioning.
PEMF
Pulsed Electromagnetic Field (PEMF) therapy is an alternative approach that has been explored for various health conditions, including PDA and autism. Studies and anecdotal reports suggest that PEMF therapy may have potential benefits for individuals with autism, including improvements in social behaviors, communication skills, and sensory processing (Harman, 2019).
Magnesium Supplement
Individuals with autism spectrum disorders, including PDA, may have varying nutritional needs, and some studies have explored the potential benefits of certain supplements, including magnesium (Strambi et al., 2006).
Magnesium supplementation provides a calming effect and could potentially help with certain symptoms associated with autism, such as anxiety and sleep disturbances. However, individual responses to magnesium supplementation can vary, and its use should be approached cautiously.
The BrainBehaviorResetTM Program is intricately designed to address the distinctive challenges encountered by children with PDA, presenting a holistic framework that integrates neuroscience, behavioral science, and tailored interventions. And as a PDA psychologist, myself and our team understands how pathological demand avoidance impacts a child and family.
This transformative program identifies the nuanced behaviors linked to PDA and also equips parents and caregivers with pragmatic tools to guide their autistic children toward a more adaptive and fulfilling trajectory.
Parent Action Steps
☐ Dive deep into the intricacies of the Pathological Demand Avoidance syndrome.
☐ Spot excessive mood swings, sensory overload, panic attacks, and high anxiety.
☐ Join support groups, like the National Autistic Society or our CALM Brain Community, which can be a great resource.
☐ Consult professionals and use the Extreme Demand Avoidance Questionnaire (EDA) or a PDA checklist.
☐ Integrate role play, sensory adjustments, and overload recognition into your child’s life.
☐ Seek tailored therapies with professionals to support your child's emotional level.
☐ Nourish humor, understanding, and the best approach for you and the whole family.
☐ Communicate openly with schools and ensure they support your child's learning.
☐ Recognize and celebrate each small victory as progress is the journey's sweet reward.
☐ Use our Solution Matcher to get personalized treatment for your child.
Citations
Coben, R., Linden, M., & Myers, T. E. (2009). Neurofeedback for Autistic Spectrum Disorder: A Review of the Literature. Applied Psychophysiology and Biofeedback, 35(1), 83–105. https://doi.org/10.1007/s10484-009-9117-y
Goodson, A. (2018, October 10). Emotion Regulation and Executive Function in Children and Adolescents with Autism Spectrum Disorder and Pathological Demand Avoidance Traits. Discovery.ucl.ac.uk. https://discovery.ucl.ac.uk/id/eprint/10057420/
Harman, J. (2019). Treating Autism Spectrum Disorder Using Pulsed EMF Therapy: A Case Series Report peer-review by editorial board of Asia Pacific Journal of Neuro therapy (APJNT). Asia Pacific Journal of Neurotherapy (APJNT), 1(2), 21-026. https://apjnt.org/wp-content/uploads/2019/12/Joe_Harman_APJNT_Journal_Vol1_No2_2019.pdf
O’Nions, E., Christie, P., Gould, J., Viding, E., & Happé, F. (2013). Development of the “Extreme Demand Avoidance Questionnaire” (EDA-Q): preliminary observations on a trait measure for Pathological Demand Avoidance. Journal of Child Psychology and Psychiatry, 55(7), 758–768. https://doi.org/10.1111/jcpp.12149
O’Nions, E., Viding, E., Floyd, C., Quinlan, E., Pidgeon, C., Gould, J., & Happé, F. (2017). Dimensions of difficulty in children reported to have an autism spectrum diagnosis and features of extreme/“pathological” demand avoidance. Child and Adolescent Mental Health, 23(3), 220–227. https://doi.org/10.1111/camh.12242
O’Nions, E., Viding, E., Greven, C. U., Ronald, A., & Happé, F. (2013). Pathological demand avoidance: Exploring the behavioural profile. Autism, 18(5), 538–544. https://doi.org/10.1177/1362361313481861
Strambi, M., Mariangela Longini, Hayek, J., Berni, S., Macucci, F., Scalacci, E., & Piero Vezzosi. (2006). Magnesium Profile in Autism. Biological Trace Element Research, 109(2), 097-104. https://doi.org/10.1385/bter:109:2:097
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023