Stress and anxiety disorders are more prevalent than ever in today's perpetually connected world, where we are bombarded by constant input from various sources. As adults, multi-tasking is a common expectation, and we are pushed to go further faster in every aspect of our lives, endlessly comparing ourselves to others via a steady stream of social media. It should come as no surprise that nearly half of adults experience mental disorders during their lifetime, and one in two children have a physical or mental health issue.
It's common for someone to be dealing with depression, anxiety, or obsessive-compulsive disorder (OCD). Over 3 million Americans struggle with obsessive-compulsive disorder, commonly called OCD. You may have heard someone refer to their insistence on something being in a specific order or organized neatly as OCD. Often OCD is referred to almost jokingly. But it’s not a joke for millions. It’s a day-to-day struggle.
Kayla’s Story
After seeing four therapists, Kayla and her parents found their way to us. Kayla, a tween girl, first experienced anxiety as a young child. The anxiety disorder quickly morphed into OCD. She went from therapist to therapist with no success. The OCD steadily worsened.
One of her family members recommended our office after noticing Kayla’s obsessive thinking and compulsive rituals had reached the point that she couldn’t sit next to anyone. She couldn’t ride on the bus or in a car. She couldn’t even sit in her classroom seat if someone was beside her. Some days, her obsessive thinking and anxiety disorder paralyzed her so much that she couldn’t even make it to school or perform her usual daily activities.
Her parents wanted to know, “Is OCD neurological or psychological?” and just need help with OCD because it tool over their life.
Kayla began neurofeedback therapy to calm her nervous system and Exposure and Response Prevention Therapy (ERP) to gain the skills to “talk back” to OCD, allowing her to tune out her obsessions and resist the mental compulsions.
With neurofeedback therapy, she began to gain control over her unwanted thoughts. Within a short time, Kayla and her parents noticed less obsessive thinking and questioning. She wasn’t tense all the time. She could finally sit with her immediate and extended family members at dinner, enjoy activities, and sleep again.
Most importantly, Kayla has more control over her worries, obsessions, and compulsions for the first time. She didn’t know that was even possible. Kayla progressed well after several months of therapy. She continues to be free from obsessive thinking today.
What is Obsessive Compulsive Disorder?
OCD is a mental illness characterized by unsubstantiated and irrational fear or anxiety, leading to self-imposed, time-consuming repetition of personal rituals. The most common ritual OCD is associated with is compulsive hand washing. However, people rarely realize that OCD is the connection between the fear of dirty objects and the cause of excessive hand washing.
An OCD sufferer might insist on washing their hands in a perfectly timed routine out of irrational fear, whether they fear their death, the death of a loved one, or possibly the destruction of something they hold dear. The underlying reason for these mental rituals is the root of the issue. A person suffering from OCD often profoundly believes that their fears, their performance of these random rituals, and the potential consequences are all connected.
OCD frequently starts in late adolescence or early twenties, although it occasionally begins in childhood. The onset of OCD occurs by age 14 in approximately 25% of cases. Between 1% and 3% of children and teens have OCD, making it one of the more common mental disorders in that age group. For at least 4 out of every ten individuals diagnosed with OCD, it becomes a chronic disorder.
Though OCD manifests in late adolescence, only an estimated 40% of individuals who develop OCD in childhood will recover from the disorder by adulthood; for the other 60%, however, a childhood onset often means the disorder will be severe and chronic.
Symptoms of Obsessive Compulsive Disorder
Every child goes through periods of extreme worry and fear, but kids with OCD can't stop worrying, no matter how irrational the fear is or how well Mom and Dad reassure them. The anxiety seems hard-wired in their brain and compels them to behave in ways they believe will prevent something awful from happening. They may not even be able to articulate why, but they know their rituals make them feel better, safer, and less anxious, so they repeat them constantly.
OCD can negatively impact your child’s development, relationships, and future. For this reason, knowing what to look for and recognizing the signs of OCD is imperative. Early treatment is key to their chances of recovery. Left untreated, these obsessions and compulsions worsen dramatically over time and could destroy their future.
OCD is commonly only thought of in terms of only having compulsive behaviors, but obsessive thinking is the more common form of OCD, which makes it hard to detect. With the common causes and triggers of OCD yet to be discovered, parents need all the support they can get.
Common OCD Symptoms in Children and Teens
Signs of OCD might include:
- Frequent irrational worries or fears
- Complaints of disturbing thoughts and feelings they can’t control
- Unusual or illogical behaviors that they can’t explain
- Becoming upset or anxious if something is out of order
- An uncontrollable desire to put things in a particular order
- Strange rituals, such as circling the room twice before walking out a door
- Compulsive behavior of any kind
- Difficulties focusing at school or while doing homework
- Frequent checking and rechecking of things
- Consistent worry that something terrible is going to happen
- Trouble making or keeping friends
- Getting upset or angry if they’re prevented from performing a compulsive behavior or if it’s interrupted before it’s completed.
- Depressed mood or anxiety disorder
It's not unusual for a child to have OCD before parents, teachers, or doctors realize it. While there are numerous symptoms of OCD, they come on gradually. Parents may only suspect OCD if their child discusses their fears with them or the child exhibits odd behavior chronically.
Parents often ask, “Does OCD come in waves?” because of the typical waxing and waning of symptoms due to life stressors.
Suppose your child manifests any of the above signs, it's best to talk with qualified mental health professionals. A clinical psychologist, child psychiatrist, or OCD specialist can talk with you and your child to determine a cause for concern. Early intervention is critical, so never dismiss chronic behaviors or excessive fears as quirks or a phase.
Neurofeedback For OCD
The human brain is an extraordinarily complex system. Still, brain scans indicate people with OCD have abnormal brainwave activity in certain areas of the brain associated with strong emotions and reactions, making them especially prone to overthinking or repetitive behaviors and thinking that results in a looping pattern in brain wave functioning (hyper coherence).
Neurofeedback therapy can train the areas of the brain associated with control and emotional reactivity to adjust brain patterns. This OCD brain treatment helps reduce OCD symptoms by managing overactive brain waves and helps retrain the brain to calm the over-reactivity of the nervous system, reducing obsessions and compulsions.
By giving the brain direct feedback, the brain learns, over time, to better regulate itself. The nervous system calms down, and the limbic system can more appropriately react to stimuli instead of irritating the brain and body.
The brain-based therapies we use, such as Neurofeedback therapy, Biofeedback, and BRT, directly impact the subconscious brain. It also reduces brain deregulation and reverses OCD by calming the nervous system to respond healthily to stimuli. That means fewer obsessions, compulsions, irritated and angry behaviors, worried thoughts, calm thinking, and engaged behaviors while developing the ability to think and act without getting stuck.
How Neurofeedback Therapy For OCD Works
Neurofeedback is a safe, non-chemical method to treat OCD and a variety of other conditions at a subconscious level. This non-invasive therapy aims to help train the brain to function more efficiently. It works through operant conditioning or reward-based training for the brain to create an appropriate pattern through reinforcement.
The first step in neurofeedback OCD is conducting a QEEG Brain Map, where EEG brainwave activity is recorded and statistically analyzed. This session consists of the placement of sensors on the scalp and ears. Once the QEEG session is complete, the child and their parents meet with the healthcare provider to review the brain map. The doctor, the parents, and the child form the best treatment plan. The number and length of sessions may vary based on each individual but may range from 20 to 100 or more sessions to complete the course of treatment.
During OCD treatment sessions, brain functioning is monitored while recording the feedback presented by the client. The goal is to train the client to promote or reduce different brain wave frequencies. Operant conditioning or reward-based training kicks in when the brain changes its activity. This teaches the brain to produce more appropriate patterns.
Through this reinforcement, new electrical brain activity occurs, and the brainwave activity is “shaped” toward more desirable, more regulated performance. As the brain learns to self-regulate, these changes reduce numerous symptoms – less compulsive thinking and behaviors, fear, and worry. These changes are lasting and remain stable over time.
How A Brain Map Identifies the Impact of OCD on Brain Functions and the Nervous System
When using QEEG to measure brainwave activity, it’s possible to see certain areas of the brain affected in people with OCD. Here are some of those parts:
1. Prefrontal Cortex
This is the front part of the brain, responsible for making decisions and controlling impulses. In kids with OCD, the QEEG shows unusual activities in this area. It means that their brain has trouble regulating obsessive thoughts and compulsive behaviors.
2. Anterior Cingulate Cortex (ACC)
The ACC helps detect errors, handle conflicts, and process emotions. In children and teens with OCD, this part of the brain is more active than usual. Such hyperactivity may contribute to the constant feelings of uncertainty and distress that they experience.
3. Basal Ganglia
The basal ganglia are deep inside the brain and control movements and habits. The caudate nucleus in the basal ganglia may not work properly in kids with OCD, which can lead to ritualistic and repetitive behaviors.
4. Thalamus
The thalamus acts like a relay station for information from our senses. It helps us pay attention and filter out unnecessary things. For individuals with OCD, the QEEG brain map shows that the thalamus may have abnormal brainwave activity. This can make it harder for them to filter out intrusive thoughts or sensations.
How Does Neurofeedback Therapy Help Treat OCD?
Clients who undergo neurofeedback therapy and complete their full treatment course experience a significant decrease in exaggerated emotional reactivity. Neurofeedback and ocd involves calming overactive brain communication that leads to intrusive thinking.
Soon, they will be able to regulate their emotions better. After several neurofeedback training sessions, healthier brain waves are created, which will eventually help reduce OCD symptoms.
Patients don’t require knowledge about brain waves as the clinical staff guides the client through the process. Neurofeedback therapy is a promising course of treatment for OCD. It’s simple, painless, and free of side effects.
While other OCD therapies risk side effects or take years to produce limited results, neurofeedback clients often see a clinical improvement after only a few sessions. The brain learns to work better without feedback through multiple neurofeedback training sessions. In time, this leads to permanent changes and life-changing benefits.
7 Reasons Neurofeedback Training Can Help OCD Reduce Obsessive Thoughts and Compulsive Behaviors
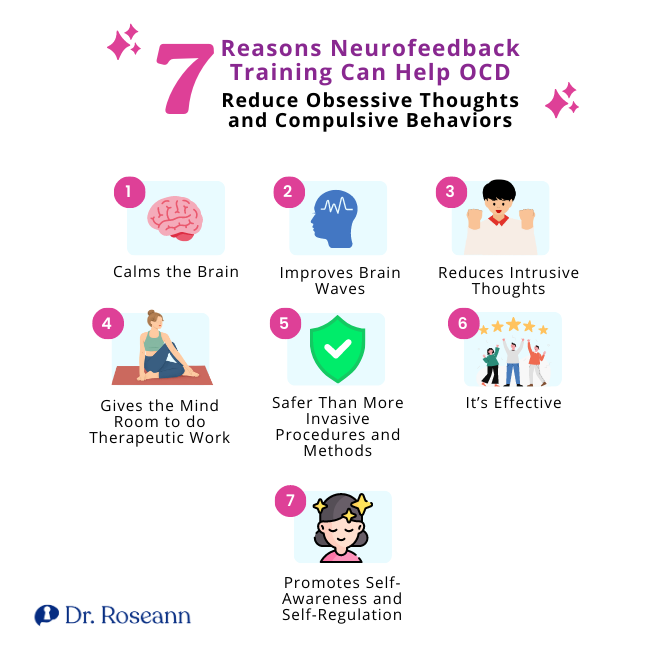
How to heal an OCD brain with nutrition, nutrients, brain treatments and psychotherapy is why many indivduals seek me out. OCD is a tryant and can really derail a life when the right mix of treatments and methods aren't found.
Neurofeedback training has gained recognition for its potential to assist individuals with OCD by targeting the underlying brain patterns to reduce symptoms. Neurofeedback is a special therapy that can help with OCD by working directly with our brain waves without causing adverse side effects.
It can specifically target and change how our brain works to address the underlying reasons why OCD happens and positively change our brain functions. Here are several compelling reasons why neurofeedback training can be a valuable approach to reducing OCD thoughts and behaviors:
1. Calms the Brain
Neurofeedback training helps calm the brain by promoting self-regulation and reducing overactive brainwave activity. By providing real-time information about brainwave patterns, people can learn to identify and modulate their own brain activity, leading to greater calmness and reduced anxiety.
2. Improves Brain Waves
Neurofeedback training aims to enhance specific brainwave patterns associated with improved cognitive function and emotional well-being. Targeting and training specific brainwave frequencies, such as alpha and theta waves, help rebalance brainwave activity and improve overall brain functions.
3. Reduces Intrusive Thoughts
Neurofeedback training has shown promising results in reducing the frequency and intensity of intrusive thoughts commonly experienced in OCD. Training the brain to modify its neural pathways and strengthen adaptive patterns can effectively decrease the occurrence of persistent thoughts.
4. Gives the Mind Room to do Therapeutic Work
Neurofeedback training enhances the effectiveness of other therapeutic approaches, such as ERP, which is a common treatment for OCD. It calms the brain and reduces anxiety levels while creating an optimal state for engaging in ERP therapy, allowing kids to confront their fears and triggers more effectively.
5. Safer Than More Invasive Procedures and Methods
Neurofeedback training is considered a safe and non-invasive approach compared to similar procedures or pharmacological interventions. It involves using sensors placed on the scalp to monitor brainwave activity.
There are no surgical procedures or medications that cause side effects. This makes neurofeedback therapy attractive for parents seeking alternative methods to treat OCD or hesitant about more invasive procedures for their kids.
6. It’s Effective
Numerous studies have demonstrated the efficacy of neurofeedback training in reducing OCD symptoms. Research has shown that neurofeedback therapy can significantly improve obsessive thoughts, compulsive behaviors, anxiety levels, and overall quality of life (Esmaeeli, 2021), with no known side effects.
7. Promotes Self-Awareness and Self-Regulation
Neurofeedback training actively engages with our brainwave activity and learning to regulate it. This process promotes self-awareness, helping us recognize when our thoughts and behaviors are veering toward obsession or compulsion.
With this awareness, we can intervene and redirect our focus, ultimately gaining more control over our thoughts and behaviors. Neurofeedback training empowers individuals with OCD to actively participate in their healing journey by developing self-regulation skills that can be applied to daily life.
Does Neurofeedback Therapy Work for OCD? The Research on Neurofeedback for OCD
From the research on QEEG Brain Map data (Prichep et al., 1993), we know which specific brain regions are over and under-activated when a person has OCD. While many of those afflicted with OCD have overactivation in their brain structures and communication, with over 10,000 brain maps, I have also found that OCD can result in stimulation due to infectious disease states associated with clinical conditions such as PANS and PANDAS streptococcal infections and autoimmune encephalopathy.
OCD can be a highly treatment-resistant condition when treatment doesn't address the neuro-behavioral components of the mental disorder. In our BrainBehaviorReset™ Program, when we work with children and teens with OCD and their families, we calm the brain with science-backed methods, such as neurofeedback therapy, and teach individuals how to dismantle the behavioral components of obsessions and compulsions with ERP therapy.
Research shows that neurofeedback therapy can reduce obsessions and compulsions without medication or harmful medication side effects (Barzegary, L., Yaghubi, H., Rostami, R., 2011 and Kopřivová et al., 2013).
In a meta-analysis of the data on neurofeedback research (Ferreira, S., Pêgo, J. M., & Morgado, P., 2019), despite heterogeneity groupings, “The overall effect size within the treatment group varied between medium to large,” indicating that neurofeedback research for OCD can be a powerful component to treat OCD.” Moreover, studies show that gains in OCD symptom reduction from neurofeedback were maintained post-treatment (Sürmeli & Ertem, 2011).
What is the Most Successful Therapy for OCD?
When you have OCD, the more you try to make the distress disappear, the more you worsen the problem. While that may provide temporary relief, OCD behaviors will soon become a bad habit that's hard to break, even if you try talking to someone or taking medications, which may have side effects. That's how the vicious cycle of OCD starts.
That's why getting the right kind of help early on is important. Our BrainBehaviorResetTM Program combines Exposure Therapy, Cognitive Behavioral Therapy (CBT), neurofeedback, CALM PEMF™, and magnesium supplementation to help your kids combat the common causes of OCD, face their fears, and learn how to deal with them so they no longer control their life.
But before starting ERP therapy, we teach parents how OCD affects the brain and behavior. It's different from regular therapy or medication, which may have side effects because you'll understand why your thoughts are going haywire and how to regain control.
We use ERP therapy and other non-invasive approaches to help OCD kids break free from constantly seeking reassurance, asking too many questions, worrying too much, and having repetitive behaviors like washing their hands or checking things repeatedly. Parents are involved in every session, so they can learn how to support their kids in a way that stops their obsessive thought or compulsive behavior.
While it can be that OCD cured for some, for others it requires continual care and managing of fearful thoughts. How to heal the OCD brain is part calming that activated nervous system and part gaining those skills to challenge those OCD fears and behaviors.
Citations:
Barzegary, L., Yaghubi, H., Rostami, R., (2011). The effect of QEEG- guided neurofeedback treatment in decreasing of OCD symptoms. Procedia – Social and Behavioral Sciences, Volume 30. https://www.sciencedirect.com/science/article/pii/S1877042811023469
Esmaeeli, S. (2021). The Effectiveness of Neurofeedback Training on the Working-Memory of People with Obsessive Compulsive Disorder Symptoms. European Journal of Molecular and Clinical Medicine, 8(1), 1795+. https://link.gale.com/apps/doc/A698747816/AONE?u=anon~76adea92&sid=googleScholar&xid=54dd8626
Ferreira, S., Pêgo, J. M., & Morgado, P. (2019). The efficacy of biofeedback approaches for obsessive-compulsive and related disorders: A systematic review and meta-analysis. Psychiatry research, 272, 237–245. https://doi.org/10.1016/j.psychres.2018.12.096
Kopřivová, J., Congedo, M., Raszka, M., Praško, J., Brunovský, M., & Horáček, J. (2013). Prediction of treatment response and the effect of independent component neurofeedback in obsessive compulsive disorder: a randomized, sham-controlled, double-blind study. Neuropsychobiology, 67(4), 210–223. https://doi.org/10.1159/000347087
Sürmeli, T., & Ertem, A. (2011). Obsessive compulsive disorder and the efficacy of qEEG-guided neurofeedback treatment: a case series. Clinical EEG and neuroscience, 42(3), 195–201. https://doi.org/10.1177/15500594110420031H0
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.