AuDHD stands for Autism and ADHD. The use of the term indicates someone has comorbid Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactivity Disorder (ADHD). There are no official diagnostic criteria for it under the Statistical Manual of Mental Disorders yet, but the term is commonly used by the Autistic and ADHD communities to describe their unique experiences.
However, ASD and ADHD are official diagnoses. In essence, children with AuDHD meet the criteria of these two neurodevelopmental conditions. As co-occurring conditions the child experiences symptoms of both ASD and ADHD and the overlap can be complex and unique, as symptoms from one condition might influence the other (Young et al., 2020).
Autism Spectrum Disorder is a neurodevelopmental disorder affecting social interactions, communication, and repetitive behaviors. Autistic people may experience sensory sensitivities, difficulties with executive functioning, and strong interests in specific topics.
On the other hand, Attention Deficit Hyperactivity Disorder is characterized by inattention, hyperactivity, and impulsivity. Children and teens with ADHD may struggle with focusing, staying organized, and controlling their emotions.
How Does AuDHD Affect a Child?
If you're a parent concerned about your child exhibiting signs of both ADHD and Autism, understanding AuDHD can be both overwhelming and enlightening. Here are things that you need to know about it:
1. Social Stigma
Unfortunately, an autistic person with ADHD is often misunderstood and stigmatized. Individuals with AuDHD may face twice as many societal challenges and they require more awareness and acceptance (Gabra & Hashem, 2021).
2. Diagnosis
A thorough assessment by a qualified professional is crucial for ASD and ADHD. Diagnosing ADHD and ASD accurately ensures that parents get access to appropriate support and resources.
3. Support
Connecting with the AuDHD community can be extremely valuable for individuals and their families. Sharing experiences, finding resources, and receiving peer support can significantly improve well-being.
Understanding AuDHD in Children
The common ADHD symptoms include inattention, difficulty focusing, hyperactivity, impulsivity, trouble with organization, executive dysfunction, and emotional regulation challenges. ASD symptoms, on the other hand, are difficulties with social cues, restricted special interests, repetitive behaviors, sensory sensitivities, and atypical processing of information. The combination of these two characterizes AuDHD.
Children and teens with AuDHD will encounter challenges at home and school. While separate conditions, both can affect one's daily life, learning, person-to-person interactions, and emotional well-being. They may struggle with routines and instructions, managing meltdowns, and building friendships.
For these children, the importance of seeking professional help should be emphasized. Getting a qualified professional assessment at an early age is crucial. Doing so helps you understand your child's specific needs and guides you toward appropriate support and interventions.
A team of specialists like pediatricians, developmental psychologists, occupational therapists, and educational professionals can work together to create a personalized treatment plan for your child.
How to Support a Child with Autism and ADHD
While having a diagnosis of comorbid ADHD and ASD, you're not alone in this journey. Having the right knowledge, support network, and access to professional help can empower you to navigate the challenges and ensure your child's well-being with AuDHD. Here are different ways to cope with it:
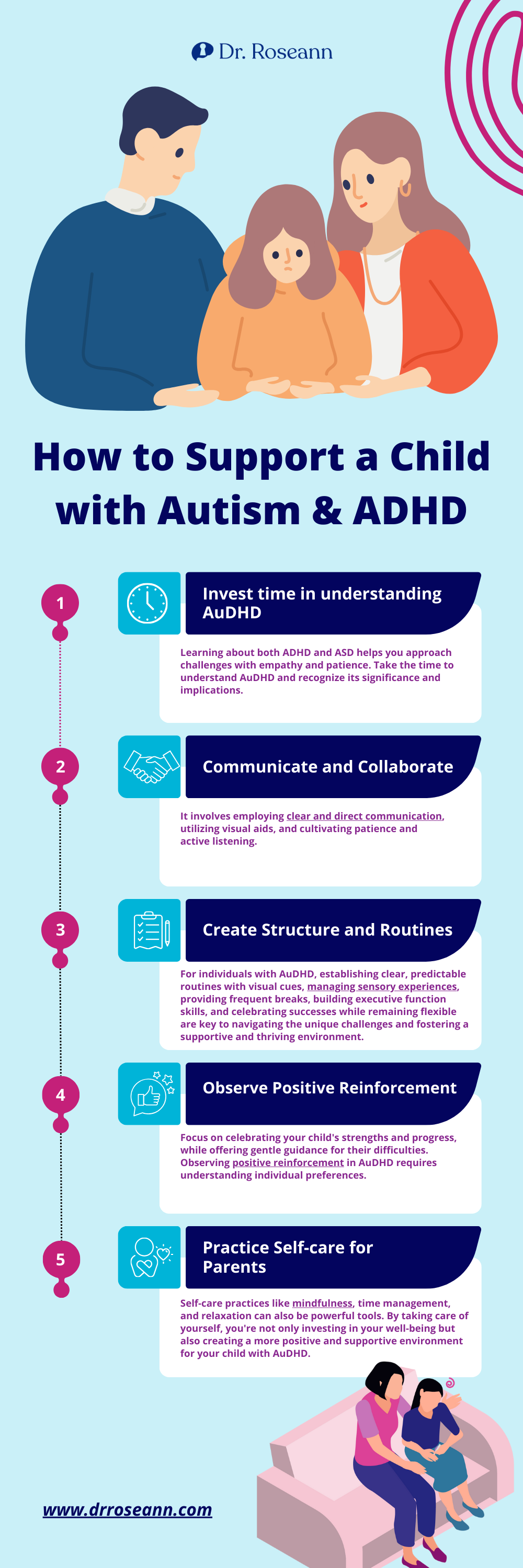
1. Invest time in understanding AuDHD
Learning about both ADHD and ASD helps you approach challenges with empathy and patience. Take the time to understand AuDHD and recognize its significance and implications. As a parent, your commitment to learning not only enhances personal growth but also promotes a society that values and accommodates diverse needs. It can also lead to fostering a culture of empathy and understanding.
2. Communicate and Collaborate
Fostering effective communication and collaboration is crucial for creating supportive environments. Recognizing the unique characteristics of individuals with AuDHD, such as varying attention spans and social communication differences, is pivotal.
It involves employing clear and direct communication, utilizing visual aids, and cultivating patience and active listening. Additionally, collaborative efforts among educators, healthcare professionals, caregivers, and individuals with AuDHD enhance understanding and address challenges, creating a more inclusive and accommodating space.
3. Create Structure and Routines
For individuals with AuDHD, establishing clear, predictable routines with visual cues, managing sensory experiences, providing frequent breaks, building executive function skills, and celebrating successes while remaining flexible are key to navigating the unique challenges and fostering a supportive and thriving environment.
4. Observe Positive Reinforcement
Focus on celebrating your child's strengths and progress, while offering gentle guidance for their difficulties. Observing positive reinforcement in AuDHD requires understanding individual preferences.
Notice what motivates your child and personalize rewards like sensory experiences, activities, or visual cues. Clearly define goals, offer immediate and specific praise linked to behavior, and monitor responses to adjust strategies.
Remember, a positive and supportive environment, where successes are celebrated and trust is built, is key to maximizing the effectiveness of positive reinforcement for individuals with AuDHD.
5. Practice Self-care for Parents
Being a parent to a child with AuDHD can be both rewarding and challenging. To support your child optimally, prioritizing self-care for every family member is crucial. This means acknowledging your own needs and taking time for activities that help you recharge and manage stress. Group therapy may help in building coping mechanisms and addressing autistic burnout.
Think of it as filling your cup first, so you can better pour into your child's. The first step is to prioritize getting enough sleep, doing physical activities, and enhancing social connections. Don't hesitate to seek medical advice from mental health professionals if needed. Remember, delegating tasks and asking for help are not signs of weakness, but strength in knowing you can't do it all alone.
Self-care practices like mindfulness, time management, and relaxation can also be powerful tools. By taking care of yourself, you're not only investing in your well-being but also creating a more positive and supportive environment for your child with AuDHD.
Parent Action Steps:
☐ Listen to my podcast, It’s Gonna Be OK! ADHD podcast series and Autism episodes.
☐ Foster empathy and patience for your AuDHD child's complex condition.
☐ Recognize and address the unique characteristics of the ADHD and autistic brain.
☐ Manage your child’s sensory input and sensory overload experiences, especially in social settings.
☐ Celebrate your kid’s strengths and progress despite their ADHD and autism diagnosis.
☐ Work 1on1 with Dr. Roseann through the BrainBehaviorResetTM Program.
☐ Use the Solutions Matcher to get appropriate treatment and personalized help for your child.
Citations
Gabra, R. H., & Hashem, D. F. (2021). Comparison of caregivers’ characteristics, stigma, and disease burden of children with autism spectrum disorder and attention-deficit disorder in Egypt. Middle East Current Psychiatry, 28(1). https://doi.org/10.1186/s43045-021-00162-0
Young, S., Hollingdale, J., Absoud, M., Bolton, P., Branney, P., Colley, W., Craze, E., Dave, M., Deeley, Q., Farrag, E., Gudjonsson, G., Hill, P., Liang, H., Murphy, C., Mackintosh, P., Murin, M., O’Regan, F., Ougrin, D., Rios, P., & Stover, N. (2020). Guidance for Identification and Treatment of Individuals with Attention-Deficit Hyperactivity Disorder and Autism Spectrum Disorder Based upon Expert Consensus. BMC Medicine, 18(146). https://doi.org/10.1186/s12916-020-01585-y
Dr. Roseann is a mental health expert who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind New Research Highlights Key Differences Among Autistic Boys and Girls
- She Knows 11 Products Moms of Kids With ADHD Swear By to Maintain Order in the Chaos
- The Healthy 12 Silent Signs of Adult ADHD You Might Be Ignoring
- Very Well Mind What Is Asperger Syndrome?
- Seeme & Liz 12 Essential Parenting Tips For Kids with ADHD
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023