For parents of autistic children, deciphering defiant behavior can be a confusing and isolating experience. Two conditions, Pathological Demand Avoidance (PDA) and Oppositional Defiant Disorder (ODD), often share surface similarities, causing further frustration in identifying the right support strategies.
Diagnostic Criteria: Is it PDA or ODD?
What is PDA? PDA is a relatively new concept that falls within the Autism Spectrum Disorder (ASD) umbrella. Children with PDA and autism are characterized by their extreme avoidance of everyday demands. Kids with the PDA profile exhibit pervasive anxiety around control and persistent demand for autonomy.
While defying instructions, they may resort to manipulation, negotiation, or meltdowns to maintain control. Social interaction can be intense, but difficulties with boundaries and rules are common. Because of this autism-PDA connection, PDA is sometimes referred to as demand avoidance autism or autistic demand avoidance.
But is ODD a form of autism? Autism and Oppositional Defiant Disorder are two distinct but oftentimes co-occurring conditions. It’s important to note that ODD is not categorized as ASD. ODD is marked by defiant behavior towards authority figures, often fueled by anger and a desire to test limits (Pondé et al., 2017).
While defiance in PDA children can be considered a pervasive developmental disorder, kids with ODD may only display it in specific situations or with certain individuals. Their social communication patterns are typically less affected.
Pathological Demand Avoidance (PDA) and Oppositional Defiant Disorder (ODD):

Motivation: Peering Beneath the Surface
Understanding the “why” behind the behavior is crucial when comparing PDA vs ODD. The huge difference between ODD and PDA is that the defiance in PDA individuals stems from an anxiety-driven need to avoid feeling controlled or trapped. They fear loss of autonomy and overwhelming sensory experiences. In contrast, ODD's defiance is generally linked to power struggles and expressing anger or frustration.
Pathological Demand Avoidance vs Oppositional Defiant Disorder Treatments
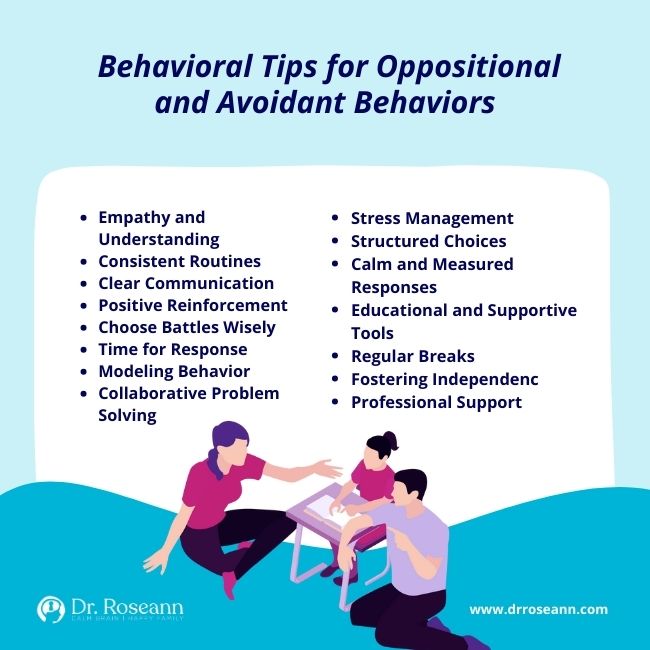
Traditional parenting methods often backfire for PDA in teens, as their defiance is not about willful disobedience. Strategies for PDA focus on understanding triggers, offering choices and control, employing collaborative communication, and building trust. Visual aids, social stories, and role-playing exercises can be invaluable (Christie, 2012).
On the other hand, children with ODD may respond better to methods such as rewards and consistent discipline for oppositional behaviors. Teaching them emotional regulation skills can help them manage frustration and express their needs more effectively.
The Intersection: Blurred Lines and Co-occurrence
When kids have both Pathological Demand Avoidance and Oppositional Defiance Disorder, things can get very tricky. Having PDA traits means feeling super anxious and saying no to the regular stuff you have to do, while ODD is about always saying no to adults. So, if a PDA child has ODD, it can seem like they're acting in a different way that doesn't make sense.
To figure this out, experts need to look at all the different things going on. They check out how the child acts, thinks, and feels to understand what's happening. Parents and professionals have to do this carefully, or it will not be easy to get the right answers. If that happens, it becomes harder for the child to get the help they need.
How to Treat Pathological Demand Avoidance and Oppositional Defiant Disorder
The treatment for PDA autism and ODD typically involves a collaborative approach and may include a combination of behavioral, educational, and therapeutic interventions. It's important to work closely with healthcare professionals including occupational therapists to develop an individualized treatment plan.
Consider neurofeedback as a potential complementary approach for treating these conditions by regulating brain activity. Focus on individualized protocols, consistency, and integration with other therapies. Neurofeedback can help your child, whether they have PDA, ODD or autism.
Additionally, parents may use a PEMF device with appropriate specifications, considering frequency, intensity, and duration of treatment that are tailored to the child’s needs. Maintain consistent and appropriate usage of the PEMF device, following recommended protocols for frequency and duration.
The regular intake of magnesium will also be helpful, as it can address certain mental health conditions, such as anxiety and mood disorders, which are prevalent in PDA, ODD and ASD. Consult with a clinical psychologist about the right magnesium type, frequency, and dosage your child needs.
Supporting A Child With Oppositional Defiant Disorder vs Pathological Demand Avoidance Syndrome
Regardless of the label, both children with PDA and ODD require understanding, empathy, and individualized support. ODD and PDA parenting means recognizing the nuances of their motivations and anxieties is key to unlocking effective interventions. By acknowledging the unique challenges faced by autistic people, we can create a world where they can thrive.
The support strategies for Pathological Demand Avoidance and Oppositional Defiant Disorder are different. For a PDA kid, focus on understanding their triggers and anxiety, offering choices and control, using collaborative communication, and building trust.
If your child has the ODD conduct disorder, implement consistent discipline, teach emotional regulation skills, and focus on positive reinforcement for desired behaviors. These are what work for Oppositional Defiant Disorder vs PDA.
Navigating the terrain of defiance in autistic children can be complex. While having a PDA and ODD diagnosis requires understanding and positive support plans, the appropriate approach will differ based on the underlying cause and motivation. If you suspect your child might have either condition, seeking professional help, evaluation and guidance is crucial.
What is P.D.A.?
P.D.A. can refer to “Pathological Demand Avoidance,” a behavioral profile associated with extreme avoidance of everyday demands. As a pervasive defiant disorder, it is often observed in individuals with autism spectrum disorder, though there is no officially recognized PDA diagnosis in the statistical manual of mental disorders.
Is PDA the same as ODD?
The PDA mental disorder is characterized by extreme avoidance of demands associated with overwhelming anxiety, often observed in individuals with autism, whereas ODD involves persistent defiant behaviors directed toward authority figures and is a distinct diagnosis not exclusive to autism.
What does PDA mean in Autism?
Pathological Demand Avoidance in autism or simply PDA autism is commonly used to describe the unique challenges faced by individuals on the autism spectrum who exhibit pathological demand avoidance behaviors. An autistic with PDA often struggles with traditional strategies for managing behavior and reacting strongly to demands, requests, or seemingly simple tasks.
Can a Child Have PDA Without Autism?
There is ongoing debate among professionals about whether PDA can exist independently of autism. In clinical practice, children may exhibit pathological avoidance without meeting all the criteria for a traditional autism diagnosis.
What's the Difference Between Oppositional Defiant Disorder and Conduct Disorder?
Oppositional Defiant Disorder (ODD) involves defiant and resistant behaviors toward authority figures, while Conduct Disorder (CD) encompasses more severe antisocial behaviors and rule violations, often leading to significant disruptions and potential legal consequences.
Does My Child Have PDA?
To know if your child has PDA, conduct a comprehensive assessment with a qualified mental health professional and consider various factors and behaviors. Observing your child's behavior in different settings and noting specific challenges can also be helpful information to share with the healthcare professional.
Are the PDA Symptoms in Adults Same as PDA in Kids?
The Pathological Demand Avoidance profile has been primarily observed and studied in children. While some characteristics associated with PDA may persist into adulthood, it's crucial to note that research on PDA in adults is limited, and the presentation of Pathological Demand Avoidance symptoms may vary. To know for sure, ask a professional for an Extreme Demand Avoidance Questionnaire or PDA test for adults.
Parent Action Steps
☐ Dive into your child's body language and motivations behind their demand avoidance behaviors to the extreme extent to determine if it’s ODD or PDA in autism.
☐ If you’re weighing ODD vs PDA disorder in your child because they avoid demands, seek expert evaluation and guidance for insights, diagnosis, and appropriate support strategies.
☐ Tailor support based on your child's social skills, motivation, ODD or PDA anxiety, and defiance disorder.
☐ Recognize the key difference between PDA and ODD and use the right parenting methods for each.
☐ Take the Pathological Demand Avoidance test to check if your child has PDA.
☐ Use the Solutions Matcher to get a personalized treatment for your child.
Citations
Christie, P. (2012). Understanding Pathological Demand Avoidance Syndrome In Children : A Guide For Parents, Teachers And Other Professionals. Jessica Kingsley Publishers.
Pondé, M. P., Matos, M. L., & Oliveira, C. C. P. B. de. (2017). Prevalence Of Attention-Deficit/Hyperactivity Disorder, Oppositional Defiant Disorder And Conduct Disorder In Children With Autism Spectrum Disorder. Brazilian Journal of Medicine and Human Health, 5(2), 39–46. https://doi.org/10.17267/2317-3386bjmhh.v5i2.1199
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
The Pathological Demand Avoidance Checklist
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024










