Imagine a child who avoids brushing their teeth like it's the plague, throws panic attacks at the mere mention of homework, and seems to possess an uncanny ability to wriggle out of everyday demands from whom they regard as authority figures.
But this isn't just plain stubbornness. It could be a sign of a condition called Pathological Demand Avoidance (PDA), a unique profile within the Autism Spectrum Disorder (ASD) umbrella.
Though without a formal diagnosis, PDA may be closely likened to Oppositional Defiant Disorder (ODD),which is characterized by persistent defiance without a strong anxiety component. However, PDA involves extreme resistance to demands driven by high levels of anxiety and a pronounced need for a strong sense of control.
What is the Pathological Demand Avoidance Profile?
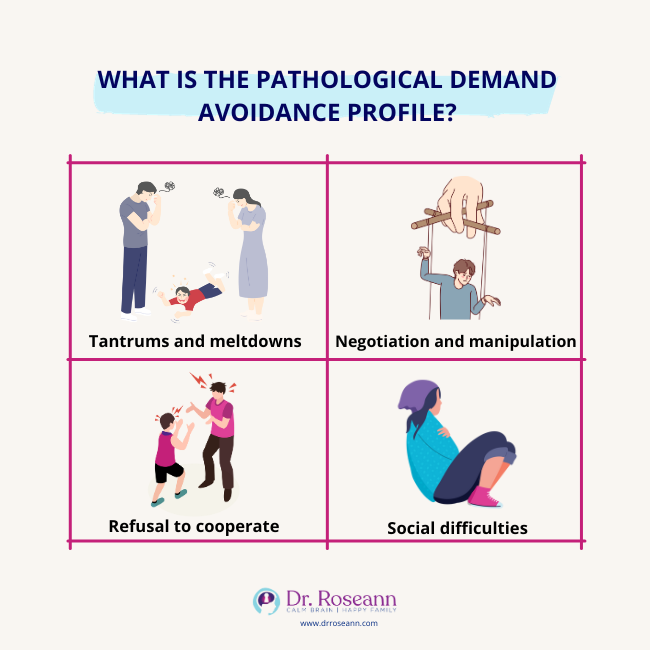
Coined by British psychologist Elizabeth Newson in the 1980s, PDA is characterized by an intense, pervasive drive for autonomy. People with PDA experience overwhelming anxiety and distress when faced with demands as they perceive them as a threat to their control. This can manifest in resisting and avoiding the ordinary demands of life and lead to:
- Tantrums and meltdowns: Seemingly trivial requests like putting on shoes or tidying a room can trigger an intense emotional outburst or panic attack.
- Negotiation and manipulation: Young people with PDA might bargain, charm, or even resort to tantrums to avoid unwanted tasks. They tend to employ social strategies to wiggle out of the ordeal.
- Refusal to cooperate: Following instructions, completing routines, and participating in everyday activities can become major battles. The use of social strategies to avoid demands is common.
- Social difficulties: Social interaction, with its inherent expectations and demands, can be challenging for people with PDA.
Pathological Demand Avoidance (PDA) vs Autism Spectrum Disorder (ASD)
While both PDA and ASD fall under the umbrella of pervasive developmental disorder, ASD, is a broader term covering a spectrum of presentations. PDA represents a newly emerging profile emphasizing extreme demand avoidance and control issues within that spectrum. Here are some of the key differences between PDA and ASD:
- Focus on demand avoidance: Unlike the core social and communication challenges in autistic people, the defining feature of PDA is the resistance to demands to an extreme extent.
- Surface sociability: Some PDA individuals exhibit good social skills in specific situations, known as “surface sociability.” This can mask the underlying anxiety and make diagnosis more complex.
- Mood swings and impulsivity: Emotional volatility and impulsive behavior are more common in PDA compared to typical presentations in autistic children.
How Does One Get the PDA Profile?
PDA is not a recognized diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). However, the National Autistic Society and the PDA Society offer valuable resources and diagnostic tools like the Extreme Demand Avoidance Questionnaire (EDA-Q) to help professionals identify this profile.
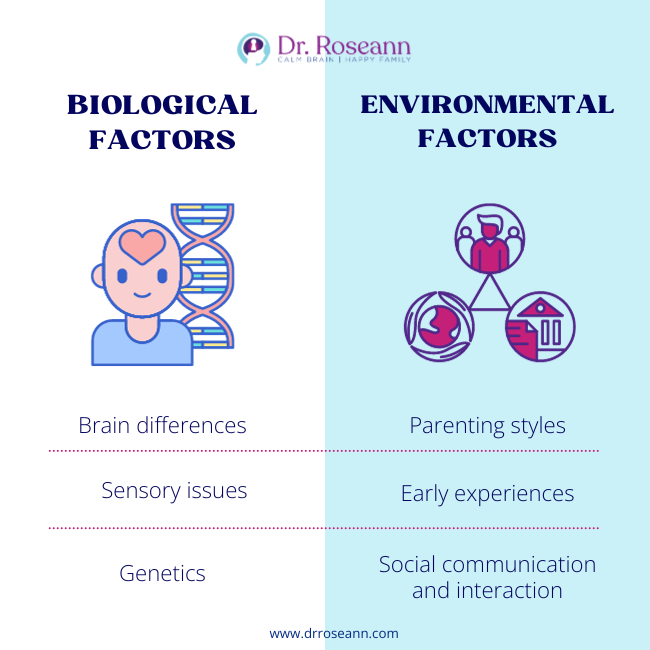
The exact cause of PDA remains unknown, but PDA research points out that it stems from a complex interplay of biological and environmental factors (Christie, 2012). Here's what we currently understand:
Biological Factors
- Brain differences: Studies suggest some individuals with PDA may have subtle differences in brain regions responsible for decision-making, emotional regulation, and executive functioning. These differences could contribute to heightened sensitivity to direct demands and difficulty processing them.
- Sensory issues: Overlapping sensitivities to sensory stimuli like noise, touch, or sight are sometimes seen in individuals with PDA. Such sensory overload can intensify their perception of demands as overwhelming or even painful.
- Genetics: While there's no single “PDA gene,” research suggests a genetic component likely plays a role, making some individuals more susceptible to developing the profile (Good, 2016).
Environmental Factors
- Parenting styles: Authoritarian or rigid parenting approaches can exacerbate demand avoidance tendencies, while collaborative and empathetic approaches can create a more supportive environment for PDA children.
- Early experiences: Traumatic or stressful experiences, especially in early childhood, can contribute to anxiety and a heightened need for control, potentially fueling demand avoidance behavior.
- Social communication and interaction: Navigating social demands and expectations can be overwhelming for children and teens with PDA, leading them to withdraw or resist social situations further.
It's important to remember that PDA is not caused by poor parenting or a child's choice. It's a complex profile with multifaceted origins. While the specific factors may vary from case to case, understanding these potential contributors can help develop tailored support strategies for children with PDA to improve their quality of life.
The Pathological Demand Avoidance syndrome is often seen in conjunction with other conditions like ASD, ADHD, and anxiety disorders. This highlights the intertwined nature of developmental disorders and the importance of early identification and a holistic approach to diagnosis and support.
Supporting People with PDA
Living with PDA can be incredibly challenging for both children and their families. Every child with PDA traits is unique. What works for one may not work for another. Patience, understanding, and a collaborative approach are key to supporting children with PDA.
Here are some tips for parenting a child with PDA:
- Don’t personalize the behavior. Children with PDA aren’t acting like this on purpose and when you understand that, it is easier to have empathy.
- Focus on collaboration. Avoid power struggles and prioritize offering choices and negotiating routines together.
- Provide structure and predictability. Having clear expectations and consistent routines can help manage anxiety.
- Emphasize positive reinforcement. Reward effort and cooperation to build confidence and motivation.
- Make them comfortable in role play and pretend to handle social situations better.
- Seek professional support. Therapists specializing in PDA can provide valuable guidance and strategies for managing avoidance of demand, including Cognitive behavioral therapy sessions.
The BrainBehaviorResetTM Program uses natural, science-backed methods to help kids with PDA and ASD. It works by understanding how their brain functions and uses neurofeedback, behavior modification, PEMF, and magnesium supplements to manage the condition. Long-term outcomes include being able to handle their feelings better, learning how to talk with others, and just feeling happier despite being exposed to different environments.
Parent Action Steps
☐ Learn more about emotional regulation by listening to my podcast, It’s Gonna Be OK!
☐ Foster open communication with your child and address defiance through clear expectations and positive reinforcement.
☐ Prioritize building emotional regulation skills to help your child manage their feelings in challenging situations.
☐ Support the development of social skills and employ interventions accordingly.
☐ Join support groups to overcome social challenges and address PDA behaviors with the help of other parents and different people who went through the same struggles.
☐ Seek guidance from healthcare professionals for accurate diagnosis and effective intervention plans.
☐ Take the Solutions Matcher to get personalized treatment for your child.
Citations
Christie, P. (2012). Understanding pathological demand avoidance syndrome in children : a guide for parents, teachers, and other professionals. Jessica Kingsley Publishers.
Good, L. (2016, December 1). Parental illness representations in pathological demand avoidance syndrome: parental coping, parenting stress, parental wellbeing and the child-parent relationship. Etheses.bham.ac.uk. https://etheses.bham.ac.uk/id/eprint/6997/
Dr. Roseann is a mental health expert who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind New Research Highlights Key Differences Among Autistic Boys and Girls
- She Knows 11 Products Moms of Kids With ADHD Swear By to Maintain Order in the Chaos
- Very Well Mind What Is Asperger Syndrome?
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024










