Relationships are complex webs of emotions, communication, and understanding. It's important to remember that when it comes to individuals with Pathological Demand Avoidance (PDA), these dynamics can become even more complicated.
Pathological Demand Avoidance, also known as Extreme Demand Avoidance is a subtype of Autism Spectrum Disorder (ASD) that manifests in an intense resistance to the ordinary demands of life. It means that autistic children or those with this pervasive developmental disorder are likely to show this condition.
This condition was first studied by Professor Elizabeth Newson, showing that individuals with the PDA profile often exhibit high levels of controlling behaviors, difficulty with social relationships, and a strong desire for sameness.
It is crucial to recognize that PDA is a neurodevelopmental condition, and the challenging behaviors associated with it are not intentional but rather a response to high levels of anxiety (Johnson & Saunderson, 2023). Developing meaningful connections with autistic people who also have PDA requires patience, empathy, and a willingness to adapt.
Understanding PDA and the Challenges in Relationships
Individuals with the Pathological Demand Avoidance Syndrome often face significant challenges in forming and maintaining relationships. These challenges arise from the core characteristics of the condition, wherein people with PDA feel the need to avoid demands.
Here's a detailed explanation of the challenges faced by young people with or without autism diagnosis suffering from the need to practice the extreme avoidance of everyday demands of all kinds.
Common Challenges of Those with PDA
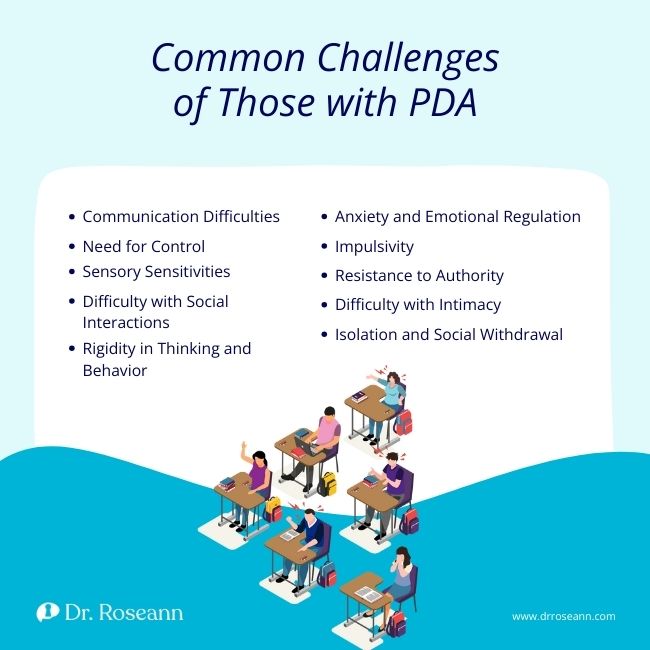
Communication Difficulties
The subset of people with PDA traits may experience challenges in verbal and non-verbal communication. They may struggle with interpreting social cues, facial expressions, and body language. Expressing their own emotions and needs can also be difficult, which causes frustration and misunderstandings in relationships.
Need for Control
One of the defining features of PDA is an overwhelming need for control. In relationships, this need for control can manifest as a resistance to external demands and expectations. The individual may go to great lengths to avoid situations where they feel their control is being challenged as they have a high intolerance of uncertainty. They often revert to the use of social strategies, leading to power struggles within the relationship.
Sensory Sensitivities
Many individuals with PDA have heightened sensory sensitivities. Common stimuli such as loud noises, bright lights, or certain textures can be overwhelming and cause distress. Navigating these sensitivities within a relationship may require careful consideration of the environment and activities to avoid triggering discomfort.
Difficulty with Social Interactions
Individuals with PDA often struggle with social interactions, finding it challenging to understand and navigate the complexities of social relationships. They may have difficulty establishing and maintaining friendships, interpreting social cues, and engaging in reciprocal communication.
Rigidity in Thinking and Behavior
Rigidity in thinking is a characteristic of PDA. Individuals may have a narrow focus on specific topics or routines, making it challenging to adapt to changes or compromises within a relationship. This inflexibility can limit the variety of experiences shared in the relationship. Healthcare professionals play a crucial role in providing them with appropriate support regarding this matter.
Anxiety and Emotional Regulation
High anxiety levels are a pervasive challenge and a core feature of PDA. The fear of demands and the need for control can contribute to heightened stress levels. Difficulties in regulating emotions may result in social anxiety, meltdowns, mood swings, panic attacks, or shutdowns, impacting the emotional dynamics of the relationship.
Impulsivity
Some individuals with PDA may exhibit impulsive behavior, acting without considering the consequences. This impulsivity can affect one's decision-making processes in relationships and may lead to challenges in maintaining a stable and predictable environment.
Resistance to Authority
Individuals with PDA often resist authority figures, including those within the context of personal relationships. This resistance can manifest as defiance or opposition to suggestions or requests, contributing to communication breakdowns.
PDA is not to be confused with Oppositional Defiant Disorder (ODD) as ODD involves persistent defiance toward authority, while PDA, manifests as extreme avoidance of demands driven by anxiety and a need for control.
Difficulty with Intimacy
Establishing and maintaining intimacy can be challenging for individuals with PDA. The need for control and the difficulties in understanding social nuances may impede the development of emotional and physical intimacy in romantic relationships.
Isolation and Social Withdrawal
Due to the challenges associated with social interactions and demands, individuals with PDA may withdraw from social situations, leading to isolation. This withdrawal can limit the opportunities for building and sustaining relationships.
Strategies for Building Positive Relationships
Building positive relationships with children and teens with PDA requires a thoughtful and flexible approach. However, calling someone's behavior PDA without a proper diagnosis can create confusion (Green et al., 2018). Here are strategies to help navigate and foster positive connections:
- Be flexible in your expectations and adapt to the individual's needs. Recognize that routines and plans may need to be adjusted to accommodate their comfort level and minimize anxiety.
- Use clear and explicit language to convey expectations and requests. Avoid vague or ambiguous instructions, as clarity can reduce anxiety and enhance understanding.
- Create and maintain predictable routines, as children with PDA often find comfort in consistency. Communicate any changes in advance, allowing them to prepare for deviations from the routine.
- Offer choices whenever possible to provide a sense of control. Allowing individuals with PDA to make decisions empowers them and reduces the likelihood of resistance.
- Acknowledge the need for personal space and boundaries. Respect their autonomy and avoid pressuring them into situations that may trigger anxiety.
- Discover and engage in activities that align with the individual's interests. Shared interests can serve as a foundation for positive interactions and strengthen the bond between you.
- Utilize visual aids, schedules, and charts to help kids with PDA understand expectations and routines. Visual supports can provide a concrete and visual representation of information and aid in comprehension.
- Help individuals develop and practice strategies for emotional regulation. This may include mindfulness techniques, sensory tools, or designated spaces where they can retreat and self-regulate when needed.
- Implement a system of positive reinforcement to acknowledge and reward desirable behaviors. Reinforce positive actions and accomplishments to motivate, solicit a positive response, and build confidence.
- Educate yourself and others about PDA to foster understanding and empathy. Share information with friends, the whole family, and colleagues to create a supportive network and reduce misconceptions about the key features of PDA.
- Involve your child in collaborative problem-solving in their everyday tasks. Engage in open communication to address challenges and find solutions together, fostering a sense of cooperation and shared responsibility.
- Be mindful of the sensory environment. Create spaces that are calm and comfortable, considering lighting, noise levels, and textures to minimize sensory overload.
- Support the development of social skills through role play, structured activities, and social stories. Guide them in interpreting social cues and navigating social interactions.
- Engage with professionals who specialize in autism spectrum disorders or PDA. Therapists, counselors, and support groups can offer not just professional help but also valuable insights and strategies for children and parents through their access to and expertise in the Diagnostic and Statistical Manual of Mental Disorders.
- Reach out to the Natural Autistic Society or any local PDA society to assist you in helping your child navigate through their condition. Getting support from fellow parents would make things a lot easier.
Navigating relationships with children and teens with Pathological Demand Avoidance requires patience, understanding, and a commitment to improving communication skills and adapting the right expectations.
Recognizing the unique needs and challenges associated with PDA allows us to create a supportive environment that fosters positive connections. It's essential to approach these developmental disorders with empathy, openness, and a willingness to learn and grow together.
Help your child with PDA using the BrainBehaviorResetTM Program. This program has the best interest of children and young adults as it uses natural science-backed solutions to address neurodevelopmental conditions like autism and PDA.
It incorporates neurofeedback, PEMF, and magnesium supplements to help your child go through the challenges in their daily life. The program may also include therapy sessions that aim to teach children the right coping mechanism to combat the symptoms and signs of PDA such as anxiety disorder, executive dysfunction, and demand avoidance behaviors
Parent Action Steps
☐ Learn more about emotional regulation by listening to my podcast, It’s Gonna Be OK!
☐ Stay informed about PDA to understand your child's challenges and strengths.
☐ Embrace adaptability in your parenting style to accommodate your child's need for control.
☐ Involve your child in finding solutions to challenges to foster autonomy, especially related to academics.
☐ Model and reinforce positive social interactions.
☐ Use the Solutions Matcher to get a personalized treatment plan for your kids.
Citations
Green, J., Absoud, M., Grahame, V., Malik, O., Simonoff, E., Le Couteur, A., & Baird, G. (2018). Pathological Demand Avoidance: symptoms but not a syndrome. The Lancet Child & Adolescent Health, 2(6), 455–464. https://doi.org/10.1016/s2352-4642(18)30044-0
Johnson, M., & Saunderson, H. (2023). Examining the relationship between anxiety and pathological demand avoidance in adults: a mixed methods approach. Frontiers in Education, 8. https://doi.org/10.3389/feduc.2023.1179015
Dr. Roseann is a mental health expert who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind New Research Highlights Key Differences Among Autistic Boys and Girls
- She Knows 11 Products Moms of Kids With ADHD Swear By to Maintain Order in the Chaos
- Very Well Mind What Is Asperger Syndrome?
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024