Obsessive-Compulsive Disorder (OCD) is a complex mental health condition that significantly affects the brain's function and chemistry. For parents of children and teens with OCD, understanding the biology of this disorder is crucial.
It's not just a series of habits or quirks; OCD is a neurological disorder that impacts neurotransmitter activity and brain structure, leading to a cycle of negative reinforcement. This blog aims to shed light on the biology of OCD and highlight natural, science-backed solutions for managing this condition.
Understanding the Biology of OCD
Obsessive-Compulsive Disorder (OCD) is indeed more than a collection of habits or quirks; it's a complex neurological disorder that significantly impacts brain function and chemistry. To fully grasp its effects, it's essential to delve into how OCD influences the brain, neurotransmitter activity, and perpetuates a cycle of negative reinforcement.
Neurotransmitter Imbalance and Brain Structure
At the core of OCD are imbalances in neurotransmitters, which are chemicals that transmit messages between neurons in the brain. The most notable of these is serotonin, a neurotransmitter that plays a critical role in regulating mood, anxiety, and happiness. In individuals with OCD, there's often an irregularity in serotonin levels, leading to the disruption of normal thought processes and behaviors.
Furthermore, OCD involves changes in certain areas of the brain. For instance, studies have shown that people with OCD often have increased activity in the orbitofrontal cortex, the part of the brain responsible for decision making and judgment. There's also altered functioning in the anterior cingulate cortex, which is involved in error detection, and in the basal ganglia, which helps control body movements. These structural and functional changes in the brain manifest in the form of persistent, intrusive thoughts and repetitive behaviors that are characteristic of OCD.
The Cycle of Negative Reinforcement
One of the key aspects of Obsessive Compulsive Disorder is how it creates a cycle of negative reinforcement. This cycle begins with an intrusive, often irrational thought or fear (obsession). For instance, a person might have an overwhelming fear of germs or contamination. This obsession then leads to a corresponding compulsion – a repetitive behavior or mental act that the person feels driven to perform to alleviate the distress caused by the obsession, like excessive hand washing.
The temporary relief provided by these compulsions reinforces the behavior, even though it is irrational. This relief is key; it's a negative reinforcement because it removes the distressing feeling, thereby increasing the likelihood of the compulsive behavior recurring in the future. Over time, this cycle becomes more entrenched, and the compulsions become more time-consuming and disruptive, often significantly impacting the person's daily life.
The Impact on Brain Development in Children and Teens
In children and teens, whose brains are still developing, Obsessive Compulsive Disorder can have a particularly profound impact. The repetitive nature of OCD behaviors can interfere with normal brain development, especially in areas related to decision-making, habit formation, and emotional regulation. This can lead to challenges in social interactions, academic performance, and overall emotional well-being.
For parents, understanding the biological underpinnings of OCD is crucial. It helps in recognizing that OCD is not a choice or a phase, but a serious mental health condition that requires professional intervention. This knowledge is empowering, as it guides parents towards seeking appropriate and effective treatments such as cognitive behavioral therapy and ERP, which can help break the cycle of negative reinforcement and manage the symptoms of OCD.
The biology of OCD is complex, involving neurotransmitter imbalances, structural and functional brain changes, and a self-perpetuating cycle of negative reinforcement.
Genetic and Environmental Factors That Affect the OCD Brain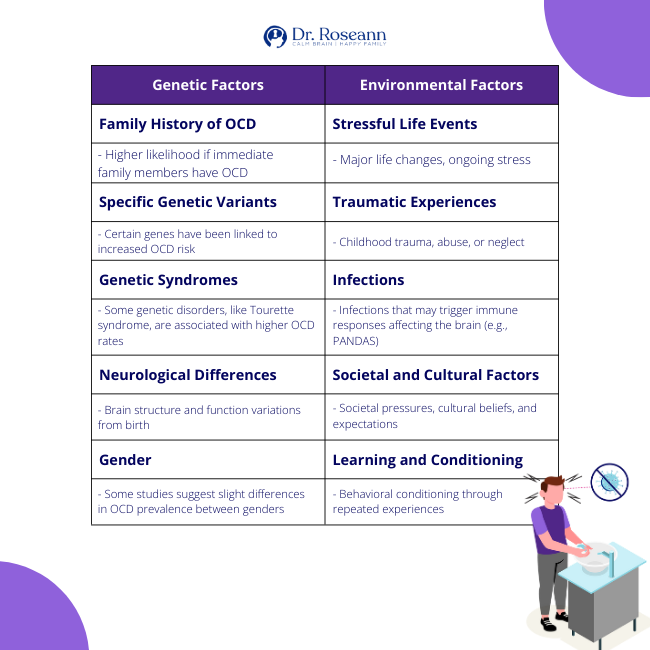
Genetics and OCD: Unraveling the Hereditary Puzzle
Obsessive-Compulsive Disorder (OCD) is a complex condition where genetics play a significant role. While the exact cause of OCD is still not entirely understood, research has consistently pointed towards a notable genetic component in its development. This understanding is crucial for families grappling with OCD, as it can guide early recognition and intervention.
The Role of Genetics in OCD
Studies have indicated that genetics are a significant factor in the likelihood of developing OCD. Individuals with first-degree relatives (parents, siblings, or children) who have OCD are at a higher risk of developing the disorder themselves. This familial pattern suggests that genes, alongside environmental factors, contribute to the risk of OCD.
Identifying Genetic Markers
Researchers have identified specific genetic markers that are more common in individuals with OCD. For instance, variations in genes related to the brain's serotonin system, which is integral to mood regulation and anxiety, have been linked to OCD. Serotonin is a neurotransmitter that helps relay messages in the brain, and irregularities in its function can lead to the characteristic symptoms of OCD.
Brain Structure and Genetic Influence
Genetics not only influence the chemical makeup of the brain but also its structure. Studies using brain imaging techniques like MRI (Magnetic Resonance Imaging) have shown differences in certain brain areas in people with OCD. For example, variations in the size and activity of the orbitofrontal cortex and anterior cingulate cortex are often observed. These brain regions are crucial for decision-making, behavior regulation, and error detection, which are areas typically affected in OCD.
Genetic Variants and OCD
Common genetic variants such as MTHFR that affect how the body removes toxins from the body and how we use the B vitamins, are associated with Obsessive Compulsive Disorder. Identifying how genetic variants impact your nutrient absorption can be pivotal in addressing root causes.
The Impact of Early Recognition
Understanding the genetic links to OCD can be a game-changer for early diagnosis and intervention. If OCD is known to run in a family, parents can be more vigilant about recognizing early symptoms in their children.
Early recognition can lead to prompt intervention, which is critical in managing OCD effectively. Interventions might include therapy, lifestyle changes, and in some cases, medication, all of which can be more effective when started early.
Genetic Research: A Pathway to Personalized Treatment
Ongoing research into the genetics of OCD is opening doors to more personalized treatment approaches. By understanding the specific genetic factors at play in an individual's OCD, treatments can potentially be tailored more effectively to their unique genetic makeup.
There already are personalized approaches to nutrition and supplements based on genetic variants. This personalized approach could improve treatment outcomes and provide more targeted strategies for managing the disorder.
Environmental Factors and OCD
The development of OCD is not solely based on genetics; environmental factors also play a significant role. Stressful life events, trauma, and even certain infections can trigger or exacerbate OCD symptoms. Recognizing these environmental triggers is essential in managing OCD, as it allows for targeted interventions that address these specific stressors.
Here are key environmental influences that can play a role in the development or exacerbation of OCD:
Stressful Life Events:
- Major life changes such as moving, loss of a loved one, or divorce.
- Chronic stress, either from daily life pressures or ongoing challenging situations.
Traumatic Experiences:
- Childhood trauma including physical, emotional, or sexual abuse.
- Significant traumatic events later in life, like accidents or natural disasters.
Infections and Immune System Responses:
- Certain infections, such as streptococcal infections, can trigger OCD symptoms, particularly in children (as seen in PANDAS – Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections and PANS).
- Autoimmune reactions where the body’s immune response affects brain function.
Parenting Styles and Family Dynamics:
- Overly strict or protective parenting potentially increasing anxiety and control behaviors.
- Family conflicts or a high-stress home environment.
- Over accommodation of the behaviors can accidently “feed” the OCD.
Cultural and Societal Influences:
- Societal pressures or norms that emphasize perfectionism or high achievement.
- Cultural stigma surrounding mental health that can exacerbate stress and anxiety.
Learning and Conditioning:
- Behaviors learned or conditioned through repeated exposure to certain situations or responses.
- Modeling behaviors after a family member or significant person with OCD or similar symptoms.
Substance Use and Abuse:
- Alcohol or drug use that can alter brain chemistry and potentially trigger or worsen OCD symptoms.
- Dependence on substances as a coping mechanism for anxiety or stress, indirectly influencing OCD behaviors.
Environmental Toxins and Health:
- Exposure to certain chemicals or pollutants that may impact brain health.
- Poor overall physical health or chronic conditions that stress the body and mind.
- Problems with detoxification can impact health.
These environmental factors, combined with genetic predispositions, contribute to the complexity of OCD. Recognizing and addressing these factors can be an essential part of a comprehensive treatment strategy for managing OCD in children and teens.
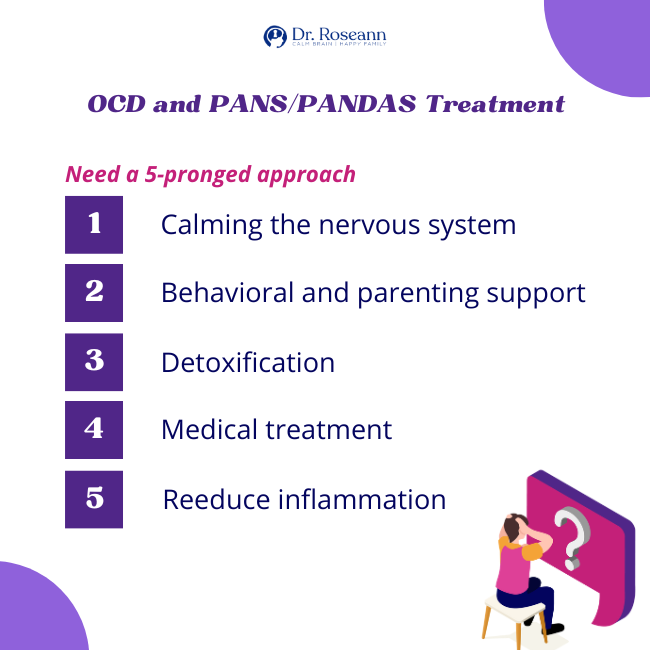
Brain Inflammation and the OCD Brain: PANS/PANDAS
A notable example of the interaction between environmental factors and OCD is seen in conditions like Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) and Pediatric Acute-onset Neuropsychiatric Syndrome (PANS).
These conditions involve brain inflammation triggered by an immune response, leading to sudden and severe OCD symptoms. Understanding these conditions underscores the importance of considering physical health and immune responses in managing OCD.
Anxiety and Other Clinical Issues and Their Link to OCD
Anxiety and OCD are different and thus should be treated differently. However, anxiety often coexists with OCD, and it's crucial to understand their relationship. Anxiety reflects real life worries. OCD on the other hand is about irrational fears that lead to compulsive behaviors.
Coexisting conditions like autism, depression or other anxiety disorders can also complicate OCD, making getting to the root causes and addressing OCD from a multi-pronged approach necessary. .
What Does an OCD Brain Look Like?
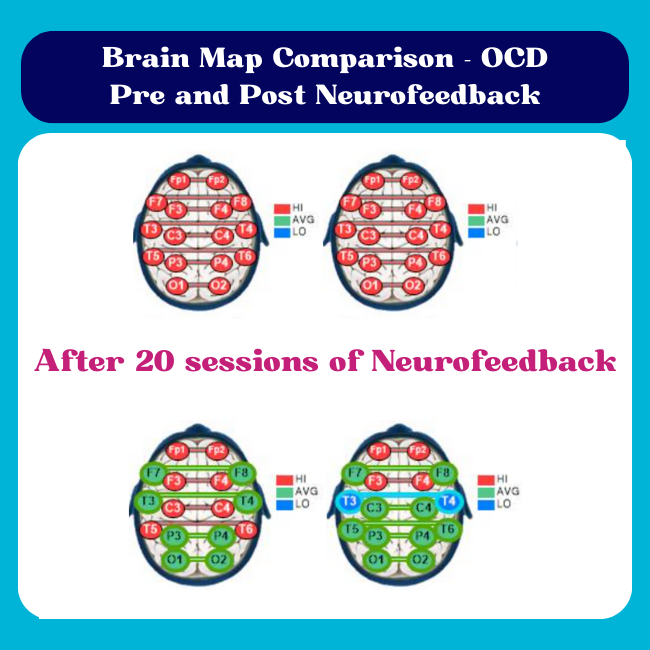
Advances in QEEG brain maps and brain imaging, such as magnetic resonance imaging (MRI), have provided insights into how OCD affects the brain. People with OCD show differences in brain regions like the orbitofrontal cortex, responsible for decision-making, and the anterior cingulate cortex (ACC), involved in error detection.
QEEG brain maps show distinct OCD brain patterns including hyper brain communication that is often seen in individuals that have looping or intrusive thoughts. With neurofeedback in our BrainBehaviorReset™ Program, we are able to calm this brain communication so the child, teen or adult can tolerate exposure without getting so activated.
How to Calm The OCD Brain
Calming the OCD brain involves a combination of therapies such as neurofeedback, PEMF, diet and supplements such as magnesium. Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention (ERP) are effective in breaking the cycle of negative reinforcement.
Alongside these, natural methods like essential oils, mindfulness, relaxation techniques, and regular physical exercise can help soothe the brain and manage symptoms.
For parents, understanding the biological underpinnings of OCD is empowering. It offers a roadmap for seeking appropriate treatments and supporting their children through the challenges of OCD. The biology of OCD involves neurotransmitter imbalances, brain structural changes, and a self-perpetuating cycle of negative reinforcement. By grasping these concepts, parents can guide their children toward effective management and recovery.
Final Words on The Brain and OCD
The journey through OCD is not easy and boy it can affect the parent-child relationship, but with a solid understanding of its biological basis, parents can be well-equipped to help their children navigate this challenging condition. Embracing both science-backed treatments and natural solutions offers a balanced approach to managing OCD, paving the way for a healthier, more fulfilling life for those affected.
Citations:
Biria, M., Banca, P., Healy, M.P. et al. Cortical glutamate and GABA are related to compulsive behaviour in individuals with obsessive compulsive disorder and healthy controls. Nat Commun 14, 3324 (2023). https://doi.org/10.1038/s41467-023-38695-z
Endres, D., Pollak, T. A., Bechter, K., Denzel, D., Pitsch, K., Nickel, K., Runge, K., Pankratz, B., Klatzmann, D., Tamouza, R., Mallet, L., Leboyer, M., Prüss, H., Voderholzer, U., Cunningham, J. L., ECNP Network Immuno-NeuroPsychiatry, Domschke, K., Tebartz van Elst, L., & Schiele, M. A. (2022). Immunological causes of obsessive-compulsive disorder: is it time for the concept of an “autoimmune OCD” subtype?. Translational psychiatry, 12(1), 5. https://doi.org/10.1038/s41398-021-01700-4
Huey, E. D., Zahn, R., Krueger, F., Moll, J., Kapogiannis, D., Wassermann, E. M., & Grafman, J. (2008). A psychological and neuroanatomical model of obsessive-compulsive disorder. The Journal of neuropsychiatry and clinical neurosciences, 20(4), 390–408. https://doi.org/10.1176/jnp.2008.20.4.390
Mahjani, B., Bey, K., Boberg, J., & Burton, C. (2021). Genetics of obsessive-compulsive disorder. Psychological medicine, 51(13), 2247–2259. https://doi.org/10.1017/S0033291721001744
Sowden, E., Robinson, D., Lovell, K., Bee, P., Fulwood, A., Lidbetter, N., Wilson, Z., Brown, A., & Pedley, R. (2023). Understanding the support needs of parents of children with obsessive-compulsive disorder: a qualitative descriptive study in the UK. BMC psychiatry, 23(1), 309. https://doi.org/10.1186/s12888-023-04637-8
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023