
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!
GUIDE
OCD, or Obsessive Compulsive Disorder, affects millions of children and young adults worldwide and is considered one of the most treatment-resistant mental health conditions. When a child or teen has OCD, the brain gets stuck in a loop of repetitive thoughts or behaviors.
Compulsions and obsessions get worse for children and teens when they try to get rid of distressful thoughts through behaviors and rituals. It can then become a behavioral habit that is very difficult to break, even with the help of traditional talk therapy or medication. It's important to address the OCD symptoms early and get the right treatment. There is hope! The best treatment for OCD is Exposure Response Prevention Therapy (ERP) combined with tools that help the brain the self-regulate. This OCD treatment guide can help.
TABLE OF CONTENTS
OCD, or Obsessive Compulsive Disorder, is a pattern of unwanted or intrusive thoughts and fears (obsessions) that lead the person to act out behaviors (compulsions), so much so that they can interfere with day-to-day activities. OCD thoughts and behaviors can look different for each person experiencing them.
OCD is different from anxiety because it involves intrusive thoughts, compulsions, and rituals. Anxiety tends to be rooted in a real issue, whereas OCD often involves a fear that may be illogical or is identified as a thought not representing the sufferer's true values. The uncomfortable feelings OCD produces are so real that the person feels compelled to perform an action to gain some relief from their distress. As a result of their differences, these two clinical conditions require very different treatments.
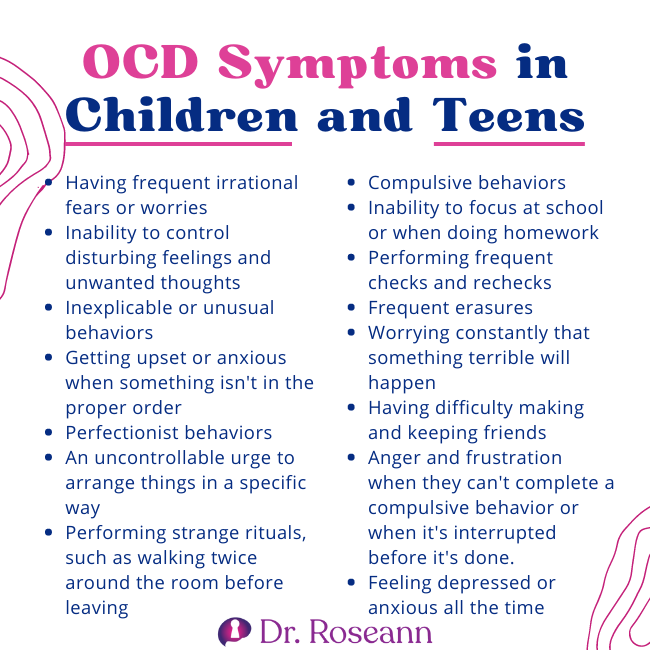
An OCD child or teen's brain is hijacked by intrusive thoughts and compulsive behaviors, making their daily lives very difficult. The presence of intrusive thoughts and compulsions makes it difficult for these kids to connect, focus, and do even simple tasks because the brain is constantly in a state of fear.
People struggling with OCD can appear highly functional. Their thoughts and compulsions can wax and wane with varying intensity. It's possible for kids to seem like they are doing well in school, but they may be struggling internally with obsessions and urges to complete compulsions. The stress of the hijacked brain and constant inner chatter may become too much for them.
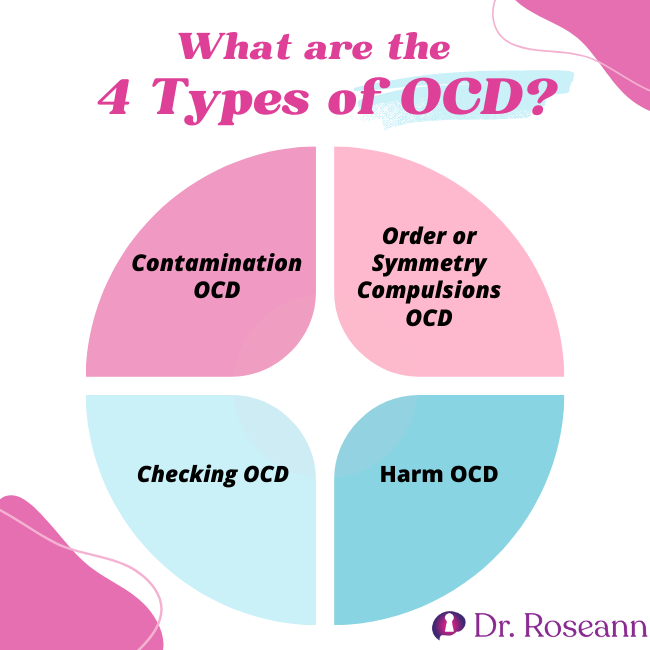
OCD comes in many different types. These are:
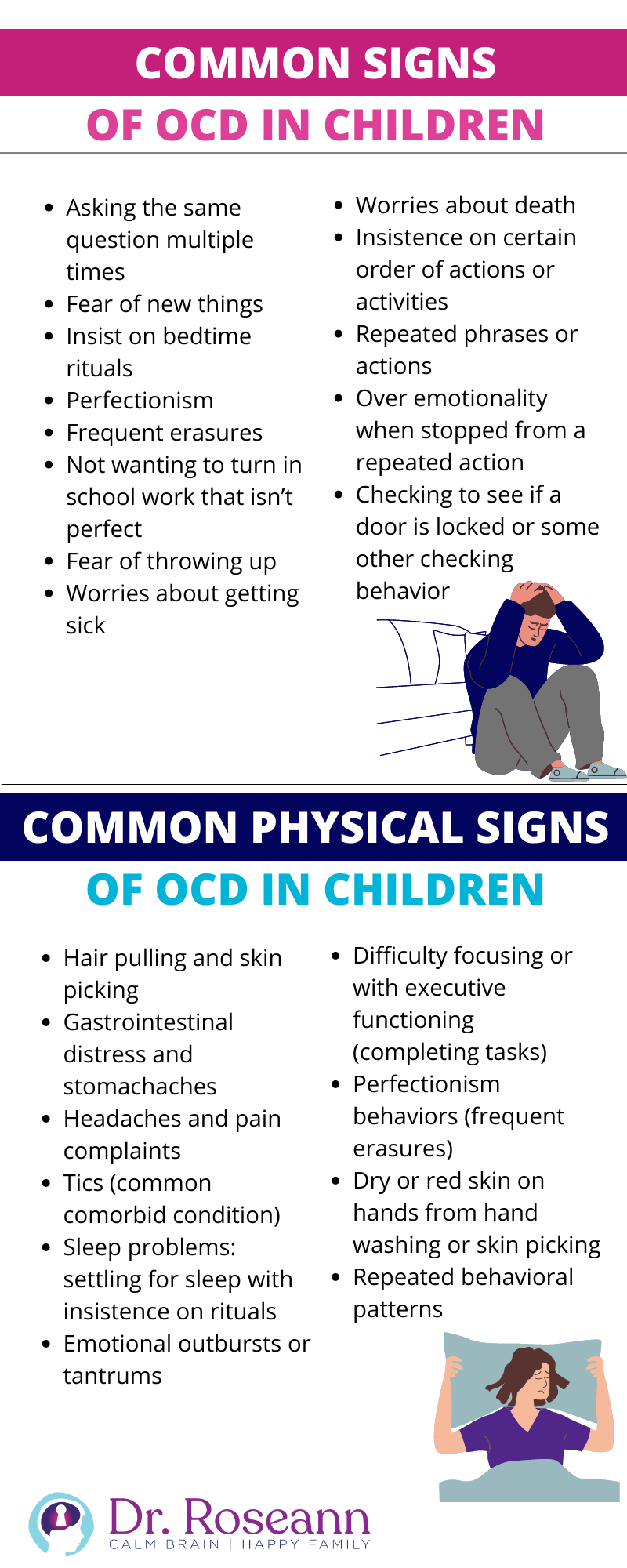
This OCD type consists of the compulsion to check, but the obsessive fear might be to prevent harm. Checking more than appropriate for the situation and not being able to walk away without checking are common symptoms. Among kids and teens these are the most common obsessive worries and compulsions they experience:
The checking process is usually repeated multiple times, sometimes hundreds of times, and can take up to an hour or more. The person that is obsessively checking can sometimes understand that it is unnecessary to keep checking, but the feeling that the OCD creates can be so intense that the person continues the checking behavior. The checking, in turn, continues to feed the negative reinforcement cycle of OCD.
This type of OCD can pertain to the obsessional fear of being dirty, or the fear of being contaminated by touching certain objects or substances. Contamination thoughts can focus on areas such as sticky residues, germs, or bodily fluids. Fears can be focused around harm coming to oneself or fear that harm might come to another person. Compulsions can include avoidance of objects, substances, or places. They can also include excessive washing of self, objects, or demanding that others clean. Obsessive worries and compulsions related to contamination among kids include:

Children with OCD often clean several times, following a ritual of repeated hand washing and body washing. The trick is that the OCD will never let them feel “clean.” The opposite is true for kids without OCD, who will wash only once or twice until they see that everything is clean (and may even need reminders to do that). It is also possible for children and teens with OCD who had contamination fears in the past to entirely avoid places, engagements, people, and objects.
Mental Contamination
Mental contamination is a more recent area that researchers are just starting to understand. Feelings of mental contamination may happen when a child or teen feels badly treated, either physically, mentally, or through critical or verbally abusive remarks, such that they are made to feel like dirt. This creates a feeling of internal uncleanliness.
A distinctive feature of mental contamination is that the source is almost always human, unlike contact contamination, which is caused by physical contact with inanimate objects. As a response, the child or teen will engage in repetitive and compulsive attempts to wash the dirt away by showering and washing, similar to traditional contamination OCD.
Symmetry and orderliness refer to the compulsion to have everything lined up symmetrically perfect. Kids and teens who have this obsessive fear experience discomfort and fear that harm might come to themself or somebody else because things aren't set up just right. Compulsive behaviors can get stuck on making sure things are even or “just right’ from the perspective of the child or teen.
Those affected will spend a lot of time getting the symmetry correct. The time-consuming checking can result in them being extremely late for school or personal engagements. They may become mentally and/or physically drained if these compulsions take a considerable amount of time. They may even avoid social contact just to prevent symmetry and order from being disrupted. This can have a negative impact on their social interactions and relationships.
This term is often used to describe all obsessional intrusive thoughts. In the context of OCD, a rumination is a train of prolonged thinking about a question or theme that is undirected and unproductive. Rumination is an OCD mental compulsion.
Unlike obsessional thoughts, ruminations are not objectionable and are indulged rather than resisted. Many ruminations dwell in religious, philosophical, or metaphysical topics such as the origins of the universe, life, and death. Kids and teens with rumination OCD appear to be deeply pre-occupied, very thoughtful, and detached.
OCD thoughts are obsessional thoughts that are intrusive, repetitive, and disturbing to the person experiencing them. Intrusive thoughts are not voluntarily produced, and they cause the sufferer extreme distress. They can give the person feelings of disgust or shame. The thoughts can be horrific or repugnant in nature. These thoughts do not represent who the person or or who the person wants to be.
While children and kids with this OCD type are capable of having such thoughts, they do not want to act on them. Furthermore, most find these thoughts nauseating and will even go to great lengths to avoid them from taking place, engaging in compulsions. Some examples are:
Hoarding is a type of OCD that refers to the inability to discard useless or worn-out possessions. Hoarding disorder was reclassified in the 2013 publication of DSM-5 as a condition in its own right. However, it does become somewhat complicated because some people will hoard for very specific obsessive worries or fears, and should still be diagnosed as OCD, rather than a hoarding disorder.

Early onset obsessive-compulsive disorder is one of the more common mental illnesses in children and adolescents with a prevalence of 1% to 30%. OCD usually begins in adolescence or young adulthood and is seen in as many as 1 in 200 children and teens.
OCD affects as much as 2% of the world's population. This disorder is often debilitating, and up to 20-40% of cases don't respond to traditional drugs or behavioral treatments (Brown University 2021).
Obsession Symptoms:
Obsession refers to repeated thoughts, urges, or mental images that cause anxiety. Here are some of its symptoms:
Compulsion Symptoms:
Compulsions are repetitive behaviors that children and teens with OCD feel the urge to do in response to an obsessive thought. Symptoms include:
Through the clinical interview process, OCD is diagnosed by a mental health professional. During intake, the clinician is trained to assess whether obsessive or compulsive behaviors are present and determines their impact on that child’s or teen’s life and functioning.
For diagnosis, these behaviors have to have a significant impact on daily functioning, occupy a lot of time, typically more than one hour per day, and cause distress. No specific psychological or laboratory OCD test exists, which often causes frustration.
A healthcare provider uses criteria explained in the Diagnostic and Statistical Manual of Mental Disorders, 5TH edition ( DSM-V) which states:
Typically, OCD starts with anxiety such that one engages in a behavior (intrusive thoughts or compulsive behaviors) in order to avoid negative outcomes. It inadvertently reinforces that behavior, making it more likely to occur.
The cause of OCD is dysregulation of brainwave activity in specific brain regions. The brain regions involved in processing emotional information, stress regulation, and switching gears are highly affected by OCD.
When you look at the brain functioning of someone with OCD, the region that regulates how one perceives stress is overactive. Their neural networks are stuck in a continual looping of inner chatter.
When their central nervous system is hyper-stress activated, they are sensitive to seemingly benign stimuli and live in a constant state of activation of the flight, fight, or freeze response. The overactive brain that can’t shut off is something that every person with OCD experiences and it’s because of the overactive brainwave activity.

PANS (Pediatric Acute-onset Neuropsychiatric Disorder) and PANDAS (Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus) can result in a sudden, rapid onset of obsessive-compulsive thoughts, behaviors, and rituals in children who are infected with a virus, such as from Lyme disease, Streptococcus pyogenes or Group A Strep.
The National Institute of Mental Health (NIMH) has found that some cross-reactive antibodies target the brain, which causes OCD, tics, and other neuropsychiatric symptoms of PANS/PANDAS. A child with PANDAS or PANS may experience severe OCD symptoms, along with cognitive and motor changes. Such a condition is referred to as Acute OCD.
Signs of Acute OCD:
A high percentage of people with autism also suffer from OCD. A Danish study of more than 850,000 people found that people with autism are twice as likely to have OCD, and people with OCD are four times as likely to also have autism.
In the same study, a genetic link was found between OCD and autism. A parent with OCD has a higher risk of having an autistic child. OCD and autism share the same reliance on repetitive behaviors to calm anxiety, suggesting a genetic overlap.
In children with Autism, stimming behaviors (such as hand flapping) are displayed and create a calming effect. Children struggling with OCD rituals and compulsions are also seeking a short term calming response to significant fears. In contrast, children with OCD do not always have social issues or communication problems, which distinguishes them from children with autism.
OCD can be treated with a variety of traditional and holistic therapies. There are some people who benefit from medication, and there are others who do not. Cognitive Behavioral Therapy (CBT) and Exposure and Response Prevention Therapy (E/RP) have consistently proven to be effective treatments for OCD.
Besides Neurofeedback and Biofeedback, and EFT Tapping can also help align the nervous system. It is necessary to regulate the Central Nervous System (CNS) before a person can fully engage in clinical therapy.
CBT is a type of psychotherapy that uses cognitive strategies to treat mental health issues at a conscious level. The concept of cognitive behavioral therapy emphasizes that how an individual perceives a situation is more related to their reaction than the situation itself, so working through those misperceptions can bring relief.
The goal of CBT is to reframe negative thinking patterns into positive ones using talk and behavioral therapy. According to research, CBT reduces symptoms more effectively than medication (59.9% vs. 33.4%) and is considered the first line of treatment for OCD.
Exposure and Response Prevention therapy involves gradually and systematically exposing a person to their fears, while assisting clients in managing their fear response. Here, therapists create a safe environment for an individual to learn to tolerate their fears, which reduces compulsive behaviors and the avoidance of dreaded situations thereby easing anxiety and panic attacks. A therapist can expose a client to their fears in several ways, including:
Imaginal Exposure
During this type of exposure, the client mentally imagines the fear or situation in question and confronts it. For example, a child with a fear of germs may be asked to visualize being near someone sick.
In Vivo Exposure
Children and teens are exposed to real-life objects and situations through this type of exposure. For example, a child or teen with a fear of germs may be asked to pick up a dirty ball.
Virtual Exposure
Through the use of technology, this type of fabricated exposure combines elements of both imaginal and in vivo exposure so that a person is placed in situations that appear real but aren’t. For example, someone who has a fear of germs might participate in a virtual simulation of touching an object that someone just coughed on.

In neurofeedback, brain wave functions are directly changed and the brain is able to self-regulate. Getting the brain to self-regulate reduces negative behaviors and symptoms.
With neurofeedback, a child with PANS/PANDAS and obsessive-compulsive behavior can improve their mental health irregularities. By adding neurofeedback, anxiety in daily life declines gradually, allowing parents to receive therapeutic coaching to support their children at home.
It is not uncommon for children with PANS/PANDAS and OCD to experience anxiety or even trauma as a result of their medical condition. The EFT technique unlocks those unwanted feelings from our subconscious in a very effective way, thereby reducing anxiety, irritation, anger, and a wide range of feelings. Emotional stress can hinder the body's ability to heal. Therapy tools like the Emotional Freedom Technique (EFT Tapping) aim to release negative emotions and beliefs that interfere with a person's emotional well-being. Using EFT can help manage pain, OCD, anxiety, anger, and other psychiatric issues that cause stress among children, making it hard for their bodies to heal.
When it comes to relieving symptoms of OCD, magnesium can play a vital role in regulating neurotransmitters that affect mental health. By reducing the release of excitatory neurotransmitters, which can cause intrusive thoughts and anxiety, magnesium helps create a more relaxed state of mind. Additionally, magnesium can increase the production of serotonin, a neurotransmitter that promotes feelings of well-being and happiness.
People with OCD tend to have an excess of excitatory neurotransmitters that can cause their brain to get stuck in a repetitive cycle of intrusive thoughts. By calming down these neurotransmitters with magnesium, individuals with OCD can experience relief from their symptoms and gain enough mental space to effectively utilize the tools taught in Exposure and Response Prevention (ERP) therapy.
Having a child with OCD can be challenging for parents because children don’t outgrow OCD. Instead, they need to learn how to overcome it through therapy and treatments.
The goal of treatment is to help a person manage obsessions. OCD can be extremely treatment resistant because it is often missed and misdiagnosed. When not addressed, the OCD brain forms a habit rooted in fear avoidant behaviors. OCD is all about having rituals that prevent “the bad thing” from happening.
OCD is very “sneaky” and family members, caregivers, and even teachers often inadvertently reinforce the behaviors because they don’t know that what they are seeing is OCD. By accommodating the behaviors, it is more likely that the OCD not only will continue but actually worsens. This is called a negative reinforcement cycle.
There are things parents can do and it is critical in getting the right diagnosis and treatment in order to dismantle OCD behaviors.
Early intervention is the best course of action. The onset of OCD usually occurs between 8 and 12 years of age but can be experienced as early as 4 years old. Parents should never ignore their child’s symptoms. When OCD habits occur for a long period of time, they become increasingly ingrained, which makes them harder to break.
Obsessive and compulsive behavior can develop in children as a means of coping with stress. When OCD behaviors are broken before they become ingrained, their severity can be lessened and, in some cases, it can even stop the disease's progression.


To support a child with OCD, parents need to receive psychoeducation and participate in ERP therapy sessions. Children need their parents' help in tolerating their obsessions and compulsions instead of suppressing them. This way, obsessions and compulsions are reduced, if not extinguished.
Consult with a therapist who is an expert in neurofeedback and ERP to initiate the natural treatment of OCD. It is important to do so before the obsessions and compulsions have become more ingrained and debilitating.

iocdf.org/about-ocd/how-is-ocd-diagnosed/
ocduk.org/omayoclinic.org/diseases-condition/obsessive-compulsive-disorder/
https://drroseann.com/category/ocd/page/2/
Brown University. (2021, December 9). Researchers identify brain signals associated with OCD symptoms, paving the way for adaptive treatment. ScienceDaily. Retrieved November 4, 2022, from www.sciencedaily.com/releases/2021/12/211209124247.htm
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Always remember… “Calm Brain, Happy Family™”
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”
She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2022

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
