In the often perplexing world of parenting, one of the most challenging paths to navigate is that of raising a child with ADHD and anxiety. These little warriors are on a unique journey, and as parents, our role is not only to support them but also to make informed decisions about effective treatment options.
First things first, let's demystify the intertwined enigma of ADHD and anxiety in children. ADHD, or Attention Deficit Hyperactivity Disorder, is a neurodevelopmental condition characterized by persistent patterns of inattention alone or combined with hyperactivity and impulsivity.
Comorbid anxiety disorders often lurk in the shadows of ADHD. It happens because of the constant reminders to pay attention and finish tasks. That means your child isn’t just dealing with one hurdle. They're jumping a double-barrelled obstacle course, and that is not an easy feat.
Common Medication Treatments for Children with ADHD
Traditionally, when parents learn that their child has a diagnosis of ADHD, their minds tend to lean towards one solution – prescription medications. Common ADHD medications include stimulants like Ritalin, Adderall, and Concerta. Selective Serotonin Reuptake Inhibitors (SSRIs) like Celexa, Lexapro, and Prozac are considered as well.
But while stimulant and non-stimulant medications are often included in treatment plans for ADHD to enhance attention and reduce hyperactivity, their role in managing anxiety in children with ADHD is a bit more complex. You see, anxiety and ADHD can intertwine in complicated ways. When it comes to anxiety, they aren’t the best choices.
Stimulant medications can exacerbate anxiety symptoms. It's not uncommon for younger children with ADHD to experience heightened social anxiety as a side effect of these ADHD drugs. It can manifest as increased nervousness, restlessness, or even full-blown panic attacks. The stimulant effect of these medications can sometimes mimic the symptoms of anxiety and create a challenging situation where it's hard to distinguish between the two.
Furthermore, drug administration offers a relatively short duration of action, which means you may need to administer multiple doses throughout the day. Doing so can lead to a rebound effect or what I like to call the “roller coaster effect”, where the child experiences a surge of medication-induced focus followed by a crash, which could increase their feelings of anxiety and irritability.
It's essential to note that while stimulant medications can affect anxiety, they don't address the underlying causes of anxiety disorders. They might help a child temporarily concentrate better in school, but they won't necessarily equip them with the coping strategies needed to manage anxiety in different life situations. Anxiety often requires a tailored and holistic approach for effective management.
In some cases, children with ADHD might be prescribed different medications to manage their anxiety alongside stimulants. However, this polypharmacy approach can introduce more complexity and serious side effects, which may not always be in the best interest of your child's long-term well-being.
Debunking the Effectiveness of Stimulant Medications for Anxiety in Children with ADHD
Some parents might assume that since stimulants may improve attention, they could also help with anxiety in children with ADHD. However, reality paints a different picture. The American Academy of Pediatrics states that stimulant medications are not recommended as a primary treatment for anxiety disorders in children with ADHD (American Academy of Pediatrics, 2011). They might even exacerbate anxiety symptoms in some cases.
These stimulant medications work by altering the levels of certain neurotransmitters in the brain, such as dopamine and norepinephrine. They essentially rev up the brain's engine to help children with ADHD pay attention, rein in impulsive behaviors, and manage hyperactivity. For many children, these medications affect their daily life.
However, it's crucial to recognize that while some stimulant medications may seem to provide little benefits, they are not the solution for everyone. Responses to these medications can vary widely from one child to another. Some children may see only modest gains or encounter side effects that outweigh whatever they may seem to provide.
The common side effects of ADHD medications can include:
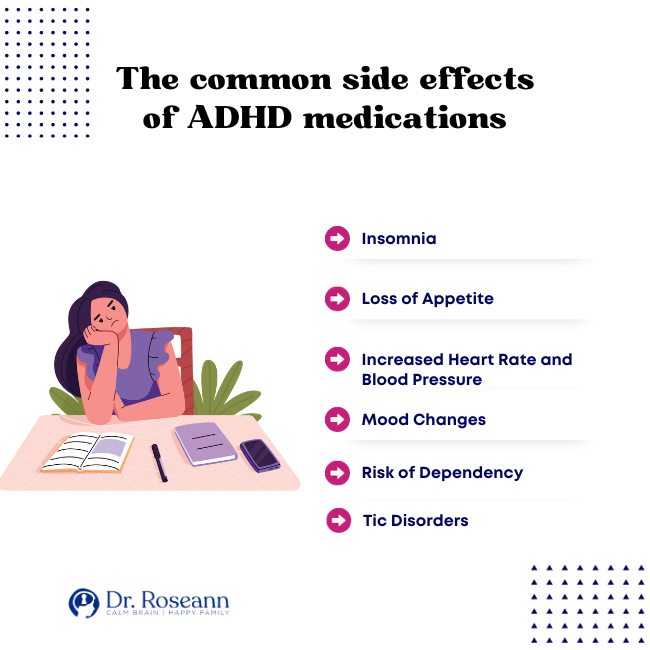
- Insomnia – Stimulants can disrupt sleep patterns, making it challenging for children to get the rest they need for healthy development.
- Loss of Appetite – These medications can suppress appetite and lead to potential issues with growth and weight gain. Weight loss can be an alarming issue for growing kids.
- Increased Heart Rate and Blood Pressure – Stimulants can put added strain on the cardiovascular system, which can be a concern for some children with preexisting heart conditions.
- Mood Changes – While stimulants can improve mood in some cases, they can also lead to mood swings, irritability, or emotional blunting in others.
- Risk of Dependency – Although the risk is relatively low when prescribed and taken as directed, stimulant medications have the potential for misuse and dependency, particularly in older adolescents.
- Tic Disorders – In rare cases, stimulants can exacerbate or trigger tics, which can be distressing for children and their families.
Exploring Natural Alternatives for Managing Anxiety in Children with ADHD
If stimulant medications aren’t the best for your kids, what's the alternative? Can you still help your child without the risks associated with stimulant and non-stimulant medications? Of course!
There are natural solutions that offer a plethora of possibilities to support brain health, enhance attention, stabilize mood, combat stress, and manage behavior. Here are some science-backed, safe, and effective treatment options:
Biofeedback
Biofeedback techniques can help children learn to control physiological functions like heart rate and muscle tension. This self-regulation tool can be particularly beneficial for managing your child's anxiety (Monastra et al., 2006).
Through biofeedback, individuals learn how to modify their physiology to improve their physical, mental, emotional, and spiritual well-being. Patients are required to participate actively in biofeedback training and to practice regularly between sessions, similar to physical therapy.
Using stress management training, clinical biofeedback can manage disease symptoms and improve overall health and wellness. Many people in the United States are using biofeedback and other natural therapies for their routine healthcare following research showing that biofeedback interventions are effective in treating different medical and mental health conditions (Frank et al., 2010).
Neurofeedback
The National Institute of Mental Health defines neurofeedback as a type of biofeedback that enables individuals to control their brain function by measuring brain waves and receiving feedback. Neurofeedback is known as a complementary and alternative treatment option for many brain conditions (Marzbani et al., 2016).
This non-invasive technique involves monitoring and training brain activity to improve self-regulation. Neurofeedback has shown promise in helping children with ADHD develop better focus and emotional control (Bakhshayesh et al., 2011).
Behavior Therapy
Behavioral interventions, like Applied Behavior Analysis (ABA) and Social Skills Training, can help children develop essential life skills, improve emotional regulation, and reduce anxiety.
One of the shining stars in the world of natural interventions is Cognitive-Behavioral Therapy (CBT).
Cognitive Behavioral Therapy is a structured and goal-oriented approach that has shown remarkable efficacy in reducing anxiety symptoms in children with ADHD. CBT equips kids with the tools they need to cope with anxiety, addressing the root causes rather than merely masking the core symptoms of ADHD (Miranda & Jesus Presentacion, 2000).
Parent Training
Equipping parents with strategies to support their children with ADHD and anxiety can be incredibly beneficial. Parent training programs can teach effective communication, behavior management techniques, and ways to create a supportive home environment (van den Hoofdakker et al., 2007).
According to the American Psychiatric Association, younger children should use behavioral strategies in the form of parent management training and school intervention as first-line treatments for ADHD. Evidence-based Parent-Child Interaction Therapy (PCIT) helps young children with ADHD and Oppositional Defiant Disorder (Parekh, 2017).
Nutritional Supplements
Some nutritional and herbal supplements, like magnesium and ginkgo biloba, are thought to have cognitive-enhancing properties. However, it's crucial to consult with a healthcare provider before introducing any supplements into your child's routine to ensure safety and efficacy.Research shows that there's a connection between low magnesium levels in the blood and ADHD. Children with ADHD tend to have slightly lower blood magnesium levels (Effatpanah et al., 2019). A healthy diet plus magnesium supplements can help alleviate ADHD symptoms in kids.
Tips for Parents in Managing ADHD and Anxiety in Their Children
Helping children with ADHD navigate the challenges of life can be both rewarding and demanding. When anxiety is thrown into the mix, it can make the journey even more complex. However, with the right strategies, lifestyle changes, and ample support, parents can play a pivotal role in effectively managing ADHD and anxiety symptoms in their kids. Here’s how:
1. Practice mindfulness and meditation
These practices have gained substantial recognition for their positive effects on attention and emotional regulation. Mindfulness exercises, such as deep breathing and guided meditation, can help children with ADHD and anxiety build greater self-awareness and develop techniques to symptoms effectively.
2. Make dietary adjustments
Nutrition plays a vital role in brain health. Consider incorporating foods rich in Omega-3 fatty acids, such as salmon and flaxseeds, which have been associated with improved attention and mood. Reducing processed foods and sugars can also contribute to more stable energy levels. Certain foods, like those rich in Omega-3 fatty acids, have been linked to improved attention.
3. Engage in physical activities
Regular exercise isn't just essential for physical health; it also has a profound impact on mental well-being. Encourage your child to engage in activities they enjoy, whether it's playing sports, dancing, or simply going for a walk. Exercise releases endorphins, which can help reduce anxiety.
4. Get adequate sleep
Prioritize a consistent sleep schedule and ensure your child gets enough rest. Sleep is essential for cognitive functioning, mood stability, and overall health. A well-rested child is better equipped to manage the challenges of ADHD and anxiety.
5. Initiate environmental modifications
Make adjustments at home and in school to create an environment that minimizes distractions and supports your child's specific needs. It might include installing designated study areas, using noise reduction tools, and creating organization systems.
6. Create a structured routine
Establishing a consistent daily routine can provide a sense of security and predictability for children with ADHD and anxiety. Their routine should include set times for meals, homework, play, and bedtime. Visual schedules or checklists can help them understand and follow the routine.
7. Break tasks into smaller steps
Children with ADHD may become overwhelmed by tasks that seem too large or complex. Break assignments or chores into smaller, manageable steps, and provide clear instructions. This can reduce frustration and anxiety.
8. Create a calm space
Designate a quiet and clutter-free area where your child can retreat when they need a break. Stock it with calming activities like coloring books, puzzles, or sensory tools. This space can serve as a haven during moments of overwhelm.
9. Limit screen time
Excessive screen time can exacerbate ADHD symptoms and anxiety. Set reasonable limits on screen use, especially before bedtime. Encourage other activities like reading, playing outside, or pursuing hobbies.
10. Foster effective communication
Foster open and honest communication with your child. Encourage them to express their feelings and concerns, and actively listen without judgment. Knowing they can talk to you about their struggles can alleviate anxiety.
Parents must recognize that this journey is both challenging and rewarding. Embracing a comprehensive approach that combines evidence-based treatments, natural alternatives, and parental support is key to helping your child thrive. If you're seeking a structured program that integrates these elements and provides expert guidance, consider exploring the BrainBehaviorResetTM Program. This program offers a holistic and personalized approach to address the unique needs of children with ADHD and anxiety, focusing on their brain health and overall well-being. Remember, you're not alone in this journey, and with the right resources and support, you can help your child unlock their full potential and lead a fulfilling life.
Parent Action Steps
☐ Take the time to learn about ADHD and anxiety in children.
☐ Consider incorporating natural solutions into your child's routine.
☐ Find local therapists who offer CBT for children with ADHD and anxiety.
☐ Create a supportive and open communication channel with your child.
☐ Implement a structured daily routine.
☐ Set reasonable limits on screen use, especially before bedtime.
☐ Collaborate with your child's school to create a supportive learning environment.
☐ Encourage your child to build positive relationships with peers.
☐ Remember to take care of yourself.
☐ Implement a reward system to motivate your child.
☐ Keep a record of your child's symptoms, behaviors, and responses to treatments.
☐ Take this ADHD Quiz to know if your child has Attention-Deficit Hyperactivity Disorder.
☐ Use the Solutions Matcher to get personalized treatment for your child.
Citations
References American Academy of Pediatrics. (2011). ADHD: Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. PEDIATRICS, 128(5), 1007–1022. https://doi.org/10.1542/peds.2011-2654
Bakhshayesh, A. R., Hänsch, S., Wyschkon, A., Rezai, M. J., & Esser, G. (2011). Neurofeedback in ADHD: a single-blind randomized controlled trial. European Child & Adolescent Psychiatry, 20(9), 481–491. https://doi.org/10.1007/s00787-011-0208-y
Effatpanah, M., Rezaei, M., Effatpanah, H., Effatpanah, Z., Varkaneh, H. K., Mousavi, S. M., Fatahi, S., Rinaldi, G., & Hashemi, R. (2019). Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Research, 274, 228–234. https://doi.org/10.1016/j.psychres.2019.02.043
Frank, D. L., Khorshid, L., Kiffer, J. F., Moravec, C. S., & McKee, M. G. (2010). Biofeedback in medicine: who, when, why and how? Mental Health in Family Medicine, 7(2), 85–91. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2939454/
Marzbani, H., Marateb, H., & Mansourian, M. (2016). Methodological Note: Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications. Basic and Clinical Neuroscience Journal, 7(2). https://doi.org/10.15412/j.bcn.03070208
Miranda, A., & Jesus Presentacion, M. (2000). Efficacy of Cognitive-Behavioral therapy in the treatment of children with adhd, with and without aggressiveness. Psychology in the Schools, 37(2), 169–182. https://doi.org/10.1002/(sici)1520-6807(200003)37:2%3C169::aid-pits8%3E3.0.co;2-8
Monastra, V. J., Lynn, S., Linden, M., Lubar, J. F., Gruzelier, J., & La Vaque, T. J. (2006). Electroencephalographic Biofeedback in the Treatment of Attention-Deficit/Hyperactivity Disorder. Journal of Neurotherapy, 9(4), 5–34. https://doi.org/10.1300/j184v09n04_02
Parekh, R. (2017). What Is ADHD? American Psychiatric Association; American Psychiatric Association. https://www.psychiatry.org/patients-families/adhd/what-is-adhd
van den Hoofdakker, B. J., van der Veen-Mulders, L., Sytema, S., Emmelkamp, P. M. G., Minderaa, R. B., & Nauta, M. H. (2007). Effectiveness of Behavioral Parent Training for Children With ADHD in Routine Clinical Practice: A Randomized Controlled Study. Journal of the American Academy of Child & Adolescent Psychiatry, 46(10), 1263–1271. https://doi.org/10.1097/chi.0b013e3181354bc2
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Learn how to get your kid to listen and finish tasks in 30 days without the constant nagging and fighting. Get the EFT Toolkit now!
Empower yourself with natural solutions for your child's mental health and behavior. Download our FREE quick start guide and start supporting your child today.
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023










