ADHD are not the letters in your child’s alphabet soup, but a neurodevelopmental disorder that's enough to make any parent's head spin. It stands for Attention Deficit Hyperactivity Disorder and affects children and teens, often making their lives and the lives of their families a tad more complicated.
What exactly is Attention Deficit Hyperactivity Disorder (ADHD)? It's a condition characterized by a trio of symptoms: inattention, hyperactivity, and impulsivity. Picture a child who can't sit still, loses focus faster than a squirrel chasing a nut, and makes decisions without a second thought. Yes, that's ADHD.
Inattention manifests as difficulty staying on task, forgetfulness, and poor organizational skills. Hyperactivity means a child is a perpetual motion machine, constantly fidgeting and unable to stay put. Lastly, impulsivity is mostly acting first and thinking later, leading to impromptu escapades and oops moments.
Let me share Oscar's journey with ADHD, which began when he was seven years old. As a clinical psychologist specializing in this condition, it’s easy to recognize the early signs. Oscar's inattentive presentation often led to disorganized schoolwork and forgetfulness. Then his impulsive behavior made him the first to raise his hand in class but also got him into frequent trouble with his teachers.
The Importance of Early Diagnosis and Treatment for ADHD
Early ADHD diagnosis and treatment are crucial. Doing so gives children a compass for their life journey. Untreated ADHD can lead to all sorts of complications, from academic struggles and difficulties with social interactions to low self-esteem and even substance use disorders later in life.
The American Academy of Pediatrics recommends that mental health professionals use behavioral therapy as the first-line treatment for ADHD before they prescribe medication for children under 6 years old (CDC, 2022). Early intervention, and not drug administration, can set the stage for positive behaviors and better long-term outcomes.
However, medication is often the first thing that comes to mind when people think of ADHD treatment. Medications like Ritalin and Adderall can help manage symptoms by increasing focus and reducing impulsivity. But, and it's a big but, they come with their fair share of side effects.
Oscar's parents considered various treatment options, and medications were also discussed with them, but they were concerned about the serious side effects. Instead, they decided to explore non-medication and behavior therapy to give Oscar the best start and they produced momentous results.
The Side Effects of ADHD Medication Treatment
Let's discuss these side effects for a moment. Know that ADHD medications aren't the be-all and end-all solution for this condition. Some side effects of using medications for ADHD include decreased appetite, sleep problems, and, in rare cases, increased blood pressure and heart rate.
These side effects outweigh whatever good these medications provide. Plus, they’re not technically beneficial for a developing brain. Furthermore, even if they're said to be FDA-approved, there's a stigma. Some folks might look at you sideways when they learn your child is taking medication for ADHD.
There are two types of ADHD medications, particularly stimulant and non-stimulant variants. But both have their fair share of side effects, and their severity can vary from person to person Here’s a list of their most common ones:
Stimulant Medications (e.g., Methylphenidate, Amphetamine-based medications):
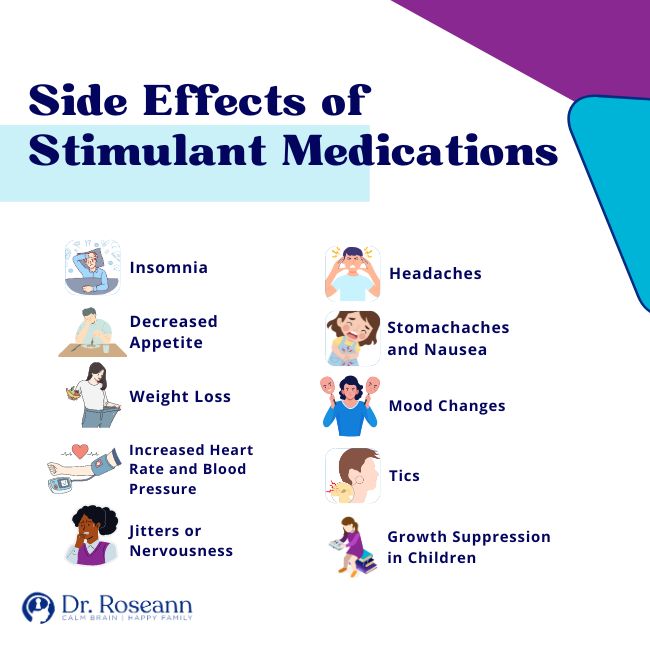
- Insomnia: Stimulants can interfere with sleep patterns, making it difficult to fall asleep or stay asleep.
- Decreased Appetite: Some children may experience reduced appetite, which can lead to other complications.
- Weight Loss: Due to decreased appetite, weight loss can occur in some individuals.
- Increased Heart Rate and Blood Pressure: Stimulants can raise heart rate and blood pressure, which may be of concern in individuals with certain heart conditions.
- Jitters or Nervousness: Some people may feel anxious or jittery when taking stimulant medications.
- Headaches: Headaches can occur as a side effect of stimulant use.
- Stomachaches and Nausea: Gastrointestinal discomfort, including stomachaches and nausea, can be side effects.
- Mood Changes: In some cases, individuals may experience mood swings or increased irritability.
- Tics: Stimulant medications may exacerbate or cause motor or vocal tics in some individuals.
- Growth Suppression in Children: There is some evidence that long-term use of stimulants can lead to slowed growth in children, although this effect is typically modest.
Non-stimulant Medications (e.g., Atomoxetine, Guanfacine, Clonidine):
- Drowsiness: Some non-stimulant medications can cause drowsiness, especially when initially starting treatment or adjusting the dosage.
- Dizziness: Dizziness or lightheadedness can occur in some individuals taking non-stimulant medications.
- Dry Mouth: Dry mouth is a common side effect of certain non-stimulant medications.
- Fatigue: Feeling tired or fatigued may occur as a side effect.
- Upset Stomach: Gastrointestinal side effects, such as upset stomach or constipation, can be experienced.
- Mood Changes: Some individuals may experience mood swings or changes in mood.
- Low Blood Pressure with Guanfacine and Clonidine: These medications can lower blood pressure, which can lead to dizziness upon standing.
Non-Medication Treatment Approaches for Attention
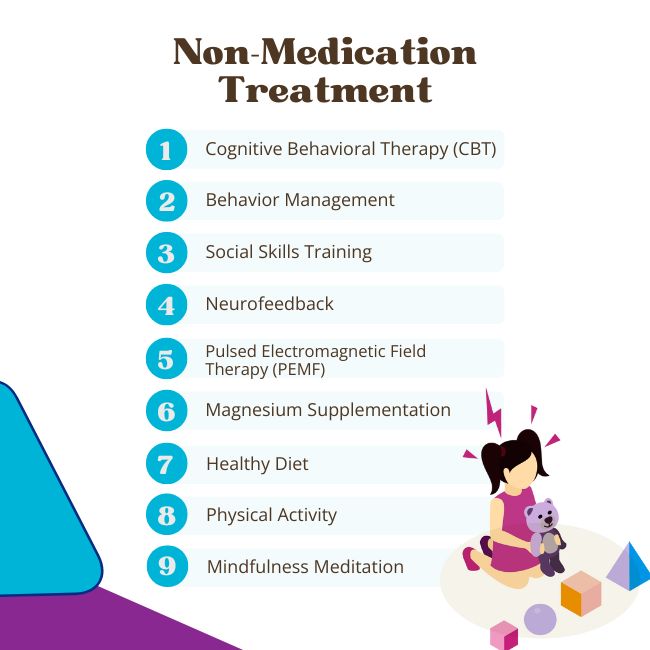
Medication isn't the only path for the treatment of ADHD. There's a world of non-medication treatment approaches that can offer valuable support and help young minds flourish. These alternatives are often chosen for their lower risk of side effects and their holistic approach to nurturing brain health.
Cognitive Behavioral Therapy (CBT)
CBT is a type of therapy that focuses on identifying and altering negative patterns of thinking and behavior. It equips children with practical tools to tackle their impulsivity, inattention, and hyperactivity. Think of it as rewiring the brain's circuitry for success.
With the guidance of a trained therapist, kids learn to recognize unhelpful thought patterns and replace them with more constructive ones. This not only improves their day-to-day functioning but also boosts their self-esteem and equips them to better handle the challenges that ADHD can throw their way (Sprich et al., 2016).
Behavior Management
Imagine transforming your child's daily life into a well-designed board game, complete with rewards and achievements. This is the essence of behavior management for ADHD. It's all about setting up a structured system to minimize problem behaviors and encourage positive ones.
One popular tool is setting up a rewards system. This nifty strategy involves tracking a child's behavior and performance throughout the day at home and in school. They earn points for completing tasks, staying focused, and controlling impulses. Rewards are then linked to these points, creating a tangible incentive to exhibit positive behaviors.
Social Skills Training
Navigating the complex waters of social interaction can be particularly challenging for children, teens, and adults with ADHD. Social skills training serves as their trusty compass, guiding them toward more successful social interactions.
In these sessions, kids and teens learn valuable skills like active listening, recognizing social cues, and responding appropriately to various social situations. Role-playing exercises help them practice these skills in a safe, controlled environment and boost their confidence in real-life scenarios.
Neurofeedback
Venturing into the realm of alternative treatments. Neurofeedback is like a mind workout for kids with ADHD. It's a type of biofeedback that focuses on training the brain to regulate its activity more effectively.
During neurofeedback sessions, electrodes are placed on the scalp to monitor brain wave patterns. When a child's brain produces desirable patterns associated with focus and calmness, they receive positive feedback, often in the form of a game or visual display. Over time, this process helps kids learn to control their brain activity, fostering an improved ability to pay attention and control impulses (Van Doren et al., 2018).
Pulsed Electromagnetic Field Therapy (PEMF)
PEMF therapy is an underutilized yet highly effective option. It involves exposing the body to low-frequency electromagnetic fields, which can stimulate brain function and reduce symptoms of ADHD.
Some individuals with ADHD have reported benefits from PEMF therapy. It's a non-invasive approach that holds promise as a complementary treatment as shown in the research by Pawluk and Layne (2017).
Magnesium Supplementation
Sometimes, a simple mineral can make a world of difference. Magnesium, often referred to as “nature's tranquilizer,” plays a crucial role in brain function and overall health. Some studies suggest that children with ADHD may have lower levels of magnesium in their bodies.
Supplementing with magnesium, under the guidance of a healthcare provider, can help support brain health and potentially reduce ADHD symptoms. Magnesium is involved in various processes, including neurotransmitter function and stress management, making it a valuable addition to a holistic ADHD management plan (Effatpanah et al., 2019).
Healthy Diet
When it comes to your child's brain, fuel matters. A diet rich in nutrients is like giving their brain a much-needed boost. Omega-3 fatty acids found in fatty fish like salmon, as well as in nuts and leafy greens, can be brain-boosting powerhouses. And don't forget the supporting cast of whole grains and lean protein – they're essential for a balanced mental diet.
Physical Activity
Think of physical activity as a secret weapon in your ADHD management arsenal. Beyond burning off extra energy, it's a mood enhancer and concentration booster. So, put on those sneakers, gather all family members, and embark on a hiking or biking adventure. It's not just exercise, but also an opportunity to create lasting memories together.
Mindfulness Meditation
Meditation isn't just for yogis. It's a skill that can transform your child's life. Mindfulness meditation is like giving them a mental toolkit that equips them with impulse control, stress reduction techniques, and emotional regulation skills. These tools not only help them navigate the challenges of ADHD but also lay the foundation for a calmer, more centered approach to life.
So, there you have it – a whirlwind tour through the maze of ADHD treatment options. Remember, there's no one-size-fits-all answer. What's crucial is that you, as a parent, have the power to make informed decisions that best suit your child's unique needs.
With the BrainBehaviorResetTM Program, these natural approaches to treating ADHD are customized to the needs of your child. With consistent neurofeedback sessions, at-home treatments, and nutrition supplementation, managing ADHD becomes a lot smoother.
Oscar's story is one of hope and determination. With the unwavering support of his parents, the guidance of skilled professionals, and a comprehensive ADHD treatment plan that included intensive holistic and alternative approaches, Oscar learned to harness his unique strengths.
As he grew older, Oscar's ADHD was not a hindrance but a part of his vibrant identity. The power of natural solutions and the potential within their child turned Oscar's ADHD journey into a remarkable adventure of growth and self-discovery. When given the right support, your child could flourish like Oscar.
ADHD might be a challenging journey, but with an effective treatment and a dash of hope, your child can thrive. Embrace the natural solutions, explore the therapies, and always believe in the potential of your child's remarkable brain. Together, you'll navigate the ADHD maze and emerge stronger on the other side.
Parent Action Steps
- Get informed about ADHD and seek professional help.
- Discuss the available treatment options with your healthcare provider.
- Promote a balanced and nutritious diet to support their brain health.
- Encourage regular physical activity for your child.
- Introduce mindfulness meditation to your family's routine.
- If appropriate, seek out cognitive behavioral therapy for your child.
- Explore behavior management strategies like time management.
- Research alternative therapies like neurofeedback and PEMF.
- Consider enrolling in parent training programs.
- Establish consistent routines and boundaries to provide structure and predictability.
- Be your child's advocate in school and healthcare settings.
- Embrace your child's journey.
- Answer this ADHD Quiz to know why your kid can’t focus, listen, or complete tasks.
- Take our Solutions Matcher to get personalized treatment for your ADHD child.
Citations
CDC. (2022, August 9). Treatment of ADHD. Centers for Disease Control and Prevention; CDC. https://www.cdc.gov/ncbddd/adhd/treatment.html
Effatpanah, M., Rezaei, M., Effatpanah, H., Effatpanah, Z., Varkaneh, H. K., Mousavi, S. M., Fatahi, S., Rinaldi, G., & Hashemi, R. (2019). Magnesium status and attention deficit hyperactivity disorder (ADHD): A meta-analysis. Psychiatry Research, 274, 228–234. https://doi.org/10.1016/j.psychres.2019.02.043
Pawluk, W., & Layne, C. (2017). Power Tools for Health. FriesenPress.
Sprich, S. E., Safren, S. A., Finkelstein, D., Remmert, J. E., & Hammerness, P. (2016). A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. Journal of Child Psychology and Psychiatry, 57(11), 1218–1226. https://doi.org/10.1111/jcpp.12549
Van Doren, J., Arns, M., Heinrich, H., Vollebregt, M. A., Strehl, U., & K. Loo, S. (2018). Sustained effects of neurofeedback in ADHD: a systematic review and meta-analysis. European Child & Adolescent Psychiatry, 28(3), 293–305. https://doi.org/10.1007/s00787-018-1121-4
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.