Obsessive Compulsive Disorder develops over time. Even when one has genetic underpinnings, our genetics don’t define us and anxiety or other clinical issues can be mitigated by lifestyle changes and learning healthy ways to cope with stress. OCD typically starts with anxiety that one engages in an action (intrusive thinking or compulsive behaviors) in order to avoid a negative result and this inadvertently negatively reinforces a behavior, which means it is more likely to occur. It is sort of like feeding a barking dog in that every time you feed into the intrusive thoughts you accidently allow them to take hold, then they are more likely to occur. Someone with OCD isn’t doing these behaviors on purpose and instead their behaviors get reinforced at a subconscious level. The good news is that OCD behaviors can be unlearned with the right kind of therapy, ERP combined with neurofeedback.
How Does OCD Effect the Brain of Children and Teens
OCD results when there is a dysregulation of brainwave activity in specific regions and in the neural networks. With a QEEG brain map or a brain check with our staff (we work with kids in person and remotely), you are able to see the exact regions that are impacted by OCD, as well as the neural networks. With OCD, regions that process emotional information, help you regulate stress, and apply the breaks and switch gears are highly impacted. When you look at the brain functioning of someone with OCD, a clear pattern emerges in that the region that regulates how one perceives stress is overactive, as well as their neural networks are “stuck on” in a continual looping of inner chatter. And when their central nervous system is hyper stress activated, they are too sensitive to seemingly benign stimuli and live in a constant state of activation or a fright response. That overactive brain that “can’t shut off” is something that every person with OCD reports and it is because of that overactive brainwave activity.
OCD Hijacks Your Brain Until You Treat It
Intrusive thoughts and compulsive behaviors hijacks a person’s brain and makes the day to day very difficult. When your brain is constantly in a state of fright, it is hard to be connected, focused, and do even simple tasks if those intrusive thoughts and compulsions are intense. Many people with OCD are highly functional and go through periods of waxing and waning when the thoughts and compulsions might be less or more intense. Kids can do really well in school as they channel their energy until the stress of that hijacked brain and constant inner chatter is just too much. There are science-backed natural methods that treat OCD and extinguish OCD behaviors and it's SUPER IMPORTANT that we address intrusive thoughts and compulsions early with kids, so we break the subconscious habit or negative reinforcement cycle.
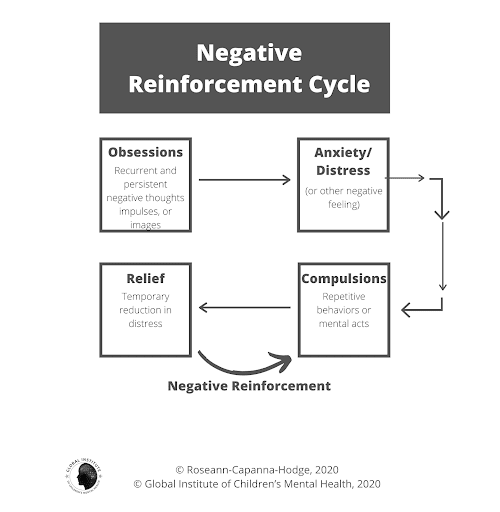
What is a Negative Reinforcement Cycle in OCD?
OCD is so treatment resistant due to something called a negative reinforcement cycle and how obsessive and compulsive behaviors get ingrained at a neurological level. Negative reinforcement in OCD is when you engage in an action in order to avoid a negative result. This avoidance robs the child or teen of the ability to learn that what they fear might not be quite as bad as they anticipated and actually reinforces the behavior. In other words, it means the child will neurologically be more likely to keep repeating the behavior instead of learning a new, healthier way to tolerate and cope with the stress. It is sort of like feeding a barking dog in that every time you feed into the intrusive thoughts or compulsive behaviors by avoiding, you actually allow them to take hold, then they are more likely to occur. This isn’t purposeful and instead occurs at a subconscious level. It is because of this negative reinforcement cycle that OCD can be very treatment resistant and why regular talk therapy doesn’t help OCD and in fact often worsens it. You need the right treatment for OCD or it is a clinical issue that will fester for years.
Is OCD Inherited?
OCD can result from genetics but also can result from other sources including, anxiety or medical conditions such as PANS/PANDAS and Lyme Disease. PANS/PANDAS are two different disorders that occur when an infectious or toxin triggers that causes a misdirected immune response that results in a sudden onset of a psychiatric issue such as OCD, anxiety, depression, rage, suicidal thoughts or the loss of focus, learning and memory issues, or a regression of behaviors.
Why is OCD Misdiagnosed?
OCD is misunderstood and often missed by medical and mental health professionals, as they lack the training to dive into the thoughts and behaviors of their patients. OCD is most commonly misdiagnosed as an anxiety disorder or depression.
OCD also co-occurs at a high rate with clinical conditions such as Autism Spectrum Disorder and PANS/PANDAS and it may be missed as providers focus on the primary issue. PANS/PANDAS and OCD are increasingly common and certainly on the rise with one in every 150 to 200 children being diagnosed. If your child has a sudden onset of OCD, then PANS/PANDAS must be ruled out. You can learn more about what PANS/PANDAS is here.
If you are not sure if your child has OCD, you can learn what the signs and symptoms of OCD in children are and how OCD is diagnosed in children in my blog, OCD in children.
How Do You Treat OCD Without Medication?
Given the potential of medication side effects and the toxic effect of psychiatric medications on a developing brain, it is preferable to begin treatment with ERP and neurofeedback. This combination is not only effective but it’s safe and natural.
OCD is very treatable when properly diagnosed and under the care of a highly trained OCD therapist. When we work with kids and their families in person or remotely we have found that consistent with the research, Exposure Response and Prevention Therapy (ERP) coupled with Neurofeedback for OCD is the winning combination. I am a huge proponent of supplements for OCD too or any science-back natural treatment for OCD.
The reason why neurofeedback for OCD and herbs for OCD coupled with ERP therapy for OCD works so well is that they calm the CNS and prime it for the new learning that occurs in ERP. ERP teaches you to get control of the OCD instead of the OCD controlling you and when we pair it with neurofeedback the nervous can go into that required parasympathetic dominant state for new learning to occur. Just think about it, how can you learn when your brain is in fight, flight, or freeze like it is with OCD… science tells us (and common sense) you can’t.
Want to learn more about OCD?
Wondering what are the signs and symptoms of OCD? Then read this article, What is OCD? OCD in children can look different than adults and is often missed. It often starts with subtle behaviors, such as a need for reassuring questions, insistence on nighttime rituals, or other behaviors that you may interpret as, “nerves” or worry. To learn more about the signs and symptoms of OCD in children and teens, read this blog to help you understand what’s the difference between anxiety and OCD. There are great natural treatments for OCD, including supplements for OCD or herbs for OCD, neurofeedback for OCD, and Exposure and Response Prevention for OCD and here is more information about how OCD is treated.. Looking for information on natural solutions and treatments for OCD? Then download this FREE Natural Solutions and Treatments for OCD. And wondering what the research says what dosages of these herbs and supplements your child should be taking, then download this FREE OCD Supplement Checklist.
Are you looking for help for your child’s or teen’s behavior?

Boy, the world is stressful right now (and it has been for a long time!). Of course, you are worried about your child’s stress level! You want to see them SUCCEED and be confident. Your child may be struggling with focus, stress, mood, behavior, emotions, or socially and you aren’t sure what to do about it and you feel STUCK… Well, Dr. Roseann is here to show you how to GET UNSTUCK and cultivate success in small and big ways!
As a licensed therapist and certified psychologist, as well as a special needs mom herself, Dr. Roseann knows what it is like to search for ways to help your child’s attention, learning, and behavior and still see your child struggle. So, if you’ve gone down the Google MD and ineffective medication and therapy rabbit hole, it is time to get support from Dr. Ro who can help you help your child to be focused, calm, and feel good about themselves.
Want to work with Dr. Roseann, so you can turn your child’s behavior around and GET UNSTUCK and CULTIVATE SUCCESS?
Join our Raising Successful Kids Community, where you get Dr. Roseann secrets to raising a successful child at school, home and in life regardless of your kid’s age or ability. For less than $1 a day, you get Dr. Ro, the foremost expert in the world on children’s mental health in your back pocket! Join a community of like-minded parents and get the secret sauce to cultivating confidence, independence, and success in your child in only the way that Dr. Ro can do!
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
Want to work with Dr. Roseann personally? She sees people at her Ridgefield, CT center using neurofeedback, biofeedback, and psychotherapy to turn behavior around, as well as does neurofeedback and coaching remotely. She has also reached billions through her dozens of media appearances on her mission to, ‘Change the way we view and treat children’s mental health™.”
The best way to find out if we can help you is to apply to work with us, so we know you are ready for the powerful change that lies ahead.
Are you a professional who wants more training from Dr. Roseann?
Sign up for her Professional Webinars and CE-Based Courses or purchase her book, Teletherapy Toolkit™: Therapist Handbook for Treating Children and Teens.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.” She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2021










