Raising children may be chaotic sometimes, but it's a beautiful journey. Having children and teens with mental health and behavioral issues is no easy task. Even then, know that you're not alone in this wild ride.
It is even more challenging when you are uncertain what is behind your child’s behavior. You may be puzzled by the low motivation, difficulties focusing or rigidity and wondering if it could be ADHD, ASD or PDA. Well you aren’t alone.
Each can affect mood, stress, and behavior in different ways but also have many similarities too. Let's explore the link between Attention-Deficit Hyperactive Disorder, autism, and Pathological Demand Avoidance, as these conditions intertwine in complex ways.
Is it ADHD or something else?
What is Pathological Demand Avoidance?
In the vast realm of Autism Spectrum Disorder, a fascinating and distinct profile emerges called Pathological Demand Avoidance or PDA. PDA is a proposed subtype of autism that warrants our attention. Children and teens with the PDA profile of autism have central difficulty processing and responding to demands placed upon them.
Unlike individuals with other forms of autism, they display an extreme extent of demand avoidance behaviors. Even the ordinary demands of life can trigger anxiety-based needs for control, leading to a relentless urge to avoid tasks or directives. This avoidance is not driven by defiance but rather by an overwhelming need to protect themselves from the distress associated with immediate demands.
Recognizing PDA traits can be crucial for understanding and supporting those who experience this condition. PDA kids may exhibit an intolerance of uncertainty, excessive mood swings, and a strong need for autonomy (O'Nions & Eaton, 2020). Their anxiety levels can escalate quickly, and they may experience panic attacks when faced with overwhelming demands.
One of the key features of PDA is the avoidance of tasks and the resistance to authority figures. Children and teens with PDA struggle with traditional strategies that are effective for those with other forms of autism. Their condition calls for a shift in approach and the development of social processes that respect their need for autonomy and freedom of choice.
It is essential to recognize that PDA behaviors are not rooted in defiance but rather in a rational demand avoidance driven by anxiety and a need for control. These kids have a distinct profile within the autism spectrum, and acknowledging this can pave the way for better support and management.
Symptoms and Characteristics of Autism and Pathological Demand Avoidance
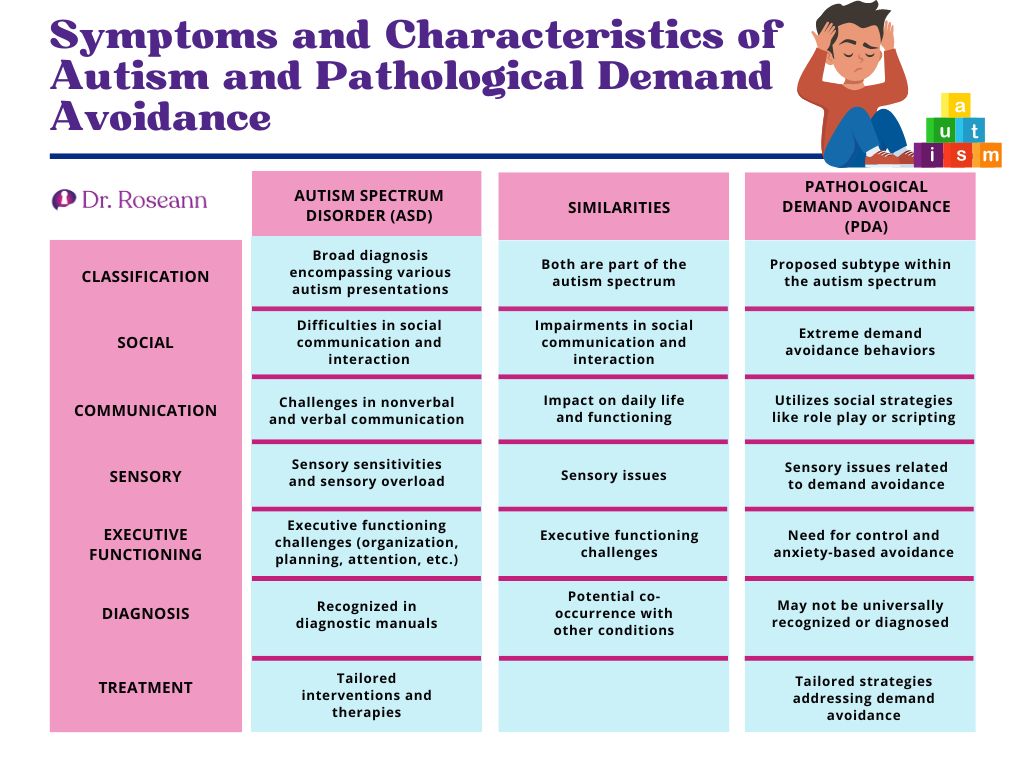
Understanding the symptoms and characteristics of autism and PDA is crucial for parents, caregivers, and healthcare professionals supporting children and teens on the autism spectrum. While autism and PDA share some similarities, they also exhibit distinct features that set them apart.
Autism, as a part of the autism spectrum, is characterized by social communication and interaction impairments. Autistic children may struggle to understand and use nonverbal communication cues, maintain eye contact, and engage in reciprocal conversations.
They may also experience challenges in navigating social situations and forming meaningful relationships. Sensory issues are another common feature of autism, where individuals may experience sensory overload or be hypersensitive to certain stimuli such as noises, lights, or textures.
On the other hand, PDA is proposed as a subtype of autism spectrum disorder. PDA kids exhibit extreme demand avoidance behaviors not rooted in defiance or oppositional defiant disorder.
Unlike autistic people, who may struggle with social situations, PDA kids have a distinct profile characterized by a strong need for control and anxiety-based avoidance of everyday demands (Woods, 2022). They may actively resist or avoid tasks, leading to a significant impact on their daily functioning.
While autism and PDA share impairments in social communication and interaction, the central difficulty for PDA children is their avoidance of demands rather than a lack of social skills. These kids may exhibit excessive mood swings and have difficulty coping with the ordinary demands of life. The diagnostic criteria for PDA are still being refined, and researchers continue to study the distinct features of this profile.
How Does ADHD and Attention Problems Fit into Pathological Demand Avoidance and Autism?
Let's throw another acronym into the mix: Attention Deficit Hyperactivity Disorder, or ADHD. ADHD is a neurodevelopmental condition that can coexist with both PDA and autism. While ADHD is a distinct disorder, it shares some overlapping features with PDA and autism, leading to potential diagnostic complexities and challenges in understanding individuals with multiple conditions.
In the context of PDA and autism, ADHD can further complicate a child's symptoms and behaviors. Children with PDA may exhibit characteristics of ADHD, such as difficulties with attention, impulsivity, and hyperactivity, which can exacerbate their extreme demand avoidance behaviors (Egan et al., 2020). It becomes challenging for them to engage in tasks or activities, which may lead to increased anxiety and stress.
Similarly, individuals with autism may also have ADHD, resulting in additional difficulties with attention, impulse control, and hyperactivity. It can impact their social interactions, communication skills, and ability to focus on tasks or follow instructions. The sensory issues common in autism and ADHD can further contribute to sensory overload and difficulties in sensory processing.
I remember a young girl, let's call her Kelly, who faced the challenges of having ADHD and PDA. Kelly's days were often filled with restlessness, difficulty focusing, and overwhelming anxiety caused by the demands of everyday life. It seemed like a constant struggle for her to navigate social interactions and complete tasks.
Her case was difficult to diagnose, but she got the interventions needed to manage her condition. Natural solutions such as neurofeedback, PEMF, and magnesium supplementation have greatly helped her.
Strategies for Supporting Kids with ADHD, Autism, and PDA Profile
There’s no need to fear if you suspect your child or teen of having ADHD and autism or PDA. Some strategies exist that can help manage and support them. While it's essential to consult with healthcare professionals for personalized advice, here are some helpful approaches to consider:
1. Develop a structured environment
Establishing a predictable routine and clear expectations can help children with ADHD, autism, and PDA feel more secure and in control. Providing visual schedules and using visual supports can assist in understanding and managing daily tasks.
2. Use social strategies
Teaching social skills and providing opportunities for practicing social interactions are crucial. They are also a long game that needs continual reinforcement. Role-playing scenarios and social stories can aid in understanding social cues and appropriate behavior in different situations.
3. Address sensory issues
Recognize and address sensory sensitivities or sensory overload experienced by individuals with autism and PDA. Create sensory-friendly environments, offer sensory breaks, and explore sensory integration techniques to help regulate sensory responses.
4. Support communication skills
Communication is the foundation of all relationships. It is important to keep communication flowing with our neurodivergent children. When communication is a physical challenge, it may be necessary to enhance communication abilities through various approaches, such as augmentative and alternative communication (AAC) systems, visual supports, and social communication interventions. Encourage using strategies like social scripts and narratives to facilitate effective communication.
5. Create a team of professionals
Seek guidance from healthcare professionals with expertise in autism and PDA, such as psychologists, occupational therapists, and speech-language pathologists. Their specialized knowledge can provide valuable insights and tailored strategies that can help your child thrive.
6. Foster self-regulation skills
Teach self-regulation techniques, such as deep breathing exercises and mindfulness practices, to help manage anxiety and emotional regulation. These strategies can empower individuals to cope with overwhelming situations and reduce the impact of demand avoidance behaviors.
7. Promote executive functioning skills
Develop strategies to support planning, organization, time management, and problem-solving skills. Visual organizers and breaking tasks into manageable steps can aid individuals in completing tasks and building independence around executive functioning.
8. Encourage engagement in special interests
Recognize and incorporate special interests as motivators and tools for engagement. Special interests provide a sense of purpose, increase intrinsic motivation, and facilitate learning.
9. Foster a supportive network
Involve parents, caregivers, and educators in understanding and implementing strategies for managing autism and PDA. Encourage collaboration, sharing experiences, and support from communities and organizations like our Natural Parenting Solutions Facebook Group.
10. Consider individual needs
Recognize that each individual with autism and PDA has unique strengths, challenges, and preferences. Tailor interventions and strategies to meet their specific needs, focusing on promoting their well-being and enhancing their quality of life.
As we navigate the intricate world of autism, PDA, and ADHD, let us remember the importance of embracing neurodiversity and promoting inclusivity. Autistic individuals, including people with PDA, have unique strengths and perspectives that can enrich our society. By fostering a culture of acceptance, understanding, and support, we can enhance their quality of life and create a more inclusive world.
Our BrainBehaviorResetTM program is an integrative approach that combines neuroscience, psychology, and natural therapies to create personalized treatment plans for individuals with neurodevelopmental disorders. Through it, children and teens can access natural, comprehensive, evidence-based techniques tailored to their unique needs, including neurofeedback, PEMF, and nutritional guidance.
The goal is to empower children and teens to optimize their brain health and unlock their full potential, providing hope and support for those seeking holistic and practical approaches to managing neurodivergent conditions.
Parent Action Steps
✅ Understand the overlap and co-occurrence of ADHD, Autism, and PDA
✅ Recognize the common symptoms and characteristics of ADHD, Autism, and PDA
✅ Seek professional diagnosis and evaluation to determine the specific conditions present
✅ Implement tailored strategies for social communication and interaction challenges
✅ Address sensory issues and provide sensory support to alleviate overload
✅ Develop executive functioning skills through structured routines and organization techniques
✅ Consider neurofeedback, PEMF therapy, and magnesium supplements as natural solutions
✅ Support your child's mental health and well-being through therapy and counseling
✅ Connect with other parents and neurodivergent communities for advice and understanding.
✅ Take advantage of technology tools and apps to assist in everyday life and learning.
✅ Advocate for your child's needs within educational settings and get accommodations.
✅ Take our Solutions Matcher to get personalized help for your child
✅ Take the “Is it ADHD or something else?” quiz to know if your child has ADHD
Citations
Egan, V., Bull, E., & Trundle, G. (2020). Individual differences, ADHD, adult pathological demand avoidance, and delinquency. Research in Developmental Disabilities, 105, 103733. https://doi.org/10.1016/j.ridd.2020.103733
O’Nions, E., & Eaton, J. (2020). Extreme/“pathological” demand avoidance: an overview. Paediatrics and Child Health, 30(12), 411–415. https://doi.org/10.1016/j.paed.2020.09.002
Woods, R. (2022, April 7). Demand Avoidance Phenomena (“ Pathological ”/ Extreme ” Demand Avoidance): As a Social Construct. Openresearch.lsbu.ac.uk. https://openresearch.lsbu.ac.uk/item/8zq59
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.