Understanding Somatic OCD is essential for parents of children and teens grappling with this challenging form of Obsessive Compulsive Disorder (OCD). This blog aims to provide a comprehensive overview of Somatic OCD, including its diagnosis, symptoms, and effective treatment options, with a particular emphasis on natural therapies.
What is Somatic OCD?
Somatic OCD, a distinct subtype of Obsessive Compulsive Disorder (OCD), manifests as an excessive and intrusive focus on the body's autonomic functions. These functions are typically automatic and unconscious, like breathing, blinking, or the rhythm of one's heartbeat. However, in Somatic OCD, these normal bodily processes become the center of intense and unwanted attention.
Unpacking the Complexities of Somatic OCD
Heightened Focus on Involuntary Functions
Individuals with Somatic OCD experience a heightened state of consciousness regarding bodily processes that typically occur without notice. This could involve an acute awareness of the path air takes during respiration, the frequency of blinking, or the palpable beating of the heart.
Invasive Nature of Awareness
This is not just an increase in awareness but an invasive, often distressing fixation. It's as though the brain's usual ability to filter out mundane sensory information is impaired, resulting in a constant, intrusive focus on these autonomic processes.
Anxiety and Apprehension
Accompanying this heightened awareness is a profound sense of anxiety and fear. Sufferers may irrationally fear that ceasing to consciously monitor these functions could lead to their cessation, despite their involuntary nature.
Life Disruption
The relentless nature of this preoccupation can disrupt everyday life significantly. Routine tasks and activities demanding focus become formidable challenges, as the individual is continually sidetracked by their own internal sensations.
The Toll on Mental and Physical Well-being
Mental Health Challenges
The obsessive nature of this condition can lead to elevated levels of anxiety and stress, and in severe cases, even depression. The frustration and fear of losing control over one's thoughts can have a profound impact on overall mental health.
Physical Health Implications
The obsessive focus on bodily sensations can also manifest physically. For instance, an excessive preoccupation with breathing can result in hyperventilation, while a fixation on swallowing might lead to throat discomfort.
Exploring the Origins of Somatic OCD
Somatic Obsessive Compulsive Disorder can stem from multiple sources.
Neurological Underpinnings
The root causes of Somatic OCD are not entirely clear, but it's thought to involve a dysregulation in brain areas tasked with sensory information filtering. This dysregulation may lead to abnormal fixations on bodily sensations.
Psychological Triggers
Stress and anxiety are also considered significant contributors. Certain stressful events or periods in life can trigger the onset of Somatic OCD, especially in those predisposed to anxiety disorders.
Behavioral Aspects
A behavioral dimension is also evident in Somatic OCD. Attempts to suppress or ignore these intrusive thoughts can paradoxically make them more pronounced, creating a cycle of escalating obsession and anxiety.
Recognizing and Addressing Somatic OCD
Understanding the nuances of Somatic OCD is crucial, especially for parents, caregivers, and individuals facing this condition. Its profound impact on everyday life highlights the importance of acknowledging this form of OCD as a serious and legitimate challenge.
There are many myths about OCD, which makes it hard for even professionals to identify it. Recognizing Somatic OCD is the first step towards seeking effective treatment and support, paving the way for a journey toward better management and potential recovery.
How is Somatic OCD Diagnosed?
Diagnosing Somatic OCD requires a thorough evaluation by a mental health professional, typically involving clinical interviews and detailed questionnaires. The professional will assess for persistent, intrusive thoughts and repetitive behaviors related to bodily functions, which are the key indicators of Somatic OCD. It is important to work with a professional experienced with children and teens.
What are Other Types of Body or Health-Focused Disorders That Can Overlap with Somatic OCD?
Somatic OCD shares similarities with other disorders like hypochondriasis, where there's excessive worry about having a serious illness, and Body Dysmorphic Disorder, which involves preoccupation with perceived physical flaws. Distinguishing Somatic OCD from these disorders is crucial for appropriate treatment.
Somatic OCD Symptoms
Somatic OCD is characterized by an intense and often overwhelming focus on internal bodily sensations or processes. This condition goes beyond normal body awareness, creating a state of hyper-vigilance that can be both mentally and physically exhausting.
The individual may find themselves constantly distracted by these sensations, making it difficult to focus on tasks, engage in social activities, or even relax. This heightened state of alertness to bodily functions typically leads to significant anxiety and distress, as the individual may fear that ignoring these sensations could lead to harm or indicate a serious health issue.
Examples of Somatic Obsessions
- Breathing: An obsessive awareness of the rate, depth, or rhythm of breathing. Individuals may fear that if they stop thinking about breathing, they might stop breathing altogether.
- Heartbeat: A preoccupation with the sensation of the heartbeat, its speed, or regularity. There might be a fear that any variation in the heartbeat is indicative of a heart problem.
- Blinking and Swallowing: Intrusive thoughts about the frequency or the mechanics of blinking and swallowing. The individual might worry that these processes will not happen automatically.
- Digestive Processes: Obsessing over the sounds or sensations of digestion, leading to concerns about digestive health.
- Muscle Tension: Fixating on the feeling of muscle tension or relaxation in various parts of the body, such as the back, neck, or jaw.
- Skin Sensations: Becoming overly aware of sensations on the skin, like itching or temperature, leading to obsessive thoughts about skin health or diseases.
- Balance and Posture: Preoccupation with the sense of balance or the exact positioning of the body in space, causing anxiety and distress.
Examples of Somatic Compulsions
- Checking Breathing or Pulse: Repeatedly checking to make sure they are breathing correctly or that their heart rate is normal, often using medical devices like pulse oximeters.
- Seeking Medical Reassurance: Frequently visiting doctors or seeking medical tests to confirm that bodily functions are operating normally.
- Rituals Involving Bodily Functions: Engaging in specific breathing patterns, blinking a certain number of times, or swallowing in a particular way to ensure these functions continue normally.
- Mirror Checking: Frequently looking in the mirror to observe certain bodily functions or movements.
- Touching or Tapping: Using touch or tapping certain body parts as a ritual to ensure they are functioning or to ‘reset' a sensation.
- Counting or Timing Bodily Functions: Compulsively counting breaths, heartbeats, or the frequency of blinks or swallows.
- Avoidance Behaviors: Actively avoiding situations that might make their bodily awareness more acute, such as quiet rooms where internal sounds like heartbeat or breathing are more noticeable.
Understanding these specific symptoms and behaviors is crucial for parents and caregivers in recognizing Somatic OCD in their children. It helps in seeking appropriate professional help and providing the necessary support at home.
Distinguishing Characteristics of Sensorimotor Obsessions
A key feature of Somatic OCD is sensorimotor obsessions, which involve a debilitating awareness of autonomic bodily functions. Unlike general awareness, these obsessions create a fixation on these functions, leading to significant distress and compulsive behaviors.
Somatic OCD Treatment
Treatment usually combines therapy with methods that calm the brain. Supplements for OCD, neurofeedback, PEMF, and nutrition and diet can all work synergistically with Exposure and Response Prevention (ERP) therapy.
ERP therapy combines Cognitive Behavioral Therapy (CBT) with exposures and is highly effective, helping individuals to alter their thought patterns and responses to obsessive thoughts.
Somatic ERP Therapy
Exposure and Response Prevention (ERP) therapy, a form of CBT, is particularly successful in treating Somatic OCD. It exposes individuals to their fears (like ignoring a bodily sensation) and prevents the usual compulsive response, thereby reducing the anxiety over time.
Examples of Somatic Exposures in ERP Therapy
Exposure and Response Prevention (ERP) therapy is a cornerstone in the treatment of Somatic OCD. It involves gradually exposing the individual to their feared thoughts or sensations and then helping them to resist the urge to engage in compulsive behaviors. Here are some expanded examples of how somatic exposures can be applied in therapy:
Deliberate Focus with Controlled Response:
- Breathing: A common exercise might involve focusing intentionally on the act of breathing, noticing each inhale and exhale, and then consciously refraining from altering the breathing pattern despite any rising anxiety.
- Heartbeat Awareness: The individual might be asked to sit quietly and concentrate on their heartbeat, learning to tolerate the discomfort and anxiety without engaging in checking behaviors like taking their pulse.
Incremental Increase in Exposure Duration:
- Gradual Extension of Non-Checking: Start with brief periods of not checking bodily functions and gradually increase the duration. For example, if the person compulsively checks their swallowing, they might begin by delaying this check for one minute, gradually increasing to longer periods.
- Scheduled Attention Shifts: Setting specific times to focus on a bodily function, then deliberately shifting attention away for increasingly longer periods, helps in gradually reducing the anxiety associated with non-attention.
Mindful Exposure to Sensations:
- Mindful Walking: Paying attention to the sensation of feet touching the ground, then purposefully redirecting focus to the external environment, practicing staying present without obsessing over the sensation.
- Texture Exposure: Touching different textures and focusing on the sensation against the skin, then practicing letting go of the focus and moving attention to another activity.
Resisting Reassurance-Seeking:
- Refraining from Medical Consultations: For those who seek constant medical reassurance, an exposure exercise might involve resisting the urge to call or visit a doctor for a non-critical concern, slowly extending the time between these reassurance behaviors.
Sensory Overload Exposures:
- Intense Physical Activity: Engaging in rigorous exercise, focusing on the heightened awareness of bodily sensations like sweating or muscle fatigue, then practicing non-response to these sensations.
- Cold and Hot Exposures: Alternating between hot and cold temperatures in showers or baths, concentrating on the body's reaction to these extremes, then working on non-reactive behavior.
Visualization and Imaginal Exposures:
- Visualization of Worst-Case Scenarios: Imagining scenarios where the individual loses control over a bodily function, then mentally working through the anxiety without engaging in physical compulsions
Technological Aids:
- Using Apps or Recordings: Listening to guided meditations or apps that prompt focus on certain body parts or functions, then practicing shifting attention away after a set period.
These somatic exposure techniques are tailored to confront the specific fears and compulsions of the individual with Somatic OCD. By practicing these exposures under the guidance of a trained therapist, individuals learn to tolerate the anxiety associated with their obsessions, gradually reducing their impact and frequency over time.
How Parents Can Help a Child With Somatic OCD
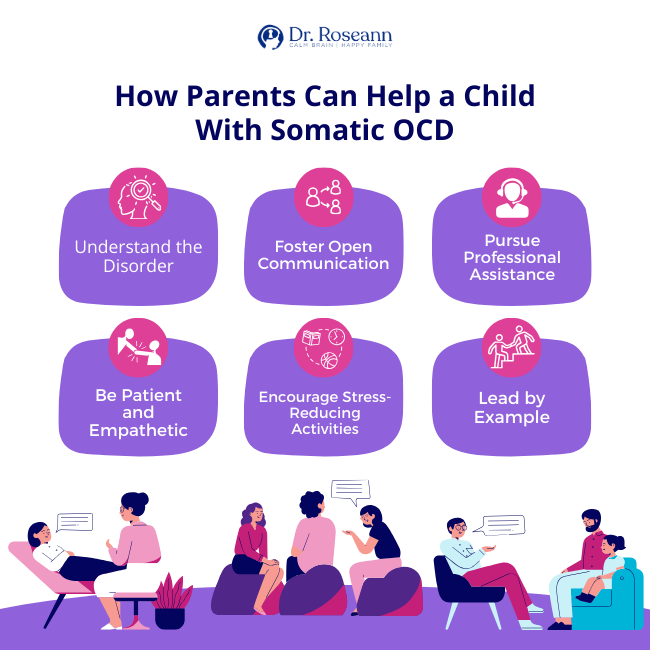
As parents, witnessing your child struggle with Somatic OCD can be both heart-wrenching and challenging. This subtype of Obsessive-Compulsive Disorder, marked by an intense preoccupation with bodily functions, can significantly impact your child's daily life and overall well-being.
Understanding how to effectively support and guide your child through this journey is crucial. In this section, we will explore various strategies and approaches that you, as a parent, can adopt to help your child manage and cope with Somatic OCD. From fostering a supportive home environment to collaborating with healthcare professionals, we'll delve into practical steps you can take to empower your child and facilitate their path towards recovery and resilience.
- Understand the Disorder: Comprehending the nuances of Somatic OCD is crucial for providing appropriate support.
- Foster Open Communication: Ensure your child feels comfortable discussing their fears and experiences without judgment.
- Pursue Professional Assistance: Engage with therapists skilled in treating OCD, particularly those experienced in ERP therapy.
- Be Patient and Empathetic: Recognize the challenge of overcoming Somatic OCD and appreciate each step forward, no matter how small without accommodating the behaviors.
- Encourage Stress-Reducing Activities: Activities like cooking together and regular exercise can be beneficial in managing anxiety.
- Lead by Example: Demonstrate positive coping mechanisms and non-reactive responses to symptoms.
Additional Considerations in Somatic OCD Treatment
Mindfulness and Relaxation Techniques and Somatic OCD
While mindfulness and relaxation techniques can be particularly effective in managing anxiety and even some forms of OCD, care should be taken in use of these techniques with Somatic OCD. Practices like yoga, deep breathing exercises, and mindfulness meditation can inadvertently reinforce the somatic OCD or my too anxiety producing of an exposure.
The Importance of a Supportive Environment
Creating a supportive and understanding home environment is crucial. Parents should educate themselves and other family members about Somatic OCD to foster empathy and reduce potential stressors in the home.
Involving the Child in Treatment Decisions
Involving children and teens in their treatment planning can empower them and increase their engagement in the therapeutic process. Psychoeducation about OCD is key in this process. This collaborative approach can make the process of confronting OCD easier.
Citations
Bürgy M. (2019). Phenomenology of Obsessive-Compulsive Disorder: A Methodologically Structured Overview. Psychopathology, 52(3), 174–183. https://doi.org/10.1159/000501165
Puranen J. P. (2022). Bodily obsessions: intrusiveness of organs in somatic obsessive-compulsive disorder. Medicine, health care, and philosophy, 25(3), 439–448. https://doi.org/10.1007/s11019-022-10090-3
Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive-compulsive disorder. Nature reviews. Disease primers, 5(1), 52. https://doi.org/10.1038/s41572-019-0102-3
Van Noppen, B., Sassano-Higgins, S., Appasani, R., & Sapp, F. (2021). Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder: 2021 Update. Focus (American Psychiatric Publishing), 19(4), 430–443. https://doi.org/10.1176/appi.focus.20210015
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023










