Both Pathological Demand Avoidance (PDA) and AuDHD (co-occurring Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder) involve complex neurodevelopmental differences that can manifest in overlapping ways.
Interestingly, both conditions are profiles of autism and ADHD, but they manifest differently. Understanding the complexities of each condition is crucial for providing appropriate support and navigating challenges effectively.
PDA: Defying Demands, Seeking Control
PDA, also called Extreme Demand Avoidance, is characterized by an intense aversion to demands and expectations. People with PDA often exhibit oppositional behavior, meltdowns, and significant social difficulties (Newson, 2003).
Key features of PDA include:
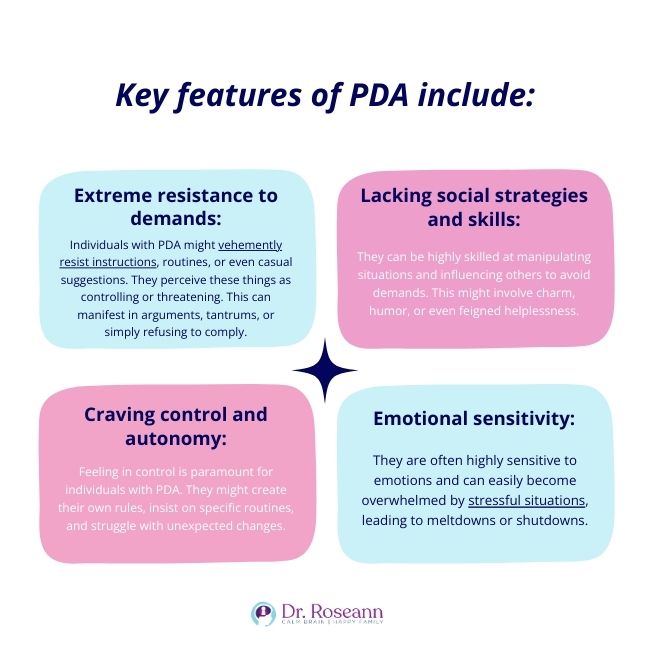
- Extreme resistance to demands: Individuals with PDA might vehemently resist instructions, routines, or even casual suggestions. They perceive these things as controlling or threatening. This can manifest in arguments, tantrums, or simply refusing to comply.
- Lacking social strategies and skills: They can be highly skilled at manipulating situations and influencing others to avoid demands. This might involve charm, humor, or even feigned helplessness.
- Craving control and autonomy: Feeling in control is paramount for individuals with PDA. They might create their own rules, insist on specific routines, and struggle with unexpected changes.
Emotional sensitivity: They are often highly sensitive to emotions and can easily become overwhelmed by stressful situations, leading to meltdowns or shutdowns.
AuDHD: A Blend of Challenges
AuDHD, refers to co-occurring ASD and ADHD. This mental health condition presents a unique set of challenges that blend aspects of both disorders (Leitner, 2014).
Common AuDHD features include:
- Social communication difficulties: Individuals with AuDHD may struggle with understanding and using nonverbal cues, initiating and maintaining conversations, and interpreting social rules. This can lead to misunderstandings and social isolation.
- Inattention and hyperactivity-impulsivity: Difficulty focusing, easily getting distracted, and impulsive behaviors are common challenges. This can impact academic performance, daily tasks, and relationships.
- Repetitive behaviors and restricted interests: Intense focus on specific topics or repetitive behaviors like hand flapping or rocking might be present. These can provide comfort and predictability, but can also interfere with daily life.
- Sensory sensitivities: Over- or under-responsiveness to sounds, lights, textures, tastes, or smells can be highly challenging, creating discomfort and impacting daily activities.
Features of PDA vs AuDHD: Overlapping and Distinct Traits
While PDA and AuDHD have distinct core features, they do share some overlapping areas that can sometimes make differentiating between them challenging. Here's a closer look at the common ground:
Social challenges: Both PDA and AuDHD can involve difficulties with understanding and using social cues, interpreting social rules, and maintaining relationships. Children and teens might struggle with initiating conversations, taking turns, and engaging in reciprocal social interactions. However, the underlying reasons behind these challenges may differ:
- PDA: The social difficulties associated with children with PDA often stem from a desire to avoid demands and maintain control, leading to manipulative behavior or withdrawal.
- AuDHD: Social challenges might be due to difficulties with processing non-verbal information, understanding social cues, and regulating emotions.
Emotional regulation: Both conditions can manifest in emotional meltdowns or outbursts, but the triggers and underlying reasons can vary:
- PDA: Meltdowns often occur in response to perceived demands or loss of control, with intense frustration and resistance.
- AuDHD: Meltdowns might be triggered by sensory overload, social anxiety, or difficulty managing frustration due to attention or hyperactivity challenges.
Executive functioning: PDA and AuDHD can involve difficulties with planning, organizing, and following through on tasks. This can impact daily life in areas like time management, completing routines, and staying organized.
Sensory sensitivities: While not a core feature of PDA, some individuals with PDA can experience over- or under-responsiveness to certain sensory inputs, similar to those with AuDHD. This can create discomfort and interfere with daily activities.
While some features of PDA and AuDHD overlap, there are also key distinctions:
- Demand avoidance: The core of PDA is the intense resistance to demands, while in AuDHD, social communication challenges and attention difficulties might be more prominent.
- Social skills: Individuals with PDA often exhibit strong social skills and adept manipulation, while those with AuDHD may experience more significant social difficulties.
- Emotional regulation: Emotional sensitivity and meltdowns are common in both conditions, but the triggers and underlying reasons might differ.
Pathological Demand Avoidance (PDA) vs and AuDHD – Autism spectrum disorder with Hyperactivity/Deficit Disorder
Diagnosis, Treatment, and Support
Currently, no specific criteria exist for diagnosing PDA, which leads to misdiagnoses as ASD or ADHD. On the other hand, AuDHD requires meeting diagnostic criteria for both ASD and ADHD. Specialized assessments by professionals familiar with PDA are crucial for accurate diagnosis, while AuDHD typically involves interviews, observations, and standardized tests for both conditions.
Building trust and reducing demand triggers are fundamental for managing PDA, alongside therapies like CBT adapted for PDA, play therapy, and sensory integration. Conversely, AuDHD treatment focuses on addressing core ASD and ADHD symptoms through also through CBT, along with social skills training, and occupational therapy.
Family support is crucial for both conditions, with PDA requiring understanding triggers and providing consistent support, while AuDHD families need to understand both ASD and ADHD and create a structured environment.
The BrainBehaviorResetTM Program can help address the underlying symptoms of any subtype of autism and ADHD through natural therapies such as neurofeedback, PEMF, and magnesium supplementation. With these science-backed methods, there will be less to no dependence on medications, which can be detrimental to a child’s developing brain.
PDA and AuDHD require specialized support and understanding. Consulting a qualified mental health professional with expertise in neurodevelopmental conditions is crucial for accurate diagnosis and developing appropriate interventions.
Parent Action Steps
☐ Listen to my podcast, It’s Gonna Be OK! ADHD podcast series and Autism episodes.
☐ Remember that each child’s experience is unique and requires a personalized approach.
☐ Focus on your child’s strengths and challenges, not just the diagnosis.
☐ Celebrate progress and offer ongoing support along the journey.
☐ Use the Solutions Matcher to get personalized help for your child.
Citations
Leitner, Y. (2014). The Co-Occurrence of Autism and Attention Deficit Hyperactivity Disorder in Children – What Do We Know? Frontiers in Human Neuroscience, 8(268). https://doi.org/10.3389/fnhum.2014.00268
Newson, E. (2003). Pathological demand avoidance syndrome: a necessary distinction within the pervasive developmental disorders. Archives of Disease in Childhood, 88(7), 595–600. https://doi.org/10.1136/adc.88.7.595
Dr. Roseann is a mental health expert who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind New Research Highlights Key Differences Among Autistic Boys and Girls
- She Knows 11 Products Moms of Kids With ADHD Swear By to Maintain Order in the Chaos
Very Well Mind What Is Asperger Syndrome?
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024











