A Guide to Autism Treatment for Children, Teens and Adults
Dive into the world of Autism Spectrum Disorder (ASD), a neurodevelopmental condition manifesting a wide spectrum of symptoms and abilities. The understanding of ASD has evolved over the years, recognizing it as a spectrum disorder.
But, is autism a spectrum disorder? What does it mean? How does it impact the life of an individual? How can we support those affected by ASD? Let’s delve into unraveling the mysteries of ASD, from its origin to the various autism treatment approaches, and how it affects individuals at different stages of life.
Table of Contents
Chapter 1: Is Autism a Spectrum Disorder?
Chapter 2: Autistic Spectrum Disorder and Related Conditions
Chapter 3: Autistic Spectrum Disorder and Co-Occurring Conditions: AuDHD, PDA & RSD
Chapter 4: Diagnostic Criteria for ASD
Chapter 5: Spectrum of Abilities and Challenges
Chapter 6: Risk Factors and Causes of ASD
Chapter 7: Living with ASD: Personal, Academic, Work and Social Implications
Chapter 8: How to Treat Autism: Autism Spectrum Disorder Treatment Approaches
Key Takeaways
- Understanding Autism Spectrum Disorder involves recognizing the range of symptoms, from learning difficulties to sensory sensitivities and repetitive behaviors.
- Diagnosis is based on behavioral autism assessments utilizing various tools, while early diagnosis enables timely access to interventions and therapies for autism that improve outcomes for individuals with the condition.
- Successful individuals demonstrate the importance of self-regulation, coping skills, and support in achieving their goals.
Chapter 1
Is Autism a Spectrum Disorder?

These signs typically appear between the ages of 1.5 to 3 years and may include:
- Learning difficulties, which may include challenges in reading, writing, and understanding complex concepts
- Sensory sensitivities, where certain sounds, textures, tastes, and lights can be overwhelming or uncomfortable
- Restricted interests, meaning a deep, intense focus on specific topics or activities
- Repetitive behaviors, such as hand-flapping, rocking, or repeating words and phrases
- Difficulties with transitions and changes in routine, which can lead to distress or anxiety
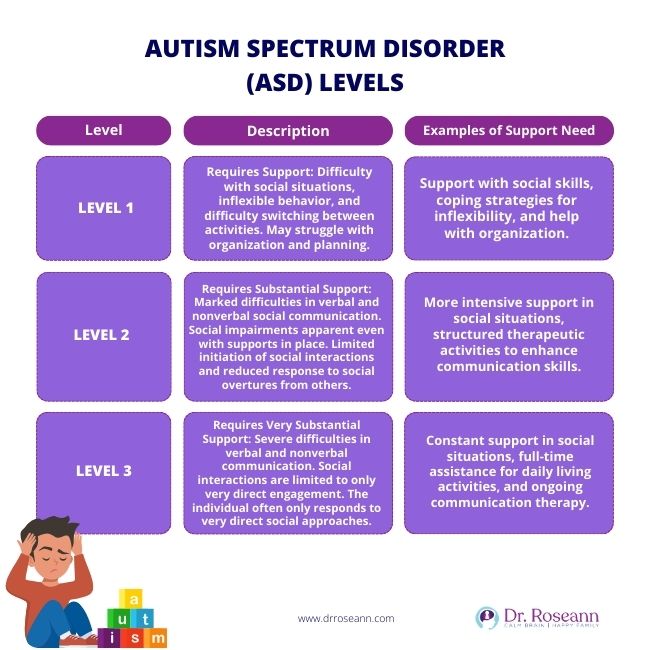
Individuals with ASD exhibit a vast array of variances in severity and functioning. Some individuals may exhibit low functioning, characterized by significant challenges in communication and social interaction, along with repetitive and restrictive behaviors. This may limit their ability to function independently and may require constant support and care.
On the other hand, some individuals may demonstrate high functioning, where they exhibit milder symptoms and can function independently with minimal help. They may possess unique strengths such as exceptional memory or specialized skills in specific areas.
Signs of ASD often surface before a child’s first birthday, and symptoms usually stabilize by the time the child is 2 or 3 years old. These early signs may include reduced eye contact, lack of response to their name, or indifference to caregivers. An early diagnosis is crucial for early intervention and support. Research shows that autism in girls is more common than autism in boys (Dworzynski et al., 2012).
It allows for the implementation of therapies and interventions that can significantly improve the child's development and quality of life. Moreover, early diagnosis and intervention can help the child develop important skills necessary for social interaction, communication, and independent living.
ASD is primarily classified into ‘syndromic autism’ and ‘non-syndromic autism’. Syndromic autism, where ASD is a characteristic within a broader medical condition, represents about 25% of ASD cases.
Non-syndromic autism is the more common form and isn’t associated with other syndromes. Mental health is a significant aspect to consider when addressing the needs of individuals with ASD, as they may experience co-occurring mental health conditions.
Chapter 2
Autistic Spectrum Disorder and Related Conditions
Childhood disintegrative disorder, a rare condition characterized by a significant loss of previously acquired skills in multiple areas of development, is now considered part of ASD. This disorder, also known as Heller's syndrome, is marked by a period of normal development for at least two years, followed by a significant loss of skills in at least two areas of development.
These areas may include language, social skills, play, motor skills, or bowel and bladder control. The exact cause of childhood disintegrative disorder is unknown, but it's considered a part of the broader ASD due to its similarities with other conditions on the spectrum. Despite its rarity, understanding and acknowledging childhood disintegrative disorder within the ASD context is crucial for a comprehensive ASD treatment plan and diagnosis, which could include the use of a QEEG brain map.
To elaborate, syndromic autism refers to cases where autism is part of a larger syndrome or medical condition. Some of these syndromes include Fragile X syndrome, Tuberous sclerosis, and Rett syndrome. These syndromes often have other symptoms and characteristics, making the diagnosis and treatment for autism spectrum disorder more complex.
On the other hand, non-syndromic autism, which accounts for the majority of ASD cases, is when autism is the primary diagnosis and is not associated with another syndrome or medical condition.
Chapter 3
Autistic Spectrum Disorder and Co-Occurring Conditions
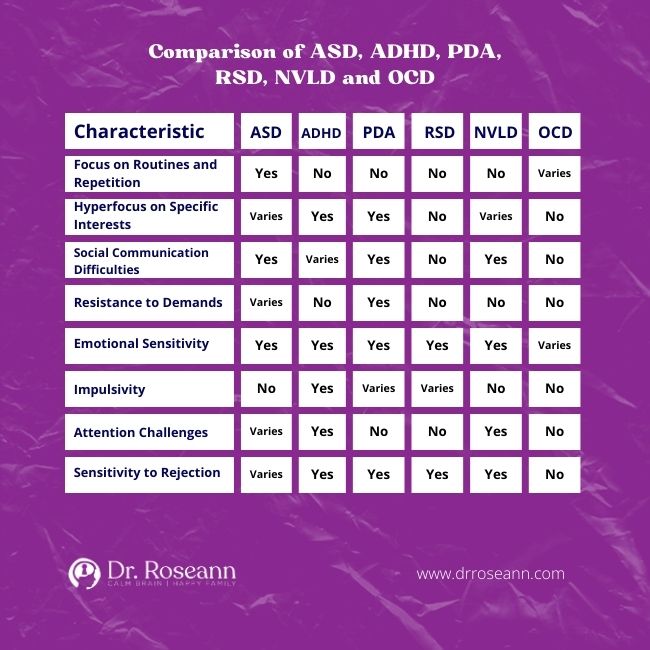
Several co-occurring conditions are commonly seen with ASD including Obsessive Compulsive Disorder (OCD), Attention Deficit Hyperactivity Disorder (ADHD), Pathological Demand Avoidance (PDA), Non-Verbal Learning Disorder (NVLD), Sensory Processing Disorder (SPD), and other conditions like Failure to Launch and Executive Functioning Issues.
Autism and Obsessive Compulsive Disorder
Autism Spectrum Disorder and Obsessive-Compulsive Disorder are distinct neurodevelopmental conditions, yet they can coexist and share certain traits, such as repetitive behaviors. ASD is characterized by challenges in social communication and sensory sensitivities, while OCD involves intrusive thoughts and compulsive behaviors driven by anxiety.
Although individuals may be diagnosed with both disorders, a comprehensive evaluation by healthcare professionals is essential to differentiate and address the specific needs associated with each condition.
Autism and Pathological Demand Avoidance (PDA)
Pathological Demand Avoidance is an informal term associated with extreme demand avoidance within the autism spectrum, though it is not officially recognized as a separate diagnostic category.
Individuals with PDA, often within the autism spectrum, exhibit pervasive and disproportionate resistance to everyday demands, coupled with heightened anxiety. This term is commonly used to describe those who employ social strategies to avoid tasks and expectations, masking compliance while covertly resisting.
While PDA shares characteristics with Autism Spectrum Disorder, it emphasizes an extreme pattern of demand avoidance, and individuals displaying PDA traits are often diagnosed within the broader autism spectrum, underlining the importance of recognizing and addressing the diverse manifestations of ASD.
Autism and Non-Verbal Learning Disorder
Autism spectrum disorder and Non-Verbal Learning Disorder are distinct neurodevelopmental conditions with differing characteristics. ASD is characterized by challenges in social communication, repetitive behaviors, and specific interests, whereas NVLD primarily involves difficulties in non-verbal skills, such as spatial awareness and interpreting non-verbal cues, alongside strengths in verbal abilities.
Although both conditions may share some social communication challenges, they have unique features, and co-occurrence is possible but requires careful assessment to address the specific needs associated with each disorder. Individuals with ASD often exhibit a broader range of social and behavioral difficulties, while those with NVLD face more specific challenges related to non-verbal processing.
Autism and Sensory Processing Disorder (SPD)
Autism spectrum disorder and Sensory Processing Disorder are related conditions with overlapping features, particularly in sensory sensitivities, but they have distinct characteristics. ASD is defined by challenges in social communication and interaction, along with repetitive behaviors, where sensory sensitivities are one aspect of a broader set of difficulties.
On the other hand, SPD focuses specifically on atypical responses to sensory stimuli and their impact on daily functioning. While individuals with ASD often experience sensory sensitivities, SPD emphasizes sensory issues as its primary feature. Co-occurrence is not uncommon, and addressing sensory challenges within the context of autism requires a comprehensive understanding of both conditions for effective intervention.
Autism and Failure to Launch
“Failure to launch” is a term used to describe a situation where individuals, typically in late adolescence or early adulthood, struggle to achieve the expected level of independence and self-sufficiency.
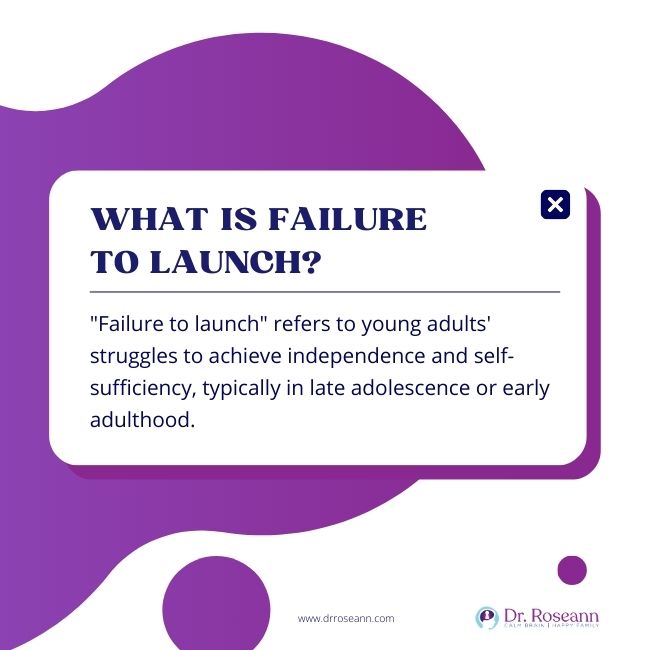
While not a formal diagnostic term, this phenomenon is often associated with challenges in education, employment, and establishing independent living arrangements. In the context of autism spectrum disorder (ASD), individuals may face additional difficulties related to social and communication challenges, executive functioning, and sensory sensitivities.
The transition to adulthood for individuals with ASD can be particularly complex, requiring tailored support, vocational training, and targeted autism interventions to address their unique needs. A multidisciplinary approach to autism spectrum treatment is recommended to provide comprehensive support and facilitate a successful transition to adulthood for individuals with ASD experiencing failure to launch.
Autism and Executive Functioning Issues
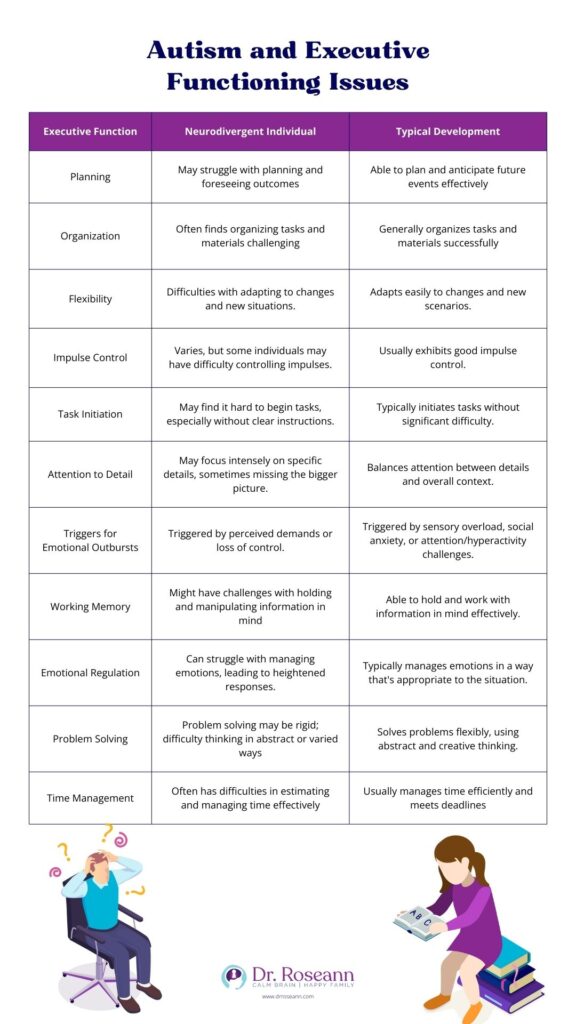
Individuals with Autism Spectrum Disorder or neurodivergence often experience challenges in executive functioning, which encompasses cognitive processes like planning, organization, flexibility, impulse control, and initiation of tasks.
These executive functioning difficulties can impact various aspects of daily life, including academic performance, social interactions, and independent living. In academic settings, challenges may arise in tasks requiring organization and sustained attention. Social interactions may be affected by difficulties in understanding social cues and adapting to changing situations.
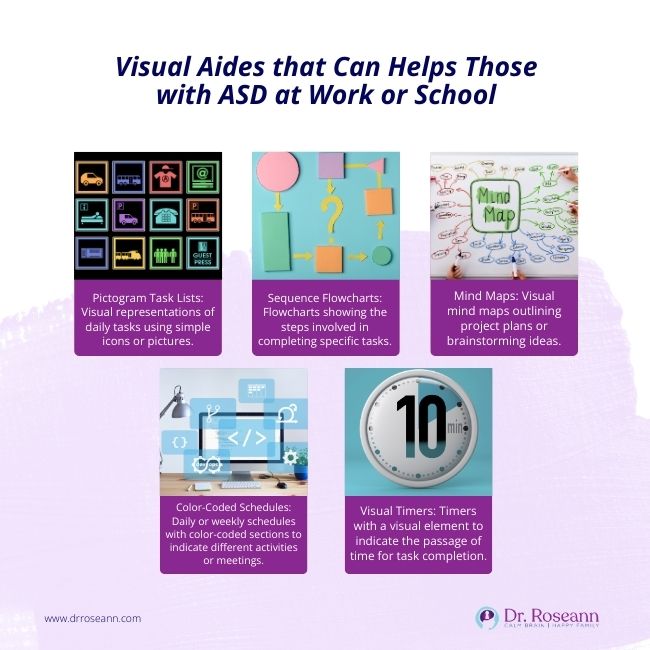
To address these issues, interventions such as structured environments, visual supports, social skills training, and task breakdowns are often employed to provide tailored support and enhance the ability of individuals with ASD to navigate daily tasks, academic challenges, and social scenarios.
Autism and Attention Deficit Hyperactivity Disorder (ADHD)
Autism spectrum disorder and Attention Deficit Hyperactivity Disorder are separate neurodevelopmental conditions, each characterized by unique features. ASD is primarily marked by challenges in social communication and engagement, along with repetitive behaviors and sensory sensitivities.
ADHD, on the other hand, involves persistent patterns of inattention, hyperactivity, and impulsivity, often affecting executive functions. While both disorders may share certain traits, such as attention difficulties, they differ in their core characteristics, making a comprehensive evaluation essential for accurate diagnosis and tailored intervention.
In some cases, individuals may receive both ASD and ADHD diagnoses, highlighting the importance of addressing the distinct challenges associated with each condition when they co-occur.
What is AuDHD?
AuDHD is a term that emerges at the intersection of Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. This unique blend encapsulates individuals who exhibit symptoms of both disorders, creating a distinctive profile that requires nuanced understanding and targeted interventions (Hanna Bertilsdotter Rosqvist et al., 2023).
AuDHD Meaning in Adults and Coping with Challenges
Autism ADHD represents a complex interplay of characteristics associated with both autism and ADHD. The term emphasizes the developmental trajectory of individuals who grapple with challenges related to attention, hyperactivity, and aspects typical of autism, shaping a unique clinical presentation.
What Does AuDHD Mean in Kids?
AuDHD signifies a co-occurrence of symptoms related to inattention, hyperactivity, and impulsivity, along with characteristics typical of autism. This includes difficulties in social communication, sensory sensitivities, and repetitive behaviors. Kids with AuDHD may navigate a more intricate neurodevelopmental landscape, blending elements of both disorders.
AuDHD Symptoms
The common AuDHD symptoms in children include:
- Challenges in sustaining attention
- Hyperactivity and restlessness
- Impulsivity in decision-making.
- Difficulties in social communication
- Sensory sensitivities
- Repetitive behaviors or intense focus on specific interests
- Difficulty managing emotions
- Intense emotional reactions to stimuli
- Organization and planning difficulties
- Impaired working memory
AuDHD vs. ADHD
While AuDHD shares some symptoms with ADHD, the presence of autistic traits sets it apart. Unlike typical ADHD, AuDHD may involve more profound challenges in social communication and a heightened sensitivity to sensory stimuli. Distinguishing between the two is crucial for tailoring interventions to address the specific needs of individuals with AuDHD.
PDA AuDHD
Pathological Demand Avoidance within the context of AuDHD further complicates the clinical picture. Individuals with PDA AuDHD may exhibit extreme avoidance of demands or requests, driven by anxiety and a need to maintain control. This aspect underscores the importance of recognizing and addressing the nuanced challenges that arise from the intersection of autism and ADHD.
Rejection Sensitive Dysphoria (RSD) and ASD
Those that have “big reactions” to real or perceived criticism or rejection, might also have rejection sensitive dysphoria or RSD. Kids and people with RSD are prone to emotional and behavioral dysregulation. These dysregulated kids can be hard to parent because their high emotionality gets in the way of learning.
The Evolution of ASD Classification
The concept of Autism Spectrum Disorder dates back to the 1970s, introduced by psychiatrist Lorna Wing. The formal recognition of autism as a spectrum began with its inclusion in the DSM-IV, a diagnostic manual published by the American Psychiatric Association.
The guidelines in DSM-5, the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders, adopted a spectrum approach to autism, consolidating previous separate diagnoses into a single umbrella category of ASD. The 11th iteration of the International Classification of Diseases (ICD-11) follows a similar approach, recognizing the spectrum characteristics of the disorder, and emphasizing difficulties in social communication.
Variability in ASD Symptoms
ASD symptoms vary among individuals, with differences in behavior, neurodevelopment, and severity. This variability can make the diagnosis and understanding of the condition more complex. There’s also a possibility of gender-specific patterns, where variations in symptom patterns exist between females and males with ASD.
Interestingly, the symptoms of ASD can change over time. Research indicates that the severity of autism symptoms can vary notably between ages 3 and 11 (Waizbard‐Bartov et al., 2022). It has been observed that some children may experience improvement and a decrease in symptom severity as they grow older.
Common Signs and Symptoms at Every Developmental Stage: Young Children, School-Age, Adolescents and Teens and Adults
As early as the first year of a child’s life, ASD symptoms may manifest as:
- Reduced eye contact
- Lack of response to their name
- Indifference to caregivers
- Sudden withdrawal or aggression
- Loss of language skills
These early signs may also be present in other developmental disabilities, making accurate diagnosis crucial for appropriate support and intervention strategies for autism.
In older children and teens, ASD may manifest through difficulties in subtle communication, such as:
- Trouble understanding tone of voice, facial expressions, or body language
- Challenges in grasping figures of speech, humor, or sarcasm
- Difficulties in forming friendships with peers
Chapter 4
Diagnostic Criteria for ASD

Behavioral assessments form the diagnostic criteria for ASD, playing a critical role in advancing behavior, skills, and language development for individuals with ASD, thus resulting in improved outcomes. Various diagnostic tools are used for assessing Autism Spectrum Disorder, including:
- CARS (Childhood Autism Rating Scale)
- SCQ (Social Communication Questionnaire)
- ADI-R (Autism Diagnostic Interview-Revised)
- DISCO (Diagnostic Interview for Social and Communication Disorders)
- ADOS (Autism Diagnostic Observation Schedule)
The initial step in pursuing an assessment for ASD typically involves initiating the process with the pediatrician, who assesses developmental milestones. It’s crucial to understand that ASD traits frequently intersect with symptoms of other disorders, creating complexities in conventional diagnostic processes. In such cases, consulting autism specialists in developmental and behavioral pediatrics can be helpful.
Behavioral Assessments in Diagnosis
It is important to assess how autistic behaviors are impacting a child or teen at home, school, socially, or in life in general so the right supports can be put into place. This includes evaluating how they interact with their family members, peers, and teachers, how they perform academic tasks, and how they manage daily activities such as eating, dressing, and grooming.
It also involves observing their behavior in different social settings, such as playgrounds, classrooms, and community events. This comprehensive assessment can help identify their specific challenges and areas where they need support. It can also highlight their strengths and abilities, which can be harnessed to help them reach their full potential. The ultimate goal is to create a supportive environment that allows them to thrive and lead fulfilling lives.
Behavioral assessments, including the following, are critical in diagnosing Autism Spectrum Disorder:
- Autism Diagnostic Observation Schedule (ADOS)
- Autism Diagnostic Interview (ADI)
- Childhood Autism Rating Scale (CARS)
- Functional Behavior Assessments (FBA)
These assessments evaluate social interactions, communication skills, and restricted or repetitive behaviors. The essential behaviors typically noted during an ASD diagnostic behavioral assessment include:
- Social communication skills
- Restrictive and repetitive behaviors
- Language and communication abilities
- Cognitive abilities
- Motor skills
Such assessments are widely acknowledged as reliable tools for an autism diagnosis, specifically for Autism Spectrum Disorder.
Importance of Early Diagnosis
Early diagnosis and intervention are vital in disease control, as they foster the development of behavior, skills, and language for individuals with ASD, thus leading to better outcomes.
Early identification of Autism Spectrum Disorder offers the chance for early intervention, which has been demonstrated to enhance:
- developmental outcomes
- improve daily living skills
- social behavior
- overall outcomes for individuals with ASD.
While there is no cure for autism spectrum disorder, intensive early intervention can significantly impact the lives of many children by enhancing their development and increasing the potential for improved life experiences and outcomes. Early diagnosis is crucial as it enables timely access to interventions and therapies.
Chapter 5
Spectrum of Abilities and Challenges

The autism spectrum covers a broad scope of abilities and challenges, spanning from high-functioning ASD to intellectual disability. There’s a broad range of abilities and challenges within the autism spectrum, including high-functioning ASD, formerly known as Asperger’s syndrome, to intellectual disability, highlighting the unique strengths of individuals with ASD.
High Functioning ASD: Formerly Asperger's Spectrum Disorder
High-functioning Autism Spectrum Disorder relates to those on the spectrum who demonstrate milder symptoms and can function independently with minimal help. It was historically categorized as Asperger’s Spectrum Disorder, a term coined by Hans Asperger in 1944 and subsequently included in diagnostic manuals in 1994.
The primary differentiating factor between high-functioning ASD and Asperger’s syndrome is that individuals with Asperger’s generally do not exhibit a delay in language skills development. The impact of high-functioning ASD on cognitive abilities varies among individuals, though research suggests a genetic correlation between autism risk and mental ability (Happé & Ronald, 2008).
Intellectual Disability and ASD
Intellectual Disability in Autism Spectrum Disorder is marked by impairments in intellectual functioning and adaptive skills. This co-occurring condition can vary in severity, affecting different aspects of an individual’s life.
Individuals with both ASD and intellectual disabilities may encounter:
- significant intellectual and adaptive functioning deficits
- heightened vulnerability to co-occurring psychiatric disorders
- potentially distinct sensory processing issues in comparison to those with ASD only.
Strengths Unique to the Autism Spectrum
Individuals with ASD often exhibit unique strengths, showcasing their exceptional abilities that transcend the challenges posed by the disorder. These strengths are a testament to their resilience and adaptability, shining a light on their potential to excel in various areas. This is a crucial aspect of understanding ASD, as it emphasizes the fact that despite the difficulties they may face, individuals with ASD are also capable of extraordinary achievements, often outperforming their neurotypical peers in certain areas. including:
- Attention to detail
- Robust visual perception
- Long-term memory skills
- Direct communication
- Talents in areas like math, computer, music, and art
- Visual thinking
- Honesty
- Intense focus
- Strong cognitive as well as visual thinking skills
ASD can lead to heightened capabilities in aspects like pattern recognition and attention to detail.
Numerous individuals with autism possess an innate talent for identifying recurring patterns and demonstrate robust analytical skills.
Chapter 6
Risk Factors and Causes of ASD

The development of ASD may be influenced by genetic and environmental factors, affecting the progression of the condition.
Genetic Influences on ASD
Genetics significantly influence the development of ASD, with many genes associated with the condition. Various genes such as:
- 7q36
- 16p13
- 18p11
- 15q24
- 12q24
- MTHFR (A1298C and C667T)
- PLEKHA8
- PRR25
- FBXL13
- VPS54
- SLFN5
- SNCAIP
have been linked to the development of Autism Spectrum Disorder (ASD). Mutations in these genes can disrupt normal brain development and function, affecting synaptic communication, neuronal connectivity, and gene regulation.
There is a correlation between specific genetic disorders and an elevated risk of ASD, including conditions such as:
- Smith-Lemli-Opitz syndrome
- Tuberous sclerosis
- Fragile X syndrome
- Rett syndrome
- Phelan-McDermid syndrome
Environmental Risk Factors
Prenatal exposure to certain substances, an environmental factor, may contribute to the development of ASD. Exposure to particular substances during pregnancy, such as antiepileptic drugs like valproic acid and pesticides, has been correlated with an increased risk of Autism Spectrum Disorder.
Recent research indicates a potential link between prenatal environmental exposure to substances such as pesticides, airborne pollutants, and acetaminophen with Autism Spectrum Disorder (Wong et al., 2015).
Infectious Disease and Autism
Certain infectious diseases, like rubella, are associated with a heightened risk of ASD. The heightened risk of developing Autism Spectrum Disorder has been associated with prenatal exposure to rubella, attributed to the potential influence of the virus on the central nervous system’s development during crucial stages of fetal growth.
Maternal immune activation (MIA), especially stemming from infections, elevates the likelihood of Autism Spectrum Disorder (ASD) in the offspring.
There is also a high rate of PANS and PANDAS in individuals with ASD. Ruling out infections and toxins as contributors to neuroinflammation is important.
Chapter 7
Living with ASD: Personal, Academic, Work and Social Implications

Academics and The Spectrum Autism
Specialized support and accommodations may be necessary for academic success in individuals with ASD. Students with ASD frequently confront academic hurdles including challenges with developmental delays, particularly:
- Writing
- Organization and schedules
- Language development and communication
- Cognitive processing delays
- Sensory perception issues
- Social skills deficits
- Resistance to change in daily routines
Educators can facilitate the inclusion of students with ASD in mainstream classrooms by implementing strategies such as:
- Establishing routines
- Providing visual supports
- Using clear and concise language
- Allowing sensory breaks
- Fostering social skills development
- Collaborating closely with support professionals, particularly an autism spectrum therapist
The Autistic Neurodivergent Brain and The Workplace
The distinctive cognitive profile of individuals with ASD can provide both challenges and opportunities in the professional environment. Strengths may be evident in their heightened attention to detail and the potential for exceptional focus on specialized tasks, which can be beneficial in fields that demand precision. However, challenges may arise from difficulties in social interactions, anxiety, perfectionism, and uneven abilities, potentially impacting job performance in roles that necessitate frequent communication or multitasking.
Individuals with ASD may find success in job sectors that align with their cognitive strengths, including computer coding, data analysis, cybersecurity, IT, accounting, and roles that require precision and attention to detail such as pharmacy technician, web designer, network engineer, forensic accountant, CPA, tax preparation specialist, bookkeeper, and billing specialist.
Navigating Social Interaction
While social interaction can be challenging for individuals with ASD, certain strategies and support can aid in improving communication and relationships.
Recommended communication strategies to assist individuals with ASD in social interactions include:
- Limiting speech
- Speaking slowly
- Being specific
- Using nonverbal language
- Recognizing repetitive behavior
- Utilizing visual communication aids
- Using technology to facilitate communication
- Encouraging social interaction and play therapy for autism
- Imitating each other
- Focusing on nonverbal communication
- Giving time for the individual to talk.
Social skills training can benefit individuals with ASD by equipping them with the capacity to:
- Engage in conversation
- Share
- Play
- Collaborate with typical peers
It can enhance their quality of life and facilitate the structured development of social skills.
Support Systems for Autistic Individuals
Family, friends, and professionals providing autism services form crucial support systems that enable individuals with ASD to thrive in diverse life aspects. These support systems provide emotional, functional, and practical assistance to individuals with ASD, fostering their overall well-being and development.
Family and friends often provide a safe and understanding environment, where individuals with ASD can express themselves freely and gain emotional support. They can also assist in day-to-day tasks, and promote social interaction and communication skills.
Professional services from an autism therapist, on the other hand, offer specialized support tailored to the unique needs of each individual with ASD. This may include child autism therapy techniques, educational support, and employment assistance, among others. These autism therapy services are designed to enhance the skills of individuals with ASD, enabling them to lead fulfilling and independent lives.
Furthermore, these support systems also play a vital role in raising awareness and promoting acceptance of ASD in society. They contribute to building a more inclusive community, where individuals with ASD are recognized, appreciated, and respected for their unique abilities and perspectives. Numerous support systems are accessible for individuals with ASD, such as:
- Medicaid
- GRASP
- Speech and Language Therapy
- Online support groups
- Autism Response Team (ART)
- Asperger/Autism Education Network (ASPEN)
Families and friends can provide support to individuals with ASD by helping others understand autism, being effective allies, supporting the development of social skills, and offering assistance. Professional services are of paramount importance in providing support for individuals with Autism Spectrum Disorder.
They are instrumental in assisting with daily activities, communication, and social skills, and offering employment support to help autistic adults find and maintain jobs through workplace accommodations and assistance.
Chapter 8
How to Treat Autism: Autism Spectrum Disorder Treatment Approaches
To treat autism naturally, the right strategies encompass non-pharmacological approaches, diet and lifestyle adjustments, and innovative therapies like neurofeedback and PEMF. Non-pharmacological interventions and biomedical treatments for autism, including psychological, educational, skill-building, and behavioral interventions for autism, are frequently utilized as the first-line approaches for individuals with ASD.
The best treatment for autism includes the use of various diagnostic tools to assess the condition, such as:
- CARS (Childhood Autism Rating Scale)
- SCQ (Social Communication Questionnaire)
- ADI-R (Autism Diagnostic Interview-Revised)
- DISCO (Diagnostic Interview for Social and Communication Disorders)
- ADOS (Autism Diagnostic Observation Schedule)

Autism behavioral therapy and educational interventions, which are non-pharmacological strategies, are often considered the primary autism treatments and therapies, and not autism spectrum medications like Prozac. These autism spectrum disorder treatments and interventions involve evaluating social interactions, communication skills, and restricted and repetitive behaviors.
Interventions such as:
- Speech and Language Therapy
- Cognitive Behavioral Therapy for autism (CBT)
- Social Behavior Interventions
- Applied Behavioral Analysis (ABA therapy)
Therapeutic interventions are particularly beneficial for very young children with ASD during childhood and adolescence. They work better than any medication for autism, which alters brain development.
Diet, Lifestyle and Exercise
Autism management and enhancing overall well-being can be influenced by diet, lifestyle, and exercise. The potential impact of specific diets, such as a gluten-free and casein-free diet, on ASD symptoms is a matter of ongoing debate.
Lifestyle factors have a significant impact on ASD symptoms. Maternal smoking during pregnancy has been linked to an elevated risk of ASD, possibly due to effects like placental insufficiency or reduced fetal blood flow. Regular exercise has demonstrated multiple benefits for individuals with Autism Spectrum Disorder, such as improving motor skills, reducing maladaptive behaviors, and decreasing anxiety levels.
Magnesium and How it Helps Autism
Some ASD symptoms may improve with magnesium supplementation. Magnesium is crucial for nerve transmission, neuromuscular conduction, and regulating neurotransmitter signaling in the brain. The consequences of magnesium deficiency may include neuroinflammation, dysfunction of the blood-brain barrier, and the potential to contribute to neurological issues such as anxiety, stress, headaches, depression, weakness, tremors, seizures, and arrhythmias, which can further complicate the challenges experienced by individuals with ASD.
Neurofeedback, PEMF, and Self-Regulation of Autism
Innovative autism therapies, such as neurofeedback and PEMF, hold potential in aiding individuals with ASD to self-regulate and manage their symptoms. Neurofeedback therapy is a non-invasive method designed to assist individuals in regulating their brain activity. It’s the best therapy for autism spectrum disorder because it involves monitoring brainwave activities and delivering immediate feedback, typically through visual or audio prompts.
Pulsed Electromagnetic Field (PEMF) therapy for autism is a non-invasive medical treatment that utilizes intermittent, current pulse-generated magnetic field pulses over a short time frame to stimulate and exercise cells, aiding in the resolution of cellular dysfunction and the treatment of autism, as well as acute and chronic pain.
Behavioral and Parenting Strategies
Focusing on reinforcing desired behaviors with a consistent routine helps children learn and develop skills.

Chapter 9
Autism in Different Life Stages
Autism across different life stages brings distinctive challenges and growth opportunities, with success stories underscoring the importance of self-regulation and coping skills.
The primary objectives of natural treatment and autism therapy at home are to diminish deficits and family distress and to enhance the quality of life and functional independence.
Childhood and Adolescence
For ASD, childhood and adolescence are pivotal periods for intervention and support, as early intervention for autism fosters better outcomes. Children with ASD can greatly benefit from intensive special education programs and ASD therapy early in life. These interventions for autism can help kids develop important skills such as self-care, language, and job skills.
Adulthood and Aging
While adulthood and aging with ASD can bring forth new challenges, they also offer opportunities for growth and independence. Receiving a correct diagnosis of ASD as an adult can assist an individual in comprehending past difficulties, recognizing personal strengths, and seeking suitable support.
Autism Success Stories: Self-Regulation and Building Coping Skills
Success stories from individuals with ASD underscore the significance of self-regulation, coping skills, and support in attaining personal and professional objectives. These narratives are accessible through sources like CBS News, the Anxiety and Depression Association of America, and scholarly papers examining the requirements of individuals with Autism Spectrum Disorders.
How is autism considered a spectrum disorder?
Autism is considered a spectrum disorder due to the variation in symptoms experienced among different people, as well as the ability for symptoms to change over time. It affects individuals of all genders, races, ethnicities, and economic backgrounds.
What is considered a spectrum disorder?
Autism spectrum disorder (ASD) is a developmental disability caused by differences in the brain. It is considered a spectrum because it includes a range of linked conditions, and can vary greatly in terms of type and severity of symptoms. People of all genders, races, ethnicities, and economic backgrounds can be diagnosed with ASD.
What is the difference between spectrum and autism?
Autism is now included in the umbrella term Autism Spectrum Disorder (ASD), which encompasses the different levels of autism. This change was made by the American Psychiatric Association in 2013.
What are the 5 different types of autism?
Autism comes in many forms, with five distinct categories of diagnosis: Autistic Disorder, Asperger Syndrome, Childhood Disintegrative Disorder, Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), and Rett Syndrome. Each type of autism has its own set of characteristics and symptoms.
How long can a child with autism live?
Individuals with autism typically live for around 39 years, with the majority succumbing to health complications around 20 years earlier than those without autism. That’s why early intervention and autism counseling are crucial.
Is there an autism cure?
There is no magic wand to cure autism spectrum disorder, but a child can thrive and live a fulfilling life by understanding and managing the condition through early intervention and support strategies, preferably with the guidance of experts from reputable autism treatment centers.
How do you treat autism?
The treatment of autism spectrum disorder involves a personalized, multidisciplinary approach, including speech and language therapy, occupational therapy, educational support, and behavioral treatment for autism. Such ASD treatments aim to enhance communication, social interactions, and adaptive behaviors, with early intervention being crucial for overall improvement in functioning and quality of life. These are helpful to those looking for ways how to cure autism.
What is the best treatment for autism spectrum disorder?
The best treatment for ASD in adults and kids involves a personalized, multidisciplinary approach, including early intervention, Applied Behavior Analysis therapy (ABA), speech and language therapy, occupational therapy, and social skills training, tailored to the individual's unique strengths and challenges, with neurofeedback, PEMF, magnesium supplements, and ongoing family involvement and consultation with healthcare professionals for effective support.
What is ABA therapy for Autism?
The Applied Behavior Analysis interventions for autism or ABA autism therapy involve systematically assessing and modifying observable behaviors using positive reinforcement, prompting, task analysis, and collaboration with caregivers to achieve individualized, measurable goals.
Where do I get autism spectrum disorder help?
For help with autism spectrum disorder, individuals and families can consult with pediatricians, developmental pediatricians, psychologists, speech and language therapists, occupational therapists, and behavioral therapists. Aside from psychotherapy for autism, there’s also a need for special education services, autism support organizations, and community mental health autism spectrum disorder services. Aside from autism disorder treatment therapy, finding early intervention programs and utilizing reliable online resources to access a range of assessments, ASD interventions, and support options tailored to individual needs can also help.
Citations
Dworzynski, K., Ronald, A., Bolton, P., & Happé, F. (2012). How Different Are Girls and Boys Above and Below the Diagnostic Threshold for Autism Spectrum Disorders? Journal of the American Academy of Child & Adolescent Psychiatry, 51(8), 788–797. https://doi.org/10.1016/j.jaac.2012.05.018
Hanna Bertilsdotter Rosqvist, Hultman, L., Sofia Österborg Wiklund, Nygren, A., Storm, P., & Sandberg, G. (2023). Naming ourselves, becoming neurodivergent scholars. Disability & Society, 1–20. https://doi.org/10.1080/09687599.2023.2271155
Happé, F., & Ronald, A. (2008). The “Fractionable Autism Triad”: A Review of Evidence from Behavioural, Genetic, Cognitive and Neural Research. Neuropsychology Review, 18(4), 287–304. https://doi.org/10.1007/s11065-008-9076-8
Hertz-Picciotto, I., Croen, L. A., Hansen, R., Jones, C. R., van de Water, J., & Pessah, I. N. (2006). The CHARGE Study: An Epidemiologic Investigation of Genetic and EnvironmentalFactors Contributing to Autism. Environmental Health Perspectives, 114(7), 1119–1125. https://doi.org/10.1289/ehp.8483
Waizbard‐Bartov, E., Ferrer, E., Heath, B., Rogers, S. J., Nordahl, C. W., Solomon, M., & Amaral, D. G. (2022). Identifying autism symptom severity trajectories across childhood. Autism Research. https://doi.org/10.1002/aur.2674
Wong, C. T., Wais, J., & Crawford, D. A. (2015). Prenatal exposure to common environmental factors affects brain lipids and increases risk of developing autism spectrum disorders. European Journal of Neuroscience, 42(10), 2742–2760. https://doi.org/10.1111/ejn.13028
Dr. Roseann is a mental health expert in Neurodivergence who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind What Is Asperger Syndrome?
- Parents Are Your Kid's Meltdowns a Sign of Rejection Sensitive Dysphoria?
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024