Obsessive-Compulsive Disorder (OCD) is a mental health condition where children, teens, and adults harbor obsessions or intrusive fears that cause them to do compulsive, ritualistic behaviors. Such compulsive acts are their responses to the obsessions they have.
In the minds of children and teens with OCD, doing these compulsions prevents the negative things they are afraid of from happening. The OCD brain forms a negative association between the behavior and the worry temporarily decreasing. The more the behavior happens, the more obsessions and compulsions occur because of this negative habituation.
In that way, these behaviors decrease their worries and feelings of distress, albeit temporarily. OCD manifests itself in different ways for every child or teen but at its core is a fear of worry actually happening and that is what drives their obsessive thinking and compulsions. .
Obsessions vs. Compulsions
Obsessions are thoughts that interrupt a person's life. It makes a person very upset or anxious to the point that they spend a considerable amount of time every day in obsessive thought to the point that they can no longer do their everyday tasks. Many people with OCD know that these obsessive thoughts aren't real. Even so, they still feel distressed about it, thinking that they could make it happen.
To counter these unwanted thoughts, individuals with OCD feel the urge to do something to reduce their anxiousness around these thoughts. These actions and behaviors become their compulsions. Compulsions are things that people with OCD do in response to their obsessions.
Most people with OCD feel that they must keep repeating these compulsions to make their anxiousness disappear, even if they don't like doing them and become rituals. As a result, they spend one or more hours a day doing repetitive things or having obsessive thoughts.
Individuals with OCD can carry out these compulsions for hours because doing so takes their minds off their anxieties and fears and their brain gets a negative reinforcement. However, all these obsessions, compulsions, and rituals only provide temporary relief. The obsessions and compulsions of a person with OCD are often completely illogical and don't have to have any basis in reality. That can be especially perplexing to family members who are desperate to help.
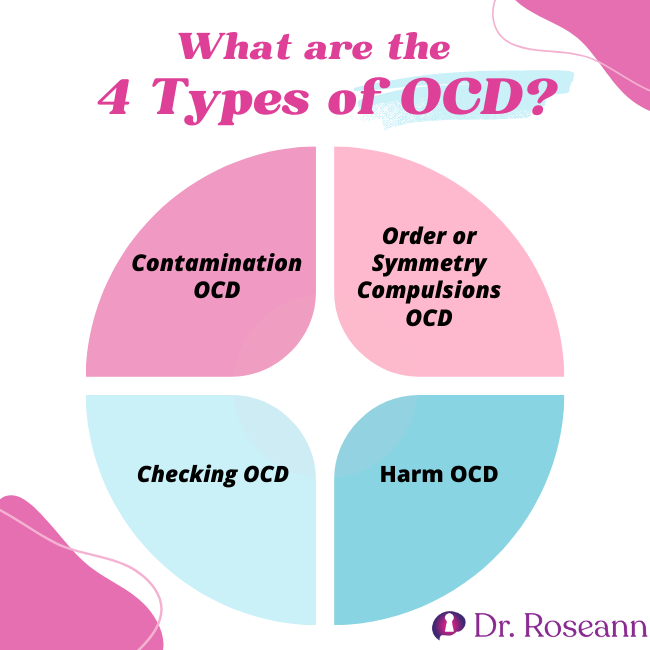
4 Most Common Types of OCD in Children
There are different types of OCD and it can be challenging to determine and diagnose each one. Parents should seek the help of a mental health practitioner if a family member shows any symptoms of OCD. This clinical disorder is often missed and confused with anxiety, which can cause a child's or teen's anxiety to get reinforced to a level that can make it even harder to treat.
A child or teen's OCD could be one of these four types:
#1 Contamination OCD
Children and teens who suffer from contamination OCD tend to exhibit decontamination compulsions in response to their contamination obsessions. For example, kids with contamination OCD may fear touching the ground, going outdoors, or getting their skin in contact with public objects.
If they end up feeling that something contaminated them, they will do a series of behaviors to alleviate their anxiety about being dirty, sick, or unclean. Their compulsions typically involve protecting themselves to avoid or remove the alleged physical and mental contamination.
I recently worked with a teen boy who was obsessed that his parents spit in his food and couldn't eat as a result. His eating became so restrictive that he lost a significant amount of weight and wasn't getting enough nutrients, which compounded his issues.
We were able to address his contamination fears while at the same time increasing his nutrient compensation to help calm his brain. A combination of PEMF with exposure and response therapy not only helped calm Jake's brain but gave his parents resources to not accommodate the OCD.
Common Contamination OCD Obsessions
Some examples of the common obsessions of people with this type of OCD are:
- Fear of contamination and contaminating others
- Fear of getting in contact with anything thought of as unclean
- Fear of germs
- Fear of being around sick people
- Fear of getting poisoned
Common Contamination OCD Compulsions
The usual compulsions of children and kids with this type of OCD are
- Excessive hand washing
- Repeated disinfection
- Frequent clothing changes
- Rigid cleaning and scrubbing
- Avoiding dirty areas or persons
These rituals and compulsions can really hijack a child's or adolescent's life. An OCD sufferer can wash their hands from 50 to 200 times daily, which can lead to physical pain. They may also take showers that last for hours.
The global COVID-19 pandemic was especially harsh for children and teens with OCD. Many sufferers experienced exacerbated OCD symptoms, while those in remission had a relapse. One study revealed that individuals with OCD have elevated obsessions and compulsions during the lockdown (Jalal et al., 2020).
#2 Order or Symmetry Compulsions OCD
Symmetry or order OCD refers to the need for perfect arrangement, order, or sameness. Children and teens with symmetry OCD experience what is referred to as “neurotic anxiety” or looping, intrusive thoughts if things don't feel or look right. They will also repeatedly think that something terrible will happen unless they perform their compulsions.
Children and teens with symmetry OCD will ensure that their environment is in perfect order. Clutter and disorganization make them anxious. Their need to constantly put things in order or symmetry may seem irrational, even to them. However, they can't seem to do anything about it. Research has shown that symmetry or ordering OCD is among the most frequent types among younger people (Jacobsen & Smith, 2017).
Common Symmetry OCD Obsessions
Children and teens with symmetry OCD may have the following unwanted obsessions:
- Overly concerned that something will happen if something is not in the proper order
- Feels anxious when things are asymmetrical
- Has an imperative need to achieve balance
Common Symmetry OCD Compulsions
The most common compulsions of children and teens with this form of OCD are the following:
- Lining up things
- Positioning items in perfect order
- Ordering or arranging items by size or color
- Repetitive behaviors related to visual checks
- Rewriting things
- Straightening up things
- Counting
#3 Checking OCD
Different people may show different symptoms of this type of OCD. These individuals don't trust their memory, so they keep checking the things around them. Sometimes, they even question these memories. One research studied how Checking OCD can cause memory distrust (Van den Hout & Kindt, 2003).
Children and teens with checking OCD display an exaggerated fear of being uncertain. As a result, they doubt their abilities to do everyday tasks and avoid social blunders. Because they are so unsure of themselves, they constantly fight intrusive thoughts of being careless or irresponsible.
Individuals with checking OCD also don't want to be blamed or scorned by others. As a result, they become overly conscientious, which feeds the OCD. But by being so, they become irrational and more susceptible to making the mistakes they dread.
They feel that they have to check things several times over or else, something terrible will happen. However, they also think they can never achieve perfection even after constantly checking. In the end, they get frustrated and are ashamed of their actions.
Many years ago I worked with a young woman who had to check septic and sewer caps because she feared she would fall in them. She knew it was completely irrational but yet she could no longer leave her house because of her checking behaviors.
Common Checking OCD Obsessions
Some of the significant fears of individuals with checking OCD are the following:
- Fear of starting a fire
- Fear of hitting people while driving
- Fear of inducing harm due to carelessness
- Fear of sending messages or emails with wrong content or inappropriate materials
- Fear of losing things
- Fear of leaving home unlocked
Common Checking OCD Compulsions
- Repeatedly checking that all home appliances are off
- Constantly ensuring that all window and door locks are working
- Always inspecting things closely
- Never-ending seeking of reassurance about their concerns
- Engages in mental rituals to go over things that they did and didn't do
- Repeatedly saying certain words or phrases
#4 Harm OCD
Suffers of this OCD subtype have unwanted intrusive thoughts about being aggressive or doing a violent act to themselves or another person. Children and kids suffering from harm OCD will have certain compulsions to make those violent thoughts go away.
Anybody can have violent thoughts and shrug them off. But for those with OCD, these thoughts worry them greatly. They believe that these thoughts have meaning or that they will enact them somehow.
For that reason, children and kids with harm OCD need reassurance that they will never act on their thoughts. It's the reason why they perform rituals or compulsions to reduce the anxiety associated with their violent thoughts.
Completing these ritualistic behaviors will make them feel less anxious, but only for a short while. They'll always do these compulsive behaviors every time the thought comes, making it an endless cycle of obsessions, fear, and doubt.
Kids with harm OCD related to self-harm are frequently miss diagnosed as suicidal. Many practitioners don't understand that they have a fear that they will harm themselves and don't actually want to or have a plan. I have worked with dozens of kids who were placed in a psychiatric facility where their OCD was missed.
Common Harm OCD Obsessions
For those with Harm OCD, the presence of the obsessions listed below are apparent.
- Getting violent mental thoughts and images and then worrying that they will act on them
- Thinks about inadvertently causing harm and never realizing it
- Terrified of hurting themselves or others on impulse
- Constant worrying about losing control and becoming a vicious person
Common Harm OCD Compulsions
The common compulsions of children and teens with Harm OCD are:
- Locking away sharp and pointed objects
- Reviewing one's every action to check if they caused harm
- Avoiding violent movies, TV shows, or news
- Excessive research of crimes online
- Compulsive praying and belief in spiritual items
- Always asking if they are capable of hurting themselves or others
OCD and Hoarding
Compulsive hoarding refers to a person's difficulty in discarding or throwing away possessions, especially ones of no value. Such behavior may affect one's physical, financial, and emotional health. Hoarding used to be a type of OCD, but it is now considered a separate condition, called hoarding disorder (Mataix‐Cols & Fernández de la Cruz, 2018).
The items that children and teens hoard keep them away from other people. Individuals with this mental health disorder commonly accumulate newspapers, pieces of clothing, magazines, boxes, plastic bags, and other odd items.
I once had a teen who hoarded food to the total dismay of her parents. It wasn't until they came to our center that we got to the bottom of her hoarding behavior.
Compulsive buying may also be related to hoarding, as well as the compulsive need to get free items. Individuals with hoarding disorder tend to have these compulsions:
- Buying items in multiple sets
- Keeping unnecessary things for fear that they'll need them in the future
- Collecting items that others consider worthless
- Storing too much of the same thing for fear of running out
Natural Solutions and Treatments for OCD
Exposure and Response Prevention Therapy is one of the best OCD treatment options. It is a combination of Exposure Therapy and CBT or Cognitive Behavior Therapy, which exposes the child or teen with OCD to trigger their feelings of discomfort until they can ignore them entirely. It is done in a very safe and systematic way under the care of a highly trained therapist.
Psychoeducation is a necessary part of the plan for the parent and child in order to overcome the behavioral habituation of the child and family. For the therapy to be effective, parents must know how OCD affects a child's brain and understand their behavior. The mental health practitioner helps identify the child's OCD triggers before gradual exposures that work to reduce and extinguish the behavior.
The emphasis of the therapy is to teach the child how to deal with the anxiety and discomfort they feel instead of avoiding them, which fuels negative reinforcement. The treatment may initially increase the child's anxiety but will eventually address it.
ERP therapy safely tests the limits of the child's fears. The mental healthcare provider will guide them and make them aware that those fears are irrational. The exposure experiences will show kids that they have nothing to be anxious about and effectively improve their quality of life without using medications with adverse side effects.
ERP is good news for parents with excessive concern about using mind-altering drugs on kids, especially during their developmental age. At our Ridgefield clinic and virtually, we help parents get an accurate diagnosis of OCD and related disorders and provide treatment to help every kid live a happy and normal life. We combine PEMF with ERP, especially with our PANS/PANDAS clients to calm the brain and teach kids how to talk back to OCD.
Citations
Jacobsen, A. M., & Smith, A. J. (2017). Symmetry and Ordering in Youth with Obsessive Compulsive Disorder. The Wiley Handbook of Obsessive Compulsive Disorders, 405–420. https://doi.org/10.1002/9781118890233.ch22
Jalal, B., Chamberlain, S. R., Robbins, T. W., & Sahakian, B. J. (2020). Obsessive–compulsive disorder—contamination fears, features, and treatment: novel smartphone therapies in light of global mental health and pandemics (COVID-19). CNS Spectrums, 1–9. https://doi.org/10.1017/s1092852920001947
Mataix‐Cols, D., & Fernández de la Cruz, L. (2018). Hoarding disorder has finally arrived, but many challenges lie ahead. World Psychiatry, 17(2), 224–225. https://doi.org/10.1002/wps.20531
Van den Hout, M., & Kindt, M. (2003). Repeated checking causes memory distrust. Behaviour Research and Therapy, 41(3), 301–316. https://doi.org/10.1016/s0005-7967(02)00012-8
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.