A vast, often missing component in the treatment of Obsessive Compulsive Disorder (OCD) in children and adolescents is explaining what OCD is and how it affects the brains of kids and their parents. That means understanding how OCD impacts a child’s behavior and how easy it is to inadvertently accommodate or feed into a child’s obsessions or compulsions.
That means well-meaning parents accidentally providing too much comfort or saying things that feed their intrusive thoughts and repetitive behaviors instead of decreasing OCD symptoms. This is called accommodation and means that parents are feeding the “OCD monster.”
A highly experienced OCD therapist for children and teens should spend much of the first session not only evaluating your child's or teen's OCD but also explaining what obsessions and compulsions look like, the neuroscience of OCD, and what areas of the brain are affected, how OCD treatments work and what treatment looks like.
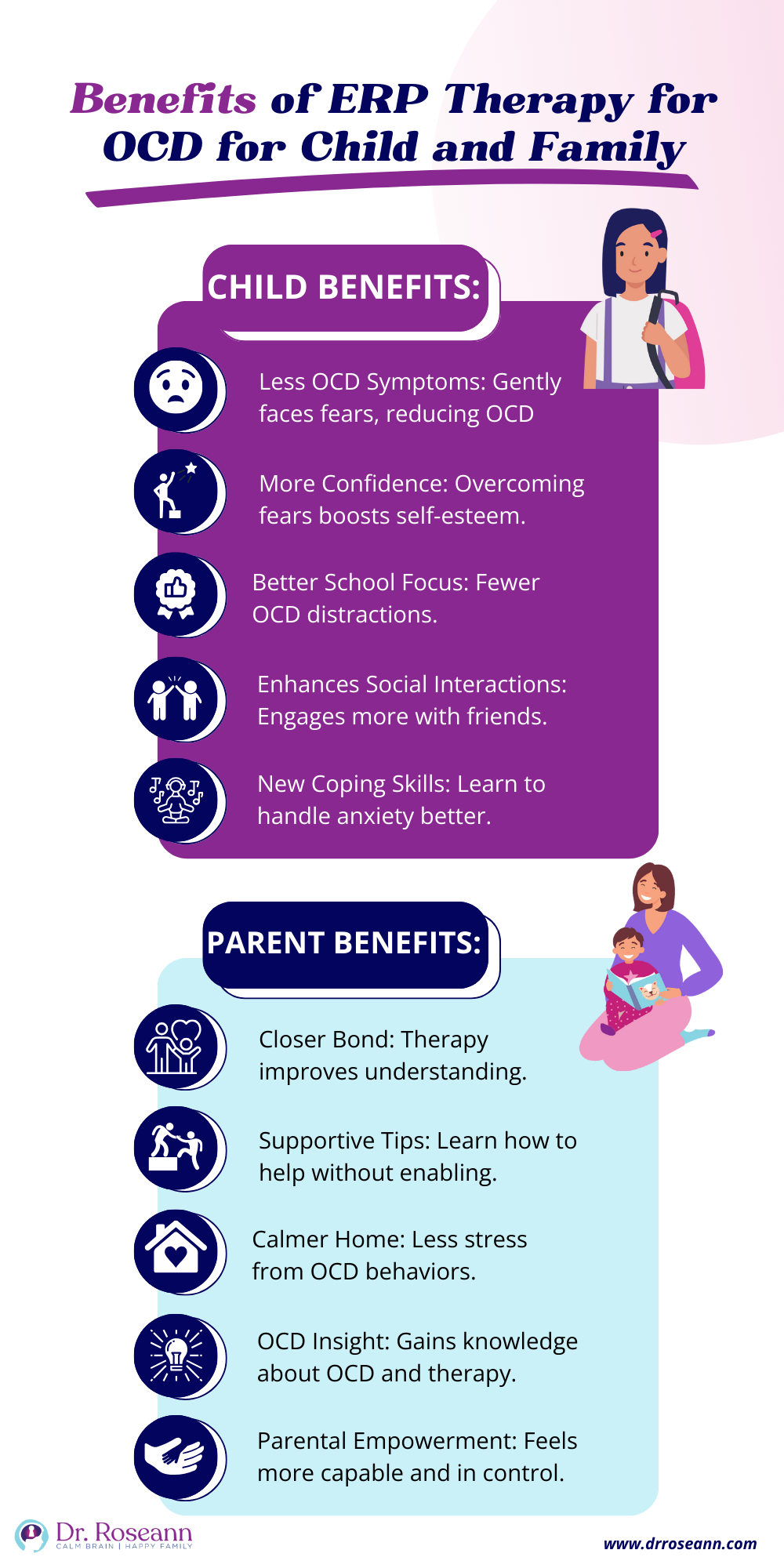
It is essential to discuss what family members should expect from treatment and paint the picture of the work done in Exposure and Response Prevention (ERP) Therapy. The daily life of living with a person with obsessive thoughts and repeated behaviors, especially repeated questioning that can go on for hours a day, can be very draining, and parents need to know what to say and do to help their child break the cycle.
How to Address Treatment-Resistant OCD

Treatment resistant OCD can be challenging to address, but several strategies can be considered. First, take a step back and understand what's happening. A thorough assessment is the key to giving us a good lay of the land to chart an effective treatment course.
A randomized controlled trial looked at treating OCD in young people who haven't responded well to previous treatments. They found that when these kids received specialized therapy, like CBT, with or without medication changes, their symptoms got a lot better. But they also discovered that many kids hadn't been getting the right kind of therapy before, which made their OCD worse. The study suggests that giving the proper treatment can help kids with OCD feel better (Krebs et al., 2014).
I once worked with a remarkable young girl named Emily, who had been battling OCD for years. Despite trying different medications and therapies, she felt like she was hitting a wall. But you know what? We didn't give up. We looked closely at her treatment plan, considered all the puzzle pieces, and decided to try something new.
We started incorporating exposure and response prevention (ERP) therapy into her sessions. ERP might sound intimidating, but consider it taking small steps outside your comfort zone, one at a time. Giving parents the tools to not accommodate the OCD is critical is overcoming OCD.
For Emily, it meant gradually facing her fears, whether it was touching a “contaminated” object or resisting the urge to perform her rituals. Over time, those small victories added up. She began to reclaim control over her life, one brave step at a time.
What Questions You Should Discuss With Your OCD Therapist?
Psychoeducation about how OCD affects the brain and behavior is critical for the child and parent. Obsessions and compulsions are hard to understand and of course are often internal, so understanding about how they form a habit in the brain is critical for conquering intrusive thoughts.
- What is Obsessive Compulsive Disorder?
- What are the symptoms of OCD in children and adolescents?
- What are the specific types of OCD symptoms that are present and how they affect your life?
- What are intrusive thoughts, obsessions, and compulsions?
- When did OCD symptoms begin?
- What are the OCD triggers?
- Will OCD in a child go away, and will my child outgrow OCD?
- Why do I need to treat OCD in my child and how it affects their brain?
- In what ways can we understand and respond to OCD symptoms without accommodating it?
- How do you help a child with OCD at home or school?
- How do you help with OCD bedtime rituals?
- How do you stop OCD intrusive thoughts?
- What is the best treatment for OCD in kids and teens?
- Can neurofeedback help OCD?
- What herbs help OCD?
- What does OCD treatment look like in children and teens?
- Do medications help OCD in children and teens?
- How does ERP work for kids?
- How do you start ERP for OCD and how long is ERP for OCD therapy for children and teens?
- What’s the difference between ERP and CBT for ERP?
- Why does talk therapy not help or worsen OCD?
- Does ERP for OCD help for PANS/PANDAS?
- What is the best treatment for PANS/PANDAS OCD?
- What are helpful parent resources for OCD in children and teens?
What is OCD Therapy Like?
A mental health professional who uses Cognitive Behavioral Therapy and Exposure Response and Prevention Therapy (ERP) for OCD will spend time at every session helping a child or teen and their parents understand why OCD thoughts and compulsions form a neurological habit and exactly how to use neuroscience to “talk back” to OCD.
Once they know the negative reinforcement cycle, kids with Obsessive Compulsive Disorder have the power to break OCD habituation. They learn to take control of their OCD instead of OCD being in control.
Developing OCD typically doesn't happen overnight, although it can with sudden onset due to PANS/PANDAS/AE, so most of the time, it will take many weeks and months to get intrusive thoughts and compulsive behaviors to a more manageable level or to even within a normal range.
What is the Best Treatment for OCD in Children and Teens?
We use a combination of two science-backed approaches, such as response prevention therapy and neurofeedback, with our in-person and virtual clients. In terms of the most effective type of psychotherapy, the efficacy of ERP for OCD is well documented. It is designed to give clients the education and skills to control their thoughts and sensations that have hijacked their brains.
Unlike talk therapy, which over-focuses on feelings, ERP teaches one to reign in those runaway thoughts. I can’t tell you how many kids (and adults) with severe OCD have found the most value in ERP in helping them break free from intrusive thinking and not connect to feelings first.
One pediatric OCD treatment study looked at how different treatments help kids with OCD. They studied 112 kids who either took medicine, talked to a therapist, did both, or took a fake pill. They found that kids who had milder obsessive compulsive symptoms understood their problem better, had fewer behavior issues, and got less help from their families improved the most with any treatment.
But if a kid had a family member with OCD, talking to a therapist alone didn't help as much. This means kids might need a mix of therapy and other treatments if someone in their family has OCD. This pediatric OCD study shows that each kid with OCD requires different kinds of help, and it's essential to consider their family history when deciding on treatment (Garcia et al., 2010).
ERP for Obsessive Compulsive Disorder in Children and Adolescents
Exposure and response prevention (ERP) is a type of cognitive therapy that’s considered the gold standard of treatment for children and adolescents with OCD. Its systematic methods have a lot of research to show how effective ERP is in reducing and even eliminating a child’s symptoms.
ERP requires heavy parental involvement and practice at home, helping your child break the OCD cycle. That means teaching your child how to cope with anxiety disorder, intrusive thoughts, and compulsions instead of accidentally reinforcing them by what we say and do.
And when you combine calming the nervous system with OCD therapy such as ERP, children with OCD can get better. We don’t talk enough about OCD success stories but at my Ridgefield, CT clinic, we help kids, adults and families tackle OCD every day.
We walk parents through this and teach them how to respond to OCD-driven behaviors and what to say to their children. Parents are often unsure of what to say to their child with OCD, and it’s so hard to see a child in distress, and gaining these tools is a game changer. A good ERP therapist empowers the child and family members with OCD tools to tamp down that OCD tyrant!
Neurofeedback for OCD in Children and Adolescents
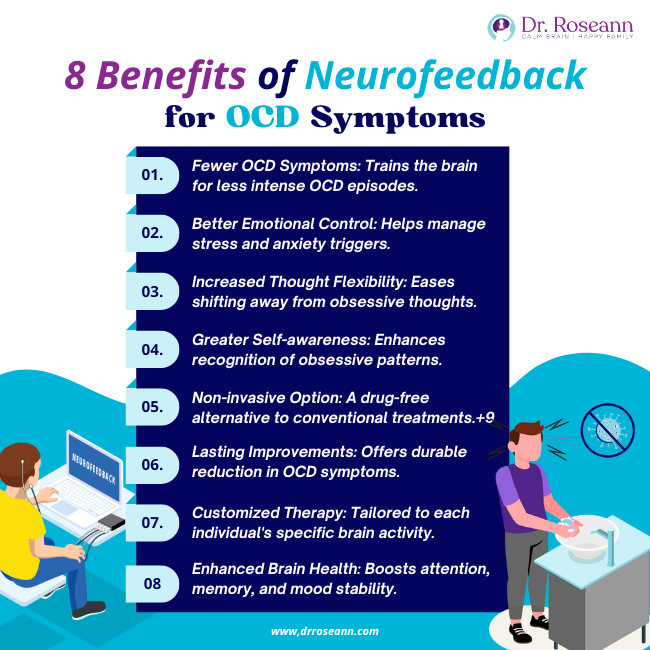
If one’s nervous system is stress-activated, then a child with severe OCD can’t think, pay attention, or take action in a way that stops their OCD. Instead, their stress-hijacked brain gets stuck in a looping thought and behavioral pattern. That is why neurofeedback for OCD is so powerful because it calms the CNS at a subconscious level so a person isn’t in a constantly activated state.
Neurofeedback calms the nervous system and moves a child to a more relaxed, parasympathetic state, and when that happens, the person with OCD can have the bandwidth to take action and think differently.
We use brain-based therapies to calm the nervous system so that a person can respond to all stimuli more healthily. That means fewer obsessions, compulsions, irritated and angry behaviors, worried thoughts, calm thinking, engaged behaviors, and an ability to think and act without getting stuck.
Aside from neurofeedback, there are great natural treatments for OCD, such as supplements, herbs, and ERP. If you are looking for information on natural solutions and treatments for OCD, then download The Natural OCD Thought Tamer Kit.
Does Medication Help Obsessive Compulsive Disorder?
Given the potential of medication side effects and the toxic effect of psychiatric medications like Selective Serotonin Reuptake Inhibitors (SSRI) on a developing brain, it is preferable to begin treatment with ERP and neurofeedback. This combination is not only practical but also safe and natural. Treatments such as neurofeedback for OCD, supplements for OCD, and ERP for OCD are science-backed methods that create lasting change.
How do anxiety disorders relate to OCD?
Anxiety disorders and OCD are related in that they both involve excessive anxiety; however, OCD is characterized by specific obsessive thoughts and compulsive behaviors, whereas anxiety disorders encompass a broader range of conditions with varied triggers and symptoms. While both conditions involve anxiety, OCD is distinguished by the presence of obsessions and compulsions.
How do you address children with mental disorders like OCD?
Children with mental disorders like OCD are typically treated using a combination of therapies, including cognitive-behavioral therapy (CBT) tailored for children, natural treatments, and family involvement. CBT helps children learn to manage their symptoms by gradually facing their fears and reducing compulsive behaviors. Family support and understanding are crucial in providing a nurturing environment that supports the child’s intensive treatment programs.
Why isn't my current treatment working for my OCD?
It's not uncommon for OCD treatment to require some trial and error. Sometimes, the approach we've been using needs adjustments to suit your child’s unique needs. That's where our collaboration comes in—we'll explore new avenues until we find what works for you and your child.
I've tried therapy and medications before—what else can I do?
It's understandable to feel frustrated, but there are still plenty of options to explore. Consider combining different therapies, trying alternative medications, or incorporating lifestyle changes into your routine. Together, we'll brainstorm creative solutions tailored to your situation.
Can't I just tough it out and ignore my OCD symptoms?
While it's tempting to try to push through, ignoring OCD symptoms often leads to increased distress and can reinforce the cycle of obsessions and compulsions. Instead, we'll gently challenge those thoughts and behaviors through therapy, empowering you to regain control over your life.
Is it normal to feel overwhelmed or discouraged during treatment?
Absolutely. Facing the challenges of OCD treatment can feel daunting at times, but it's important to remember that progress isn't always linear. We're here to support you through the ups and downs, offering encouragement and guidance every step of the way.
How long will it take to see improvement in my OCD symptoms?
Patience is vital. Recovery from OCD is a gradual process, and the timeline can vary from person to person. While some children may experience improvements relatively quickly, it may take more time and persistence for others. Rest assured, we'll work together to develop a treatment plan that sets you toward lasting change.
Citations
Garcia, A. M., Sapyta, J. J., Moore, P. S., Freeman, J. B., Franklin, M. E., March, J. S., & Foa, E. B. (2010). Predictors and Moderators of Treatment Outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 1024–1033. https://doi.org/10.1016/j.jaac.2010.06.013
Krebs, G., Isomura, K., Lang, K., Jassi, A., Heyman, I., Diamond, H., Advani, J., Turner, C., & Mataix-Cols, D. (2014). How resistant is “treatment-resistant” obsessive-compulsive disorder in youth? British Journal of Clinical Psychology, 54(1), 63–75. https://doi.org/10.1111/bjc.12061
Dr. Roseann is a mental health expert in OCD who is frequently in the media:
- BCIA: Calming the OCD Brain with Neurofeedback and ERP Therapy
- Hope for Anxiety and OCD: Sudden Onset OCD
- Integrative Practitioner: Integrative Approaches to Treating OCD
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Break the chain of OCD without medication. Download your copy of
The Natural OCD Thought Tamer Kit
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024