Obsessive-Compulsive Disorder is a mental health disorder characterized by uncontrollable and recurring thoughts, images, or impulses (obsessions), often followed by repetitive behaviors or mental acts (compulsions) to reduce anxiety or prevent perceived harm. At the root of OCD is an irrational fear that something terrible will happen if the person doesn’t complete a mental or physical ritual.
Conversely, eating disorders refer to a collection of mental disorders distinguished by atypical eating patterns, which may include inadequate or excessive food consumption and can harm a person's mental and physical well-being. Types of eating disorders include anorexia, bulimia, binge eating, and ARFID.
Understanding OCD
Obsessive Compulsive Disorder often presents differently in children than in adults. Among children, the common obsessions and compulsions are related to a variety of intrusive thoughts, as well as contamination (fear of germs or getting sick), order and symmetry (a need for things to be in a specific order or pattern), and harm (fear of causing harm to oneself or others).
Children with OCD often display OCD-related behaviors, such as avoidance behaviors, repetition, questioning, and a need for reassurance. They may engage in repetitive thoughts and behaviors such as excessive hand washing, checking and rechecking locks or appliances, counting, or repeating words or phrases in their heads.
Even though we think of OCD as a compulsion, such as handwashing, it always starts with intrusive thoughts. Their thinking becomes obsessive and “the OCD brain” begins to take control. Children may have difficulty controlling their thoughts or experience intrusive, unwanted, and distressing thoughts. Their thoughts can be pretty dark and scary, so they don’t share them.
OCD can affect children in several ways, including:
1. Academic Performance
Children with OCD may have difficulty concentrating in school due to obsessive thoughts and compulsive behaviors. Those with OCD often display perfectionistic tendencies, which affect their ability to turn in their schoolwork promptly or at all. They can be prone to excessive erasures, avoidant behavior, and emotional outbursts. Intrusive thoughts and rituals can affect their academic performance.
2. Social Functioning
OCD can interfere with a child's ability to socialize and make friends. As a result, they may avoid social situations for fear of being judged or criticized by others. It’s not unusual for a person with OCD to have obsessive thoughts about what others think about them or what they’ve said.
3. Family Relationships
OCD can create tension within families, as parents may not understand their child's behavior, and the child may become frustrated with their parent's lack of understanding. Families often get stuck trying to reason with OCD when it’s irrational. Moreover, children with OCD often get stuck on one or more family members and that person becomes part of their OCD thinking. This can be very hard on family relationships.
4. Physical Health
The compulsive behaviors associated with OCD, such as excessive hand washing, can lead to skin irritation and other physical health problems. With such a highly activated nervous system, it’s very common for someone with OCD to experience chest tightness, gastrointestinal difficulties, and sleep problems.
5. Emotional Well-Being
Children with OCD may experience significant anxiety, fear, and distress related to their obsessions and compulsions, affecting their emotional well-being. Their high-stress levels often lead to difficulties with emotional regulation and overly sensitive behaviors. With such high levels of activation, they often can’t sleep which further worsens their emotional state.
Understanding Eating Disorders
Eating disorders in children are a group of mental illnesses characterized by abnormal eating habits that can significantly impact a child's physical and emotional health. Eating disorders can occur in children of all ages but are most commonly diagnosed in adolescents and young adults as one enters puberty, and there’s more emphasis on the body.
Individuals with eating disorders may have more than one type. For example, it’s not uncommon for somebody to have anorexia nervosa and also display binge eating.
Common eating disorders in children and teens include:
1. Anorexia Nervosa
Teens with anorexia nervosa have an intense fear of gaining weight. They may limit their food intake, resulting in significant weight loss. They may also engage in excessive exercise or other behaviors to lose weight. For some with anorexia, body dysmorphia may be present first.
2. Bulimia Nervosa
Young adults with bulimia nervosa may binge eat, consume large amounts of food quickly, and then engage in purging behaviors such as vomiting or using laxatives to prevent weight gain.
3. Binge-Eating Disorder
Children with binge eating disorder may frequently devour large amounts of food and experience shame, guilt, or loss of control.
4. Avoidant Restrictive Food Intake Disorder (ARFID)
An apparent disinterest in food and eating characterizes ARFID. The avoidance is based on the sensory qualities of food or anxiety related to the adverse outcomes of eating. This avoidance behavior can lead to poor nutrition and/or weight loss due to the child's limited food intake.
Eating Disorder Symptoms in Children
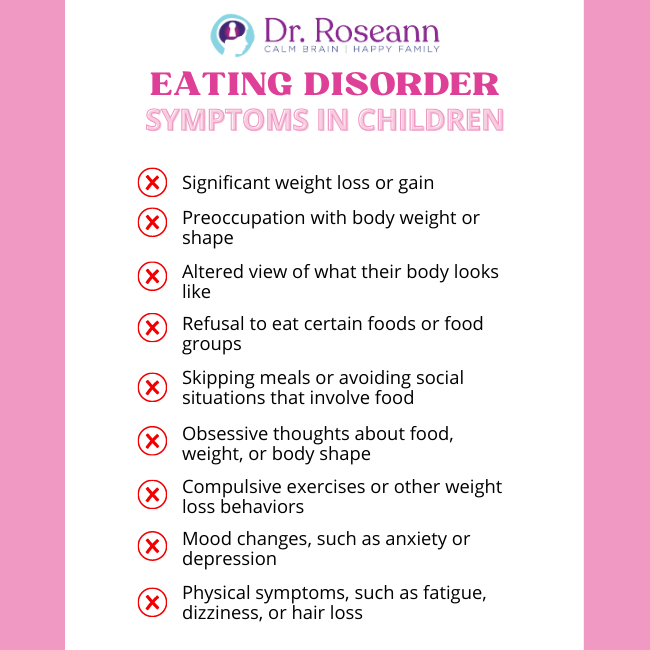
- Significant weight loss or gain
- Preoccupation with body weight or shape
- Altered view of what their body looks like
- Refusal to eat certain foods or food groups
- Skipping meals or avoiding social situations that involve food
- Obsessive thoughts about food, weight, or body shape
- Compulsive exercises or other weight loss behaviors
- Mood changes, such as anxiety or depression
- Physical symptoms, such as fatigue, dizziness, or hair loss
The Connection Between OCD, PANS/PANDAS, and Eating Disorders
PANS/PANDAS is known for causing sudden and intense anxiety, obsessions, and compulsions, which can be alarming for parents and often mistaken for a mental health issue.
While not all children with PANS/PANDAS have OCD, many children with OCD have PANS/PANDAS.
Determining whether a child has PANS/PANDAS or OCD can be challenging because of a lack of knowledgeable providers.
Restrictive eating is a common issue for those with PANS, making it difficult to ensure proper nutrition until the root causes are addressed. This behavior is often rooted in obsessional fears that require behavioral treatment.
PANS/PANDAS can cause restrictive eating due to stomach or throat pain, difficulty swallowing, sensory hypersensitivity, altered taste or smell perception, decreased appetite, obsessional fears, and body image distortions. For those with OCD and PANS, restrictive eating or eating disorders, may result due to obsessional thinking or rituals.
Hannah’s Story
The connection between OCD and eating disorders is also described in Hannah's story. Hannah was a teenager who always displayed signs of perfectionism. She was excessively concerned about her appearance, even as a five-year-old.
When she hit puberty, she was diagnosed with an eating disorder. But we later discovered that she had many ritualistic behaviors around her food. If the rituals weren't performed, she wouldn't eat. Nobody knew this, as it was going on internally. It was only uncovered after many years.
She spent years in and out of treatment places for her eating disorder. She initially worked with a therapist and then had to go inpatient more than once. Somehow, her parents figured out it was OCD. She finally got support for OCD. She had to go to a facility because it had gone on for so long. She went inpatient for three months to work on her OCD.
Hanna's story shows the link between OCD and eating disorders. It’s not always easy to discern whether somebody with an eating disorder has OCD, but using appropriate intake tools, such as the CY-BCOS, to rule out OCD is a good idea.
Here's a deeper take on the relationship between OCD and eating disorders:
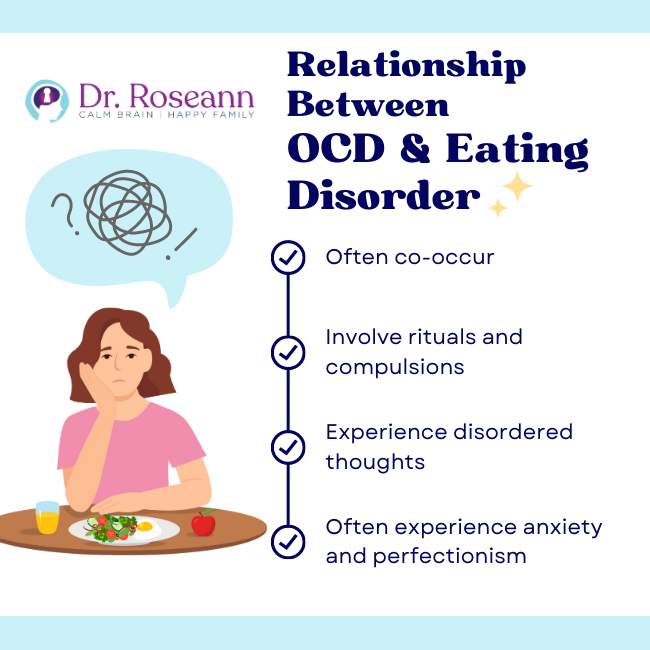
1. Comorbidity
Studies consistently show a high comorbidity rate between OCD and eating disorders (Yilmaz, 2019). Put simply, people with OCD are at a greater risk of developing an eating disorder compared to those who don't have OCD.
2. Obsessive-Compulsive Features in Eating Disorders
Some researchers have proposed that eating disorders may involve obsessive-compulsive features, such as preoccupation with food and eating rituals (Bastiani et al., 1996). These features may be similar to those seen in OCD.
Examples of rituals or compulsions around food and eating are only eating certain foods or in specific ways and engaging in excessive exercise or other behaviors to compensate for food intake.
3. OCD Symptoms in Eating Disorders
Other studies have found that individuals with eating disorders may also experience symptoms of OCD, such as intrusive thoughts and compulsive behaviors (Matsunaga et al., 1999). These thoughts may revolve around food, weight, or body shape, leading to anxiety disorders and distress. In addition, such thoughts may contribute to developing disordered eating patterns, such as restrictive eating or binge eating.
4. Common Underlying Factors
Some factors may contribute to OCD and eating disorders, such as anxiety and perfectionism. People with OCD often have high levels of perfectionism and a need for control, which may contribute to developing eating disorders.
The desire to control one's food intake or body weight may lead to restrictive eating or other disordered eating patterns. OCD and eating disorders are associated with high levels of anxiety and depression, which may contribute to the development of either disorder or the comorbidity between the two.
Similarities Between OCD and Eating Disorders
While OCD and eating disorders share similar symptoms, they are severe mental health conditions with unique characteristics. As discussed previously, anxiety, perfectionism, and intrusive thoughts and behaviors are commonalities between these two disorders.
OCD and eating disorders are associated with high anxiety levels, perfectionism and a need for control, and a preoccupation with intrusive thoughts or behaviors that can interfere with daily life. Furthermore, those with OCD are more likely to have an eating disorder than those without OCD.
Differences Between OCD and Eating Disorders
As two different conditions, some of the distinct differences between OCD and eating disorders are the following:
1. The focus of preoccupation
In OCD, the preoccupation is typically on intrusive, obsessive thoughts or fears that can lead to compulsive behaviors. In eating disorders, the preoccupation is focused on food and it’s impact on one’s weight. As a result, patients suffer from the fear of weight gain or poor body shape.
2. Types of Compulsions
In OCD, compulsions often involve repetitive actions or mental rituals to reduce anxiety or prevent harm. Those compulsions center around preventing feats from happening.
In eating disorders, compulsions may involve restrictive eating, binge eating, or purging behaviors. There is a compulsive need to control food to prevent weight gain.
3. Impact on Physical Health
While OCD can undoubtedly impact an individual's quality of life, it generally does not have as significant an impact on physical health as eating disorders, which can lead to malnutrition, dehydration, and other serious health complications. Eating disorders have a high mortality rate in cases where food restriction affects cardiac health.
Both disorders involve high internal stress that impacts the body in several ways, including physical tension, sleep, problems, pain, and gastrointestinal difficulties.
4. Treatment Approaches
While OCD and eating disorders can be effectively treated with therapy, the specific treatment approaches may differ. For example, Exposure and Response Prevention (ERP) therapy is a standard treatment for OCD, while Cognitive Behavioral Therapy (CBT) and family-based therapy are often used to treat eating disorders.
Both therapies can benefit from integrative care and appropriate nutritional therapies.
Treatment Options for OCD and Eating Disorders
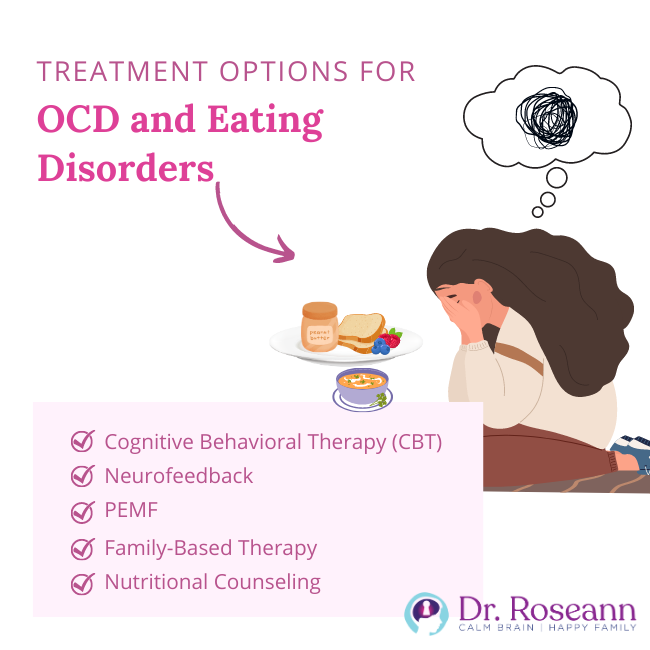
Treatment plans for OCD and eating disorders can vary depending on the severity of symptoms and the individual's unique needs. However, here are some standard treatment options for each condition:
1. Cognitive Behavioral Therapy (CBT)
The preferred and most effective treatment for OCD is a combined Cognitive-Behavioral Therapy with exposure. A therapy called, Exposure and Response Prevention (ERP) therapy.
ERP is widely considered the gold standard in OCD therapy and involves a combination of CBT with exposure therapy. Exposure therapy involves gradually exposing individuals to feared situations or objects while preventing them from engaging in compulsive behaviors. In ERP, parents and children are taught much about the brain and supported in coping with these stressful exposures.
CBT therapy is also used to treat eating disorders. It can help individuals identify and change negative thoughts and behaviors related to food and body image.
2. Neurofeedback
Neurofeedback is a therapy that employs sensors to monitor an individual's brainwaves and provide real-time feedback regarding their brain's functioning. One is giving feedback to change dysregulated brain waves to a healthy combination of brain waves.
Neurofeedback for individuals with OCD can assist them in mastering the regulation of their brain activity, which calms intrusive thoughts, stress levels, and agitation. That takes the OCD brain out of a fight, flight or freeze state, and only then can a child think or take action. No learning can occur without a regulated, calm brain.
3. PEMF
Pulsed Electromagnetic Field Therapy (PEMF) is a therapeutic device involving electromagnetic fields to enhance cellular functioning and promote recovery in the body. It calms the CNS and supports how the cells work and communicate. It also improves detoxification, a major factor in many mental health issues with genetic mutations such as MTHFR on the rise. PEMF can benefit children and teens with eating disorders and OCD as supplementary therapy.
CALM PEMF™ is a portable PEMF device that allows individuals with mental health disorders to regulate their bodies wherever they go. Dr. Roseann has created custom protocols for this FDA-approved device that addresses PANS/PANDAS, OCD, anxiety, and other clinical symptoms.
4. Family-Based Therapy
When somebody has an eating disorder, it affects the whole family. Family-based therapy (FBT) often treats eating disorders in children and adolescents.
This therapy involves the family in the treatment process and aims to help them support the individual in making healthy changes. It is also a helpful way to treat OCD without medications. Family therapy should always address ways not to accommodate OCD. That means learning how to manage avoidant or reassurance behaviors.
5. Nutritional Counseling
Nutritional counseling is always part of a care plan for individuals with eating disorders to develop a healthy relationship with food and establish regular eating patterns. Magnesium supplementation will also greatly help because it calms the nervous system and the body’s depleted nutrients.
Returning to Hannah's story, the right treatment plans were crucial to her recovery. When Hannah got to me, we addressed some underlying issues around her OCD while calming her nervous system with PEMF. We also did neurofeedback and used Exposure and Response Prevention to address her lack of coping skills
Her parents were super grateful but very frustrated about how they had used a lot of resources and gone to many mental health professionals. Yet, it still took years for her to be appropriately identified. It isn't the first time I've had somebody be misdiagnosed with an eating disorder when it was restrictive eating due to OCD.
In our center in our BrainBehaviorReset™ Program, we remotely work with people worldwide using coaching, neurofeedback, PEMF, and biofeedback to treat OCD. We teach families how OCD affects the brain and give children and families the tools to “talk back to OCD” and gain control of their triggers and anxiety.
We strive to support families dealing with the everyday challenges of childhood and adolescence, including but not limited to OCD, PANS/PANDAS, Lyme Disease, ADHD, anxiety, autism, executive functioning, learning disabilities, dyslexia, and mood and behavior dysregulation. Explore our case studies to see how our approach has made a difference for other families.
Searching for natural and effective ways to support your child or teenager struggling with OCD, anxiety, or behavior? Our solution matcher quiz can help you determine the exact next step for your family to take. Try it today to see how we can help you and your loved ones.
Citations
Bastiani, A. M., Altemus, M., Pigott, T. A., Rubenstein, C., Weltzin, T. E., & Kaye, W. H. (1996). Comparison of Obsessions and Compulsions in Patients with Anorexia Nervosa and Obsessive Compulsive Disorder. Biological Psychiatry, 39(11), 966–969. https://doi.org/10.1016/0006-3223(95)00306-1
Matsunaga, H., Kiriike, N., Miyata, A., Iwasaki, Y., Matsui, T., Fujimoto, K., Kasai, S., Kaye, W. H., & Kaye, W. H. (1999). Prevalence and symptomatology of comorbid obsessive-compulsive disorder among bulimic patients. Psychiatry and Clinical Neurosciences, 53(6), 661–666. https://doi.org/10.1046/j.1440-1819.1999.00622.x
Yilmaz, Z. (2019). A Cross-disorder Genome-wide Association Study of Anorexia Nervosa and Obsessive-Compulsive Disorder. European Neuropsychopharmacology, 29, S978. https://doi.org/10.1016/j.euroneuro.2017.08.350
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.