There is a LOT of misinformation about Obsessive Compulsive Disorder (OCD)! I spend a fair amount of time debunking OCD myths with clients, parents and even other mental health professionals. Getting the facts straight helps in not only understanding OCD but helps parents and individuals find the right treatment.
MYTH #1 – We all have some level of OCD
Uh, no on that one. OCD is a clinical disorder and even though people often think that OCD means you are organized and clean, I promise you that those with compulsions around cleanliness and germs or organization, don’t want to clean and organize; they are compelled in a really uncomfortable way.
OCD is a clinical disorder where a person or child experiences intrusive thoughts and fears (obsessions) leading to compulsive behaviors. Individuals with OCD engage in compulsive behaviors attempting to end the obsessions, decrease distress and worry, or stop perceived negative things from happening. It is all about compulsive mental and behavioral rituals needed to reduce uncomfortable and anxious feelings.
OCD is a disorder that shows itself differently for each person depending on their intensity level and type of obsessions and compulsions. Common OCD obsessions include: fear of death, germ and contamination concerns, cleanliness fixations, religious over-observations (Scrupulosity), aggressive or sexual impulses, and symmetrical or organization obsessions are common. Common compulsions include checking, washing/cleaning, and arranging.
MYTH #2 – OCD is Always Genetic
OCD can result from genetics but also can result from other sources, including, but not limited to, anxiety or medical conditions such as PANS/PANDAS/AE and Lyme Disease. PANS/PANDAS are two different disorders that occur when an infection or toxin triggers and causes a misdirected immune response that results in a sudden onset of a psychiatric issue such as OCD, anxiety, depression, rage, suicidal thoughts or the loss of focus, learning and memory issues, or a regression of behaviors.
It can even be triggered by psychiatric medication in some cases, especially when medication is used “off label” or a person is struggling with infectious disease or a high toxin level.
For most, OCD develops over time. Even when one has genetic underpinnings, our genetics don’t define us and anxiety or other clinical issues can be mitigated by lifestyle changes and learning healthy ways to cope with stress. OCD typically starts with anxiety that one engages in an action (intrusive thinking or compulsive behaviors) in order to avoid a negative result and this inadvertently negatively reinforces a behavior, which means it is more likely to occur. It is sort of like feeding a barking dog in that every time you feed into the intrusive thoughts, you accidently allow them to take hold, then they are more likely to occur. Someone with OCD isn’t doing these behaviors on purpose, and instead, their behaviors get reinforced at a subconscious level. The good news is that OCD behaviors can be unlearned with the right kind of therapy.
OCD can develop in response to a trauma, as intense anxiety can lead to a negative reinforcement cycle. The avoidance of uncomfortable emotions, sensations and thoughts can fuel obsessive thinking and compulsive behaviors.
MYTH #3 – OCD and Anxiety are the Same
OCD and anxiety are different clinical disorders that require different treatments. Even though most see anxiety and OCD as similar conditions, they are quite different. One of the greatest barriers to successful OCD treatment is misusing anxiety therapy, which can feed the OCD.
Exposure and response prevention (ERP) therapy is the gold standard of treatment for those with OCD. It’s systematic methods address the neurological behavioral habituation of OCD and has a lot of research to substantiate how effective ERP is in reducing OCD symptoms.
ERP is a combination of Exposure Therapy and Cognitive-Behavior Therapy (CBT) that gradually exposes a person to their trigger(s) so they learn how to be uncomfortable to the point where they can tolerate and ignore their trigger. ERP combines deep psychoeducation about how OCD impacts brain and behavior and the coping skills and tools that allow one to take control of their OCD.
MYTH #4 – You Always Need Medication to Treat OCD
Many people effectively treat their OCD without medication when they use tools such as neurofeedback and Exposure and Response Prevention Therapy (ERP). OCD psychotherapy (ERP) should always be used before medication because it addresses the behavioral habituation component of OCD.
OCD results when there is a dysregulation of brainwave activity in specific regions and in the neural networks. With OCD, regions that process emotional information, help you regulate stress, and apply the breaks and switch gears are highly impacted. When you look at the brain functioning of one with OCD, a clear pattern emerges in that the region that regulates how one perceives stress is overactive. And when their central nervous system is hyper stress activated, they are too sensitive to seemingly benign stimuli and live in a constant state of activation or a fright response. Neurofeedback works to safely and effectively calm brain and nervous system dysregulation so a person with OCD can learn how to talk back to their OCD.
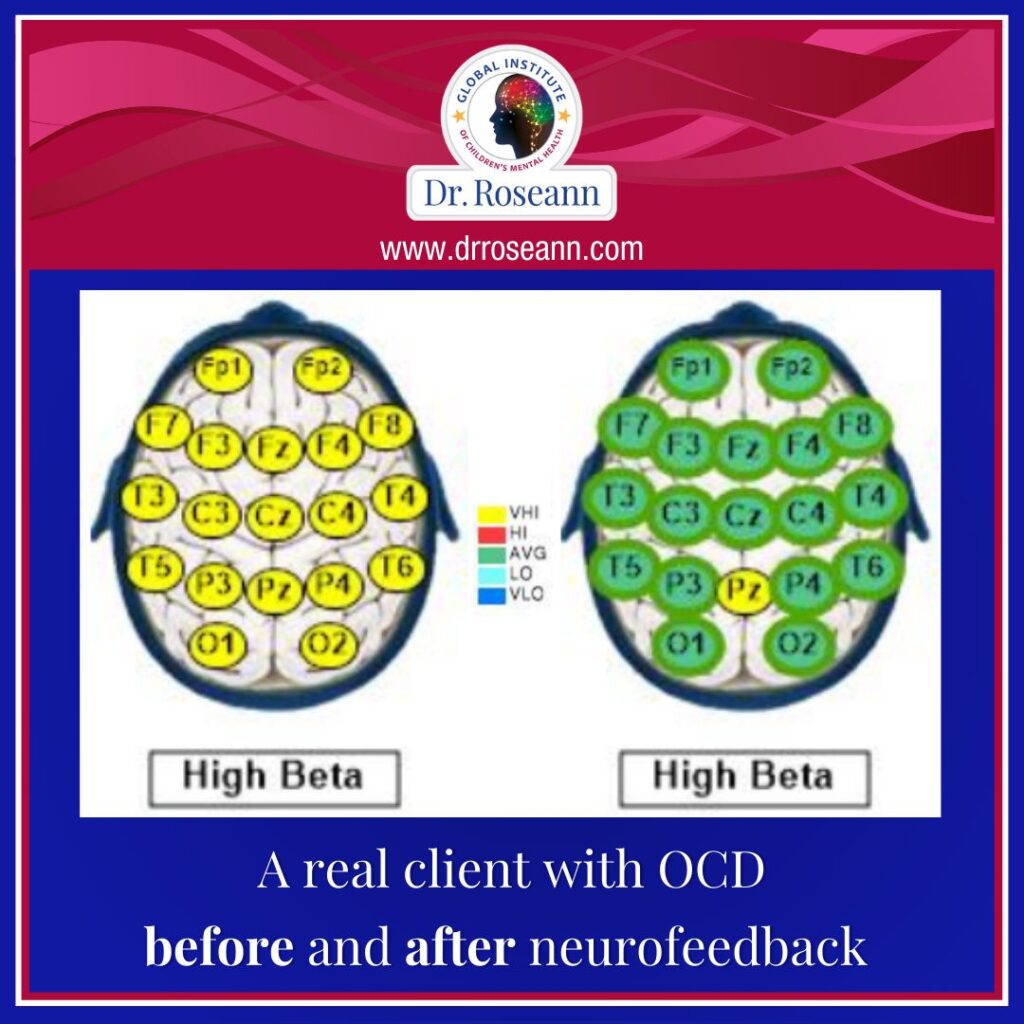
At our Ridgefield, CT center we work with children and teens with OCD in-person and remotely at home by using neurofeedback to calm the nervous system and move a child to a more relaxed, parasympathetic state. With a regulated, calm nervous system, the person with OCD can have the bandwidth to take action and think differently because their brain isn’t hijacked by intrusive thoughts. Neurofeedback calming one’s brain means a person experiences fewer intrusive and worried thoughts, compulsions, and irritated and angry behaviors.
MYTH #5 – You Can’t Have OCD and be Functional
Many people with OCD are highly functional and go through periods of waxing and waning when the thoughts and compulsions might be less or more intense. Intrusive thoughts and compulsive behaviors hijacks a person’s brain and makes the day to day very difficult. When your brain is constantly in a state of fright, it is hard to be connected, focused, and do even simple tasks if those intrusive thoughts and compulsions are intense.
MYTH #6 – OCD is Easy to Diagnose
OCD is misunderstood and often missed by medical and mental health professionals, as they lack the training to dive into the thoughts and behaviors of their patients. OCD is most commonly diagnosed as an anxiety disorder or depression. OCD also co-occurs at a high rate with clinical conditions such as Autism Spectrum Disorder and PANS/PANDAS and it may be missed as providers focus on the primary issue.
An OCD diagnosis is made by a medical or mental health professional after a one or two part clinical interview. A highly tried OCD clinician will dive into what a person’s OCD triggers are, their obsessive thoughts and compulsions and the intensity that they experience these behaviors. While people often joke they have OCD, obsessions and compulsions must occur an hour or more a day and interfere with their daily functioning.
MYTH #7 – Once You Have OCD, You Can Never Get Rid of it
Even though pharmaceutical companies want you to believe you will always need your OCD meds, through the use of ERP and other therapies that calm the CNS such as neurofeedback or biofeedback, one can learn to manage and even eliminate obsessions and compulsions. The key to combating OCD is to work with a highly trained OCD specialist who teaches you how to take control of one’s OCD and learn how to tolerate being uncomfortable and break that negative reinforcement cycle.
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023