Estimated reading time: 6 minutes
Obsessive Compulsive Disorder (OCD) can turn life upside down for young kids and their families.
When 11-year-old Iris first came to me, OCD was running the show—her days were filled with intrusive thoughts and exhausting rituals. But through my BrainBehaviorReset™ program, that story began to change.
Using neurofeedback, PEMF, dietary support, ERP, and other calm-brain tools, we didn’t just mask the symptoms—we got to the root of her struggles. Today, Iris has a powerful toolkit of strategies that help her feel calm, confident, and back in charge of her own mind.
Early Warning Signs of OCD in Kids
If you’re starting to notice changes in your child that feel more intense than typical worries, you’re not alone. Many parents miss the early signs of OCD because they can look a lot like common childhood anxiety.
Iris was just seven when her mom started noticing something wasn’t quite right. What began as harmless questions about school routines quickly turned into constant, panicked reassurance-seeking:
- “Are you sure I didn’t forget anything?”
- “What if I get sick at school?”
- “Can you double check my bag again?”
These weren’t just innocent questions. Iris would ask the same thing dozens of times and melt down if she didn’t get the answer she needed, exactly the way she needed it. Her brain was stuck in a loop.
Key early signs of OCD in kids can include:
- Repetitive questions and reassurance-seeking
- Rituals or habits they feel they must do “just right”
- Fear that something bad will happen if they don’t act on a thought
- Emotional outbursts when routines are disrupted
| Typical Childhood Worry | Early Signs of OCD |
|---|---|
| Worries come and go, especially around big changes | Worries are persistent, irrational, and often revolve around specific themes (e.g., germs, harm) |
| Child may need a little reassurance now and then | Child repeatedly asks for reassurance but never seems satisfied |
| Occasional rituals or routines (e.g., bedtime habits) | Rigid, distressing rituals that must be done “just right” to prevent something bad |
| Worry doesn’t usually stop daily activities | Anxiety or compulsions interfere with school, sleep, or family time |
| Fear fades after being comforted | Fear gets stronger over time, even after reassurance |
| Can be distracted by play or fun activities | Has trouble enjoying things due to obsessive thoughts or compulsive behaviors |
Why Does OCD Cause So Many Meltdowns in Kids?
By age 8, Iris’s meltdowns were full-blown. Anything that felt out of her control could set her off: packing the wrong lunch, sitting in a different seat at dinner, a spelling test.
The emotional dysregulation wasn’t about defiance. It was her nervous system stuck in overdrive, desperately trying to manage intrusive thoughts and fears.
Behavior is communication. In Iris’s case, her outbursts were her brain’s way of saying, “I can’t handle this overwhelm.”
Common OCD-related triggers for emotional meltdowns:
- Sudden changes in routine
- Unmet perfectionistic standards
- Transitions or uncertainty
- Uncomfortable physical sensations (e.g., sticky hands)
How Do I Help My Child When OCD Makes School Feel Impossible?
OCD was taking a toll on Iris’s school life. She began refusing to go altogether. Her mornings were filled with tears, nausea, and clinging.
School refusal is a huge red flag that your child’s nervous system is too overwhelmed to cope. For kids with OCD, it’s often not about academics, it’s about the fear of being triggered in a place they can’t control.
Signs your child’s school refusal could be OCD-related:
- Fear of germs, throwing up, or making mistakes in front of others
- Compulsions that interfere with getting ready on time
- Needing constant reassurance about their day
- Feeling unsafe when away from home
Treatments that Help Kids Recover from OCD
When Iris’s family found us, they were exhausted and scared. They had tried traditional therapy, but it wasn’t working. They needed more than coping tools—they needed to calm her brain.
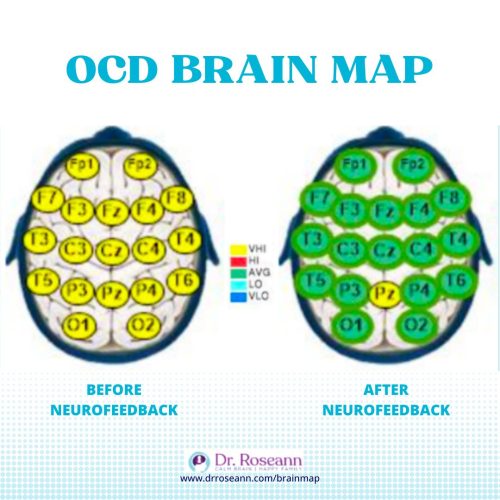
We started with a QEEG brain map, which confirmed what we suspected: Iris’s brain was overstimulated and stuck in high alert.
Through neurofeedback and brain-based OCD treatment, we began to regulate her brain and gently reduce the OCD loop.
Effective, science-backed tools for OCD in kids include:
- Neurofeedback: Trains the brain to self-regulate
- Cognitive Behavioral Therapy (CBT): Especially Exposure and Response Prevention (ERP)
- Nutritional and lifestyle support to reduce inflammation and stress
Can a Child Really Recover from OCD?
Yes, kids can recover. OCD isn’t a life sentence. With the right support, the brain can rewire, and your child can reclaim their joy.
Today, Iris is 11. She goes to school without issue. She doesn’t obsess over every detail or melt down when things change. She still has a sensitive nature, but her OCD isn’t running the show.
What OCD recovery looks like in real life:
- More flexible thinking
- Reduced rituals and compulsions
- Better emotional regulation
- Greater confidence and independence
If you’re wondering whether your child’s behaviors might be signs of OCD, take our free quiz:
👉 Take the OCD Brain Quiz
It takes less than 2 minutes and can help you understand what’s going on in your child’s brain.
Parent Action Steps
FAQs
How do I know if it’s OCD or anxiety?
OCD and anxiety often overlap, but OCD includes compulsions (repeated behaviors or mental rituals) meant to neutralize scary thoughts.
What age does OCD start in kids?
OCD can start as early as preschool, but most often appears between ages 7 and 12.
Can OCD go away without treatment?
OCD rarely resolves on its own. Early intervention is key to long-term recovery.
Does my child need medication?
Not always. Many families see strong results from brain-based therapies like neurofeedback without medication.
Citations:
Abramowitz, J. S., Taylor, S., & McKay, D. (2009). Obsessive-compulsive disorder. The Lancet, 374(9688), 491–499. https://doi.org/10.1016/S0140-6736(09)60240-3
Piacentini, J., Bergman, R. L., Keller, M. L., & McCracken, J. T. (2003). Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology, 13(Supplement 1), S61–S69. https://doi.org/10.1089/104454603322126359
Storch, E. A., Merlo, L. J., Larson, M. J., Geffken, G. R., Lehmkuhl, H. D., Jacob, M. L., … & Goodman, W. K. (2008). Clinical features and treatment response in children and adolescents with obsessive-compulsive disorder. CNS Spectrums, 13(11), 913–922. https://doi.org/10.1017/S1092852900016888
Dr. Roseann Capanna-Hodge is a licensed mental health expert that is frequently cited in the media:
- Single Care Controlling the uncontrollable: Living with OCD during a pandemic
- Holistic Counseling Podcast: Effective Treatments for OCD
- Epidemic Answers: Neurofeedback for ADHD, anxiety, OCD and mood
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!









