Attention Deficit Hyperactivity Disorder (ADHD) is a condition that affects children and adults throughout their lifespan in similar and unique ways. For some people with ADHD, these symptoms may be very internal with “zoning out” or daydreaming behaviors being the most prominent ones affecting school performance, work, or relationships.
Other people with ADHD, including both adults and children, may display more externalizing behaviors such as behavioral or emotional outbursts. With children with ADHD, the triggers to these outbursts may be more apparent, such as sensory overload, fatigue, or frustration, and other times it may be less so.
Rejection-sensitive dysphoria (RSD) is a condition that affects a large percentage of those with ADHD and overlaps with ADHD symptoms. People with RSD are prone to emotional dysregulation with real or perceived criticism or rejection. They experience emotional pain that is hard to bounce back from as a result. The strong emotional reactions can disrupt a child's and their family's life and adults too, as it often leads to friction and upset with others.
Ben was a little boy who already had been in multiple therapies and on multiple medications for his emotional dysregulation for years. His parents came to me exhausted, deflated, and with their blood pressure raising by the minute. They felt like they had tried everything to curb his explosive behaviors and meltdowns but nothing helped. The other kids were afraid to play with him and so were his siblings.
Ben came in with a diagnosis of ADHD and Oppositional Defiant Disorder (ODD), which meant he was impulsive and also combative when asked to do something. His parents tried to be loving and supportive but Ben was quick to lash out and always felt persecuted and criticized. It was that constant battle over being criticized that drove his outbursts. That is RSD. Don't worry we helped Ben love himself and his brain. Read to the end to find out how.
So let's dive into what exactly rejection-sensitive dysphoria is and why haven't you heard of this condition that might explain the behaviors you see in your child or teen.
What is Rejection Sensitive Dysphoria?
Rejection sensitive dysphoria (RSD) is when a person experiences emotional pain after real or perceived criticism or rejection. Individuals who experience RSD react very strongly and in a manner that is disproportionate to the experience.
Although not a clinical disorder, rejection-sensitive dysphoria can be severe enough to disrupt a child's or an adult's life. Their emotional responses are often out of proportion to the actual event trigger and they can be too dysregulated to respond to support. Family members often describe having to “walk on eggshells” around them to avoid their emotional or explosive episodes.
Emotional Regulation and Rejection Sensitive Dysphoria
How one responds to upset, criticism, unexpected changes, and one's stress tolerance are all factors that determine how a person regulates their emotions. For some kids, teens, and adults, managing emotional and behavioral responses are easy because they are cool under pressure.
For others, when minor things happen or plans change, they have big emotions and reactions. They embody, “Making a mountain out of a molehill.” This happens because they feel things so strongly and lack frontal lobe regulatory control to put the breaks on.
Emotional Dysregulation and The Brain
When I see the QEEG Brain Maps of individuals with emotional dysregulation, a clear pattern emerges. They have over-reactivity in the emotional centers of their brain (limbic system), poor frontal lobe control, and low activity in the occipital region. This triple whammy means that their brain feels things more strongly and lacks the ability to both put the brakes on and recover when upset.
The inability to pull back from an emotional upset causes one to get caught in a behavioral loop of over-reactivity to seemingly minor everyday stressors. The problem with emotionally reactive behaviors is that the more it happens, the more likely the subconscious brain is to repeat the pattern.
That is why interventions that we use on our BrainBehaviorReset™ Program that focus on both calming the brain so it reacts less and behavioral support to teach coping skills are imperative. You must reduce the brain's over-sensitivity and at the same time show a child, teen, or adult a healthy way to respond to stress or change.
How Does Rejection Sensitive Dysphoria Relate to Those With ADHD?
Rejection sensitive dysphoria (RSD) is comorbid with ADHD, which means that it occurs at a high rate in individuals with a diagnosis of ADHD.
The brains of individuals with ADHD are more prone to dysregulation and thus their behavior can reflect that. With emotional dysregulation, behaviors such as excitability, rapid, exaggerated mood changes, easily upset or tearfulness, rage, or being quick to anger. A lack of impulse control, cognitive flexibility, and behavioral inhibition are all common to ADHD and manifest in many ways including sensitivity to criticism.
In the case of RSD, a person with ADHD not only lacks behavioral control but may perceive the slightest suggestion as a direct character attack and become emotional as a result. Their impulsive sensitivity can be a barrier in relationships.
Is RSD Common in Those with ADHD?
With the rise in neurodevelopmental disorders and clinical mental health conditions in children in teens, RSD behaviors are also on the rise.
In one 2013 study (Surman et. al) that looked at the emotional regulation in adults with ADHD, they found that difficulties with emotional regulation were more common among those with ADHD compared with non-ADHD adults. The study results noted that 55% of adults with ADHD reported extreme difficulties with emotional regulation.
Poor emotional self-regulation behaviors such as low frustration tolerance, temper outbursts, emotional impulsivity, and mood lability are commonly associated with ADHD.
Is Rejection Sensitive Dysphoria a Symptom of ADHD?
Is it the chicken or the egg is the question most ask when it comes to emotional regulation with those with ADHD and RSD. Is it the lack of impulse control that feeds difficulties with low frustration tolerance and emotional regulation or do RSD symptoms impede one's ability to focus? There isn't an easy answer and each child or adult has a unique set of brain wave patterns and history.
There is no doubt that there is a crossover between the two and they co-occur together. Managing impulsive and dysregulated behaviors can be extremely hard on a person and their family. There is a lot of shame behind this up-and-down behavioral cycle, which only serves to add fuel to the fire.
How Is Rejection Sensitive Dysphoria Different From ADHD?
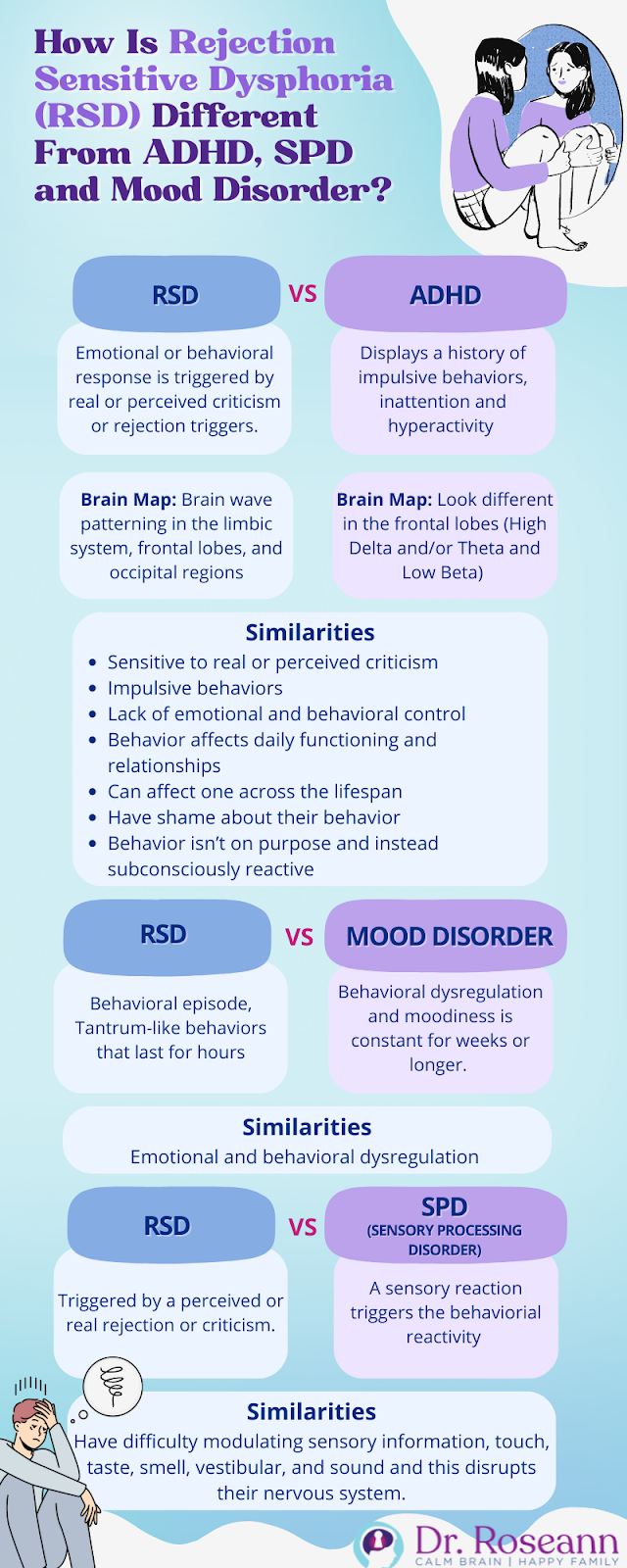
Rejection sensitive dysphoria (RSD) is different from ADHD because it is when someone becomes upset after real or perceived criticism or rejection. When they feel rejected or criticized, it triggers an emotional or behavioral response. While there is quite an overlap between ADHD and RSD because many kids (and adults) with RSD hate to be judged and therefore often feel like they are being criticized.
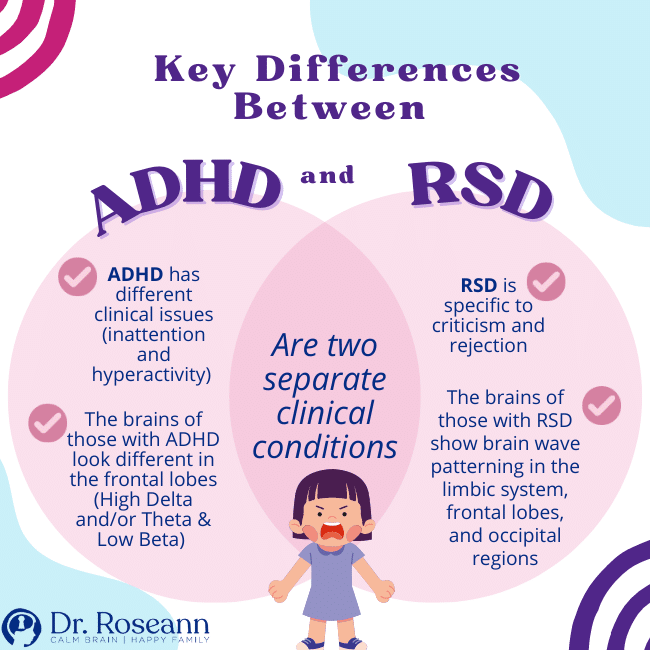
The difference between the two is that ADHD comes with a host of other symptoms, whereas RSD is specific to criticism and rejection. The symptoms of ADHD are distinct and children and adults with ADHD have a history of inattentive, hyperactive, or impulsive behaviors.
Key Differences Between ADHD and RSD:
- Are two separate clinical conditions
- ADHD has different clinical issues (inattention and hyperactivity) and issues
- RSD is specific to criticism and rejection
- The brains of those with ADHD look different in the frontal lobes (High Delta and/or Theta and Low Beta)
- The brains of those with RSD show brain wave patterning in the limbic system, frontal lobes, and occipital regions
How Is Rejection Sensitive Dysphoria Similar to ADHD?
RSD and ADHD are similar in that they can affect both children and adults alike across the developmental lifespan and impact emotional and behavioral regulation.
There is also overlap between RSD and other mental health conditions including, sensory processing disorder (SPD), autism (ASD), social phobia and anxiety, and mood disorders, as these behaviors can be present.
It is important to note that individuals with borderline personality disorder (BPD) are also particularly sensitive to perceived criticism but the trigger often is related to when they don't get what they want or when things do go as planned. Individuals with BPD typically have a parent with BPD and/or trauma history.
Similarities Between ADHD and RSD:
- Sensitive to real or perceived criticism
- Impulsive behaviors
- Lack of emotional and behavioral control
- Behavior affects daily functioning and relationships
- Can affect one across the lifespan
- Have shame about their behavior
- Behavior isn't on purpose and instead subconsciously reactive
Why Haven't I Heard of RSD?
While the behaviors associated with RSD aren't new, understanding how this combination often presents itself together is. Emotional regulation is an important developmental skill and when kids don't learn to self-regulate, that means they need adult intervention to help self-soothe, deal with frustration, manage unexpected or disappointing outcomes, or whatever else life throws their way.
The difference with kids with RSD is that their emotional dysregulation is a direct result of real or perceived criticism. You may be thinking, “Does my kid have RSD?” Well, they certainly might.
Why isn't RSD an Official Diagnosis Yet?
For a disorder or issue to become a formal clinical diagnosis, not only must there be research, a group of mental health professionals must agree that it should be included in the Diagnostic and Statistical Manual (DSM). The DSM is a clinical reference guide that professionals use to make a formal diagnosis and is updated very infrequently.
Definition and Explanation of RSD
Rejection Sensitive Dysphoria (RSD) is a term that defines an extreme emotional sensitivity and pain triggered by the perception that a person has been rejected or criticized by important people in their life. Unlike general sensitivity to rejection, RSD is characterized by intense and overwhelming emotional responses that can seem disproportionate to the situation.
In the context of ADHD, RSD manifests as an acute response to perceived criticism, leading to rapid, intense emotional reactions. This sensitivity often exacerbates the symptoms of ADHD, making emotional regulation even more challenging. The term ‘RSD' itself is a combination of ‘rejection', denoting the trigger for the dysphoria, and ‘dysphoria', meaning a profound state of unease or dissatisfaction. This condition goes beyond mere rejection sensitivity or rejection anxiety disorder, as it typically results in swift and very intense emotional pain.
What Are Signs of RSD or How Can a Person With ADHD Recognize That This May be Going on?
RSD may not be a formal clinical condition yet but the symptoms are real and can be quite disruptive in a person's life at home, school, or work. Symptoms of RSD are triggered by hurt feelings due to feeling criticized, judged, or rejected.
RSD symptoms include:
- Sudden emotional outbursts after real or perceived criticism or rejection
- Emotional overwhelm
- Low frustration tolerance
- Defensiveness
- Sudden mood changes
- Rage or easily angered
- Social withdrawal
- Fear of failure
- Rumination
- Negative self-talk
If you see extreme or explosive reactions to suggestions or mild criticism in someone you care about, then they may have rejection-sensitive dysphoria. Getting them education and support for RSD is important to foster healthy frustration tolerance and coping mechanisms.
How Is Rejection Sensitive Dysphoria Different from a Mood Disorder?
The primary difference between RSD and mood disorders is that RSD has a clear trigger; real or perceived criticism and rejection. Individuals with a mood disorder shift their mood with no clear trigger and a mood episode can last for an extended period.
They are similar in that behavioral episodes can be quite explosive and “tantrum-like” behaviors can last for hours. The difference is that with a mood disorder the moody behaviors persist and the duration of a mood episode must be present for at last two weeks.
So, there can be an up and down in behavioral and emotional dysregulation with both RSD and mood disorder, but with the latter, the moodiness is a constant for weeks or longer.
Causes of RSD
The exact causes of Rejection Sensitive Dysphoria are not fully understood, but it is believed to be a complex interplay of neurobiological, psychological, and environmental factors. Neurologically, it may be linked to the way the brain processes emotions and pain, with some theories suggesting a dysregulation in the brain's neurotransmitter systems, such as dopamine pathways.
Psychologically, individuals with ADHD may have a heightened vulnerability to RSD due to their inherent difficulties with emotional regulation. Environmental factors, including past experiences of rejection or criticism, can also contribute to the development of RSD. Understanding these causes is crucial, as it helps in tailoring more effective treatment and management strategies.
Comorbidities with RSD and ADHD
RSD often co-occurs with ADHD, forming a complex relationship that can complicate diagnosis and treatment. This comorbidity can intensify the challenges faced by individuals, as they struggle with the impulsivity and attention issues of ADHD alongside the intense emotional reactions characteristic of RSD. Additionally, RSD can be comorbid with other conditions such as anxiety disorders, depression, and even bipolar disorder, adding layers of complexity to the clinical picture.
How Is Rejection Sensitive Dysphoria Different from a Sensory Processing Disorder?
Sensory processing issues are common to many clinical conditions such as ADHD, ASD, OCD, and PANS/PANDAS and are also stand-alone issues. Children with sensory processing issues or a Sensory Processing Disorder (SPD) have difficulty modulating sensory information, touch, taste, smell, vestibular, and sound and this disrupts their nervous system.
The nervous system disruption can cause emotional or behavioral reactivity. The difference between RSD and SPD is the triggers are different. With SPD a sensory reaction triggers the behavior, whereas with RSD it is triggered by a perceived or real rejection or criticism.
The behaviors can appear suddenly and with SPD a sensory diet, or treatment for sensory sensitivity, can greatly help to reduce the behaviors. For example, adding in a sensory nervous system regulation activity such as dry brushing or trampolining can help a child be more receptive to food textures.
I recall working with Annabelle who was so sensitive to food textures that she stopped eating, which of course led to an increase in emotionally reactive behaviors (hello, she was running on empty!). After dry brushing and using the backside of a toothbrush on her face before she ate, she gradually was able to eat more and more. The improved nutrition coupled with sensory therapies and strategies virtually eliminated her emotional tantrums.
How Does Emotional Dysregulation Affect One Across the LifeSpan
Kids and adults who have trouble with regulating emotions often struggle with relationships and other functional areas of their lives.
Shaw et. al (2014) examined the long-term impact of emotion dysregulation in those with ADHD. When they surveyed the literature, there were three key findings:
- Emotional dysregulation is common in ADHD throughout the lifespan and is a major contributor to functional impairment.
- Emotional dysregulation may result from dysfunction within a striato-amygdalo-medial prefrontal cortical network, which impacts how one is recognizing and switching attention to emotional stimuli.
- While there are treatments for emotion dysregulation, there needs to be a focus on the associated clinical symptoms to stimulate novel therapeutic approaches.
Are There Ways to Cope with Having RSD?
The first thing to do if you think you or a child has RSD is to get help from a licensed professional. Addressing the misperceptions and low-stress tolerance that are at the core of this disorder is critical in breaking the cycle.
Explosive behaviors aren't tolerated in society and lead to social isolation, constant conflict, and even legal issues. Unchecked rage makes people uncomfortable and even scared, so that means people will likely avoid you.
Understanding the issue and gaining coping skills through the therapeutic process can help an individual regulate their thinking and behavior. Without impulse control, a child or person gets stuck in a constant cycle of emotional activation. So, learning to recognize triggers, pause before you react, and how to walk away are tools that should be taught, practiced, and reinforced.
How Can Loved Ones Cope with a Person Who has ADHD and RSD?
Understanding what rejection sensitive dysphoria, triggers, and strategies to support yourself and the person you love is as important as the person getting the treatment. A person with RSD isn't doing this on purpose but has difficulty putting the brakes on their overreactions. That also means they likely feel ashamed and hopeless about their situation.
Having patience with the therapeutic process and sticking with a plan to build problem-solving and coping skills, while improving family communication can have a powerful effect on the individual and family dealing with RSD.
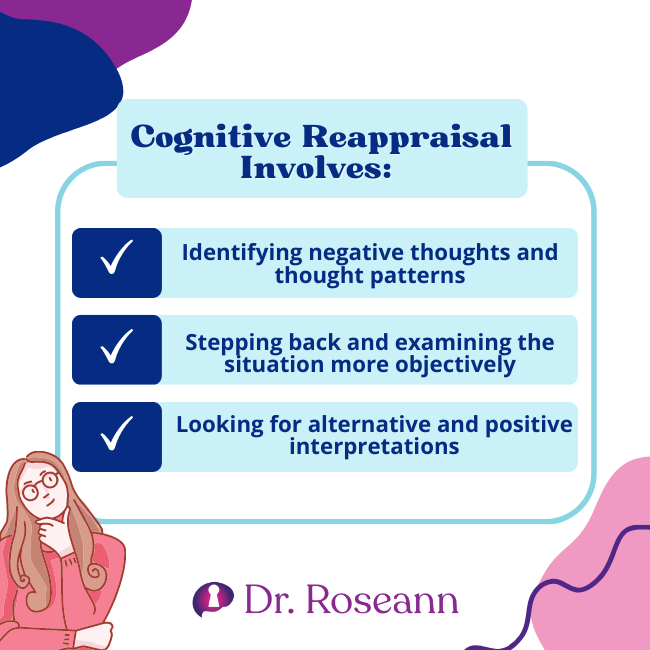
Teaching your child or loved one a strategy called cognitive reappraisal, which involves changing how one thinks about a situation to influence one's emotional response, is important (McRae & Gross, 2020). Because a person with RSD misperceives the situation, thought reframing helps one to manage unwanted thoughts.
Cognitive Reappraisal Involves:
- Identifying negative thoughts and thought patterns
- Stepping back and examining the situation more objectively
- Looking for alternative and positive interpretations
Support and Coping Strategies for Families and Individuals
Dealing with RSD requires a multi-faceted approach. For families and individuals, understanding the condition is the first step. Relationship advice for those dealing with RSD revolves around fostering an environment of understanding, patience, and open communication. It's important to recognize the emotional pain behind the reactions and to approach situations with empathy.
Coping strategies include:
- Educational Support: Learning about RSD and its triggers can help families and individuals anticipate and manage situations better.
- Therapeutic Interventions: Techniques like cognitive-behavioral therapy (CBT) can be effective in helping individuals understand and change their thought patterns.
- Emotional Regulation Skills: Teaching and practicing emotional regulation techniques can be beneficial, especially for those with ADHD and RSD.
- Supportive Environment: Creating a supportive, calm and non-judgmental environment can help reduce feelings of rejection and criticism.
Understanding the nuances of Rejection Sensitive Dysphoria, especially in the context of ADHD, is essential for effective management and support. Recognizing the causes, acknowledging comorbidities, and implementing effective coping strategies can significantly improve the quality of life for those affected by RSD.
How is Rejection Sensitive Dysphoria Treated?
Children with rejection-sensitive dysphoria can be very hard to parent because of their high emotionality. Parents are often perplexed by their behavior and wonder if it is purposeful, which further leads to the breakdown of the parent-child relationship.
Care must be taken to educate parents about RSD and how to build stress tolerance and foster coping skills. Consistent reinforcement of the behaviors you want to shape and ignoring overly reactive responses can also be powerful.
Parent Tips to Manage Emotional Dysregulation in ADHD and/or RSD
Parenting children and teens who are reactive or even emotionally explosive is hard on the child and parent. When every interaction could potentially result in upset on both ends, it affects how you both feel about each other. Parents never think their child will be anything but easy but that often isn't the case.
The good news is that even the most dysregulated children can learn healthy coping skills. It is just going to take shifting what you are doing to shape the behaviors you both want. We guide parents every day in our premier one-to-one program, BrainBehaviorReset™, to cultivate regulated behaviors even when they have clinical diagnoses such as autism, ADHD, PANS/PANDAS, mood disorders, etc.
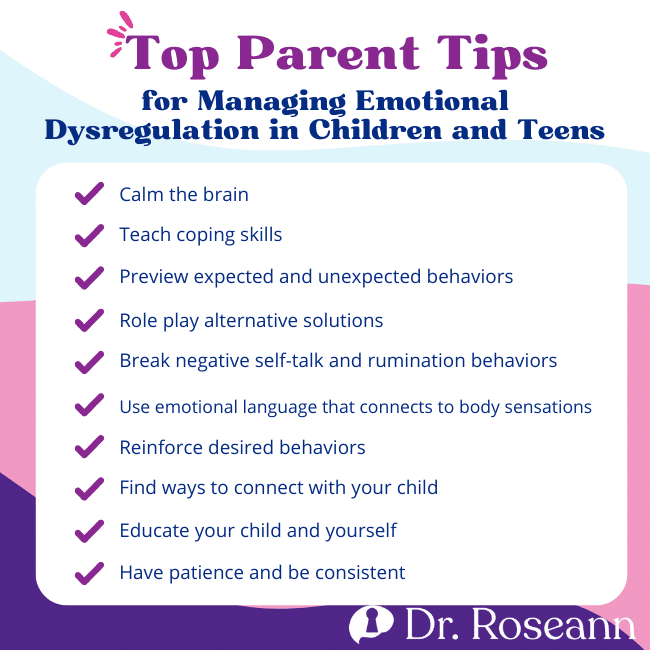
Top Parent Tips for Managing Emotional Dysregulation in Children and Teens
- Calm the brain
- Teach coping skills
- Preview expected and unexpected behaviors
- Role play alternative solutions
- Break negative self-talk and rumination behaviors
- Use emotional language that connects to body sensations
- Reinforce desired behaviors
- Find ways to connect with your child
- Educate your child and yourself
- Have patience and be consistent
Remember Ben? The little boy whom no one would play with because of his emotional and behavioral outbursts and whose parents felt like they had exhausted all options to help him? Well, Ben is a thriving adult now because we calmed his brain with neurofeedback and taught Ben (and his parents) how to cope with frustration and unexpected changes, and stop his negative self-talk.
His brain was too on fire to take a different action and instead, he was caught in a behavioral loop that he couldn't get off until his brain was calm. Only then could Ben use the coping skills that he learned in therapy. It didn't happen overnight but Ben learned to understand his brain and more importantly love himself. When that happened, he was able to connect with other children, and his siblings and have a loving, non-friction, relationship with his parents. And that is why I do what I do… so we can have happy families!
Just remember even if you feel frustrated and hopeless because you have tried a lot with your child or teen, it is all about calming the brain and teaching new skills. Have patience and stick with it and you both will be better for it today and for the days to come.
Parent Action Steps
☐ Observe your child for possible symptoms, such as emotional dysregulation, impulsivity, and inattention.
☐ Consult a mental health professional for a comprehensive evaluation and guidance.
☐ Seek support and education to discover effective strategies for managing your child's condition.
☐ Explore treatment options, such as therapy or neurofeedback, tailored to your child's needs.
☐ Help your child develop coping skills, including cognitive reappraisal, to manage emotions and frustration.
☐ Be patient and consistent in implementing coping strategies and reinforcing desired behaviors.
☐ Stay informed about the latest research and developments to make informed decisions in supporting your child with RSD and ADHD.
☐ Take this ADHD Quiz to know if your child has ADHD or something else.
☐ Try our Solutions Matcher to get personalized treatment for your child.
Citations
Bennett, Shannon & Albano, Anne. (2020). Using exposure with adolescents and youth adults. 10.1016/B978-0-12-815915-6.00013-5.
McRae, K., & Gross, J. J. (2020). Emotion regulation. Emotion (Washington, D.C.), 20(1), 1–9. https://doi.org/10.1037/emo0000703
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. The American journal of psychiatry, 171(3), 276–293. https://doi.org/10.1176/appi.ajp.2013.13070966
Surman, C. B., Biederman, J., Spencer, T., Miller, C. A., McDermott, K. M., & Faraone, S. V. (2013). Understanding deficient emotional self-regulation in adults with attention deficit hyperactivity disorder: a controlled study. Attention deficit and hyperactivity disorders, 5(3), 273–281. https://doi.org/10.1007/s12402-012-0100-8
Dr. Roseann Capanna-Hodge is an expert in ADHD and RSD and frquently featured in the media.
- Parents Magazine: Are Your Kid's Meltdowns a Sign of Rejection Sensitive Dysphoria
- Healthline Understanding Self-Regulation Skills
- She Knows 11 Products Moms of Kids With ADHD Swear By to Maintain Order in the Chaos
- The Healthy 12 Silent Signs of Adult ADHD You Might Be Ignoring
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2023










