If you’re a parent of a child with autism spectrum disorder (ASD), you might be familiar with the overwhelming array of treatment options—especially when it comes to managing co-occurring conditions like anxiety and obsessive-compulsive behaviors.
Many parents turn to medication, particularly selective serotonin reuptake inhibitors (SSRIs) like Prozac, hoping it will alleviate these symptoms. But recent research reveals a reality that may surprise you: Prozac, one of the most commonly prescribed SSRIs for children with autism, is no more effective than a placebo when it comes to treating these challenging behaviors.
Despite the increasing prevalence of autism—affecting 1 in 44 children in the U.S. as of 2021—medication often fails to address the core symptoms of autism. Yet, many families are still left with few alternatives, prompting a continued reliance on SSRIs. So, what does this mean for parents trying to make the best decisions for their child’s health? This article dives into the research on autism and Prozac, its side effects, and why a more holistic, brain-calming approach may offer better long-term results for children with ASD.
At my Ridgefield, CT clinic, the philosophy of “skills not pills” forms the foundation of how we approach autism spectrum disorders. We believe that instead of relying on medication, a holistic approach is far more effective in helping children thrive. Our focus is on nurturing the brain and body using a combination of targeted behavioral interventions.
Clinical Study on Prozac and Autism Spectrum Disorders
Prozac is the brand name for fluoxetine, a type of selective serotonin reuptake inhibitor (SSRI). Fluoxetine treatment is often prescribed to manage symptoms of depression and anxiety, helping to stabilize mood and improve overall emotional well-being.
New research demonstrates what most already know, that SSRI medications don’t move the dial for anxiety and obsessive-compulsive behaviors in children with autism spectrum disorder (ASD).
Autism is on the rise across the globe, and as of 2021 in the United States, 1 in 44 children have autism. The guidelines for autism took more than 12 years to be updated and were last updated in 2019.
Early intervention is critical in life outcomes in children with autism, but diagnosis isn’t standardized, and autism occurs along a spectrum, so symptoms can be hard to identify.
Many choose to medicate their children with autism, especially if they have co-occurring conditions such as ADHD and OCD, because they aren’t presented with other options. There is no medication for autism itself or for its core symptoms, which are usually classified into three categories:
- Difficulties with social interactions
- Trouble communicating
- Repetitive behaviors
However, medication may be used to manage behaviors or conditions that tend to co-occur with autism. These can include anxiety, depression, or attention-deficit/hyperactivity disorder (ADHD). By focusing on these associated conditions, medications can help improve the quality of life for both the child and their family.
Research On Autism Medication
The results of the randomized clinical trial, published October 22, 2019 in JAMA, found that a commonly prescribed SSRI medication for children and adolescents with autism, is no more effective than a placebo at treating obsessive-compulsive behaviors. (Reddihough et al., 2019)
Prozac is a commonly prescribed medication for kids and teens with autism.
At first, the Prozac (fluoxetine) group appeared to show a slight lessening of obsessive-compulsive symptoms after the 16 weeks of treatment when compared with the placebo. However, after the researchers controlled for potentially confounding factors including age, sex and the severity of symptoms at the start of the trial, they found that there was no difference between the treatment and control groups. The group that received the Prozac did no better than the placebo and the obsessive-compulsive behaviors remained. In general, many children with ASD have anxiety and OCD symptoms.
This was a clinical trial conducted across multiple centers to compare fluoxetine and placebo in children and teens aged 7.5 to 18 years with autism spectrum disorders (ASDs). Participants had a score of 6 or higher on the Children’s Yale-Brown Obsessive Compulsive Scale (CYBOCS-PDD), indicating high levels of repetitive behaviors. The study took place in three health centers in Australia, with enrollment from November 2010 to April 2017 and follow-up ending in August 2017.
Participants were randomly assigned to receive either fluoxetine (75 participants) or a placebo (71 participants). The medication started at 4 or 8 mg per day (depending on weight) and was increased to a maximum of 20 or 30 mg per day over 4 weeks. Treatment lasted for 16 weeks.
The primary outcome measure was the change in CYBOCS-PDD scores, which range from 0 to 20, with higher scores indicating more severe repetitive behaviors. A clinically meaningful change was defined as a 2-point decrease. After 16 weeks, the fluoxetine group’s average score decreased by 3.72 points, while the placebo controlled study group’s score dropped by 2.53 points. The difference between the two groups was statistically significant, with a 2.01-point greater reduction in the fluoxetine group. However, when adjusted for additional factors, the difference was not deemed statistically significant.
Secondary outcomes look at side effects. Significant adverse events were common in both groups, affecting 45% of the fluoxetine group and 42% of the placebo group. The most frequent issues were mood disturbances like irritability, gastrointestinal problems (nausea, diarrhea), and sleep disorders.
The results of this current 2019 research, which is a randomized clinical trial, added further support to 2004 research, 2008 research, 2009 research, 2019 research that found none to mixed results for pharmacological interventions for those with autism. The findings in this 146- participant study, are consistent with other research, which demonstrates the inconclusive efficacy of SSRIs for those with ASD at best.
The researchers noted, “Published reports indicate that more than half of children and adolescents with ASDs are prescribed medication, with 21% to 32% receiving selective serotonin receptor inhibitors (SSRIs) despite inconclusive evidence for their efficacy”.
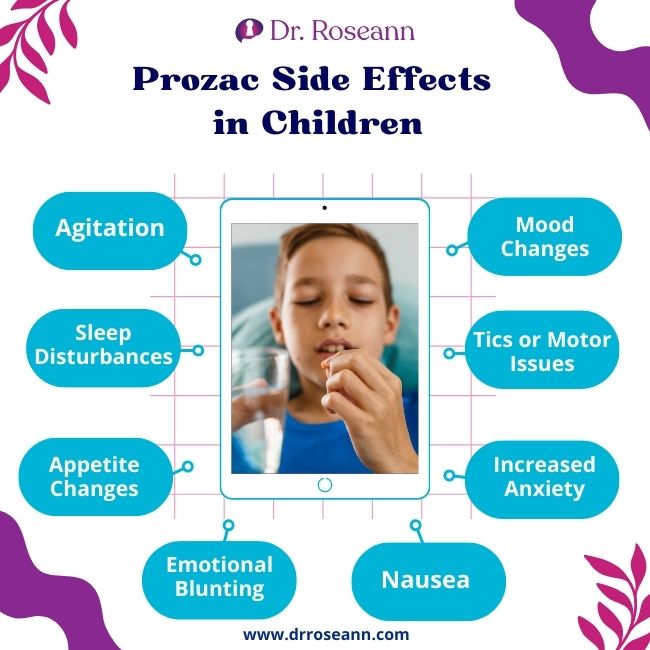
Prozac Side Effects in Children with Autism Spectrum Disorder
Common side effects of Prozac in children with ASD include:
Agitation, Restlessness or Repetitive Behaviors
Some children may become more agitated, irritable, or hyperactive after starting Prozac. This can sometimes manifest as increased repetitive behaviors or difficulty calming down. Some common examples of repetitive behaviors in children with autism include stemming, toe walking, walking in circles and rigid routines or rituals.
Sleep Disturbances
Prozac may cause insomnia or disturbances in sleep patterns, which can exacerbate behavioral issues, particularly in children who already have difficulty sleeping.
Appetite Changes
A reduction in appetite is a common side effect, which can lead to weight loss. Monitoring weight and nutrition is essential, especially for children with autism who may have restricted diets.
Emotional Blunting
Some children may experience reduced emotional responses or seem more detached or less expressive after taking Prozac.
Nausea or Gastrointestinal Issues
Fluoxetine can cause stomach upset, nausea, diarrhea, or constipation, which may be particularly difficult for children with sensory sensitivities.
Increased Anxiety or Aggression
In some cases, Prozac can initially increase anxiety or aggressive behaviors, particularly when starting or adjusting the dosage.
Tics or Motor Issues
Some children may develop new or worsened tics or other involuntary movements while on Prozac.
Mood Changes
Rarely, SSRIs like Prozac can cause mood swings, irritability, or even suicidal thoughts in children and adolescents. It’s important to monitor any behavioral changes closely, especially during the first few weeks of treatment.
Parents should work closely with their child’s healthcare provider to monitor for side effects, especially since children with autism may not always be able to express discomfort in typical ways. Regular check-ins and adjustments to the dosage may help mitigate some of the side effects.
Selective Serotonin Reuptake Inhibitors
Selective Serotonin Reuptake Inhibitors (SSRIs) are a class of medications primarily used to treat depression and anxiety by increasing serotonin levels in the brain. When it comes to autism, SSRIs are sometimes prescribed to manage symptoms such as anxiety, obsessive-compulsive behaviors, and irritability, which can be common in individuals with autism spectrum disorder (ASD).
However, the effectiveness of serotonin medications treating core autism symptoms—like difficulties in social interaction, communication, and repetitive behaviors—is unclear. Research on their use in autism is mixed. Some individuals with autism may benefit from SSRIs, particularly if they have co-occurring anxiety or obsessive-compulsive disorder (OCD), while others may not respond well or may even experience increased agitation, restlessness, or other side effects.
Autism Spectrum Disorders and Medication
So why is prozac still prescribed so much? Autism is a complex disorder with multiple reasons why it happens; none of which we really fully understand how these multiple factors interact and directly cause autism. Unfortunately, like so many disorders there is a constant push to find that magic pill that is going to fix it. We know that autism doesn’t result from a specific biochemical or genetic issue, so a different approach needs to be taken.
Parents need to know that they can reduce symptoms when they use evidence-based therapies, such as neurofeedback and exposure and response prevention psychotherapy (ERP) for OCD. You have to calm the brain and pair it with new learning and in the case of OCD, that means teaching a child with autism replacement behaviors for their fear driven obsessions and compulsions.
Remember, at the core of OCD is a fear of something bad happening if they don’t complete a behavior and that means they have to unlearn that and learn a new, healthy way to respond to their fears and worries. And children and teens with autism can do that with a combination of neurofeedback and ERP. Whether in-person at our Ridgefield, CT center or virtually all over the world, we guide parents with the best of science-backed therapies that work to calm the brain, which is the first step in treating autism and dysregulated kids.
Our BrainBehaviorReset™ Program focuses on:
- Nutrition
- Addressing Nutrient Deficiencies
- Sleep
- Genetic Mutations
- Detoxification
- Calming the brain with brain-based therapies
The pairing of science-backed therapies, such as neurofeedback, PEMF, biofeedback, and psychotherapy with support for the body has helped thousands of clients become calmer, more flexible, more focused, better able to communicate with others, and just feel more even in their mood.
How is autism diagnosed?
Autistic disorder is typically diagnosed through a comprehensive evaluation involving medical professionals, developmental specialists, and sometimes educators. There isn’t a single medical test for autism, such as a blood test or brain scan, so the diagnosis is based on observing behavior, developmental history, and assessing how a child meets (or does not meet) key developmental milestones.
The Autism Diagnostic Interview-Revised (ADI-R) is a structured interview used by clinicians and researchers to diagnose autism spectrum disorder (ASD). It includes detailed symptom checklist and is designed to assess key areas of autism, including communication, social interaction, and repetitive behaviors. The ADI-R is typically conducted with a parent or caregiver who knows the individual well and involves a detailed questionnaire covering the person’s developmental history and behavior. This tool is considered one of the gold standards for autism diagnosis, often used in combination with other assessments like the Autism Diagnostic Observation Schedule (ADOS).
Since autism spectrum disorders co-occurs with other mental health issues using, a mental health provider can test for these conditions with other diagnostic tools such as the Spence children’s anxiety scale and Brown obsessive compulsive scale. Healthcare professionals use the Diagnostic and Statistical Manual of Mental Disorders (DSM) as a guide as it provides standardized criteria for the classification of mental disorders.
What is PDD?
Pervasive Developmental Disorder (PDD) is a term that was used to describe a group of disorders characterized by delays in socialization and communication skills, and often associated with repetitive behavior and restricted interests. Pervasive developmental disorders included several conditions that are now recognized as part of the autism spectrum.
What are educational and behavioral interventions for autistic children and adolescents?
Educational and behavioral interventions for autism focus on improving communication, social skills, and behavior. Applied Behavior Analysis (ABA) is a common approach that uses positive reinforcement to teach new skills and reduce challenging behaviors. Social skills training helps individuals with autism learn how to interact effectively with others, while speech therapy improves communication abilities. Occupational therapy (OT) assists in developing motor skills and coping strategies for daily tasks. These interventions are tailored to the individual’s needs and can be delivered in both educational and home settings.
What is the maximum does of Prozac?
For children, the maximum dose is usually lower and determined by weight and age. The maximum dose of Prozac (fluoxetine) for most adults is typically 80 mg per day. However, for conditions like depression, anxiety, or obsessive-compulsive disorder (OCD), the usual maintenance dose ranges from 20 to 60 mg per day. It’s important to follow a doctor’s guidance, as dosing can vary based on the individual’s condition and response to treatment.
What are stereotypic and complex behaviors in autism spectrum disorders?
In autism, stereotypic behaviors are repetitive actions or movements that are performed in a predictable, patterned way. Examples include hand-flapping, rocking, or repeating certain phrases. These behaviors are often used by individuals with autism to self-regulate or cope with sensory overload.
Complex behaviors, on the other hand, involve more intricate or multi-step actions and interactions. These can include complex rituals or routines, detailed and repetitive patterns of play, or specific, often elaborate, ways of interacting with objects or people. While these behaviors can also be repetitive, they typically involve a more sophisticated sequence or organization. These behaviors may also be seen in adult autism spectrum disorders.
Why is low dose fluoxetine given to children?
Low-dose fluoxetine is given to children to treat conditions such as depression, anxiety, and obsessive-compulsive disorder (OCD). Starting with a low dose helps minimize the risk of side effects while assessing the child’s response to the medication. Gradually increasing the dose allows for careful monitoring and adjustment based on the child’s individual needs and tolerance. This approach aims to balance effectiveness with safety, ensuring the child receives the appropriate therapeutic benefit with minimal adverse effects.
Citations:
Reddihough DS, Marraffa C, Mouti A, et al. Effect of Fluoxetine on Obsessive-Compulsive Behaviors in Children and Adolescents With Autism Spectrum Disorders: A Randomized Clinical Trial. JAMA. 2019;322(16):1561–1569. doi:10.1001/jama.2019.14685
Palermo MT, Curatolo P. Pharmacologic treatment of autism. J Child Neurol. 2004 Mar;19(3):155-64. PMID: 15119475.
Soorya L, Kiarashi J, Hollander E. Psychopharmacologic interventions for repetitive behaviors in autism spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2008 Oct;17(4):753-71, viii. doi: 10.1016/j.chc.2008.06.003. PMID: 18775368.
King BH, Hollander E, Sikich L, McCracken JT, Scahill L, Bregman JD, Donnelly CL, Anagnostou E, Dukes K, Sullivan L, Hirtz D, Wagner A, Ritz L; STAART Psychopharmacology Network. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism. Arch Gen Psychiatry. 2009 Jun;66(6):583-90. doi: 10.1001/archgenpsychiatry.2009.30. PMID: 19487623; PMCID: PMC4112556.
Dr. Roseann is a mental health expert in Neurodivergence who is frequently in the media:
- Forbes Experts Say Wellness Design Provides Benefits To Individuals On The Autism Spectrum
- Medicinal Media Different minds grow awareness: understanding the autism spectrum
- Neurofeedback Autism in Action Podcast
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child’s Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024