Pathological Demand Avoidance (PDA) : A Guide to Understanding and Treatment
Navigating the world of childhood behavioral disorders can be very challenging. When it comes to Pathological Demand Avoidance (PDA), those challenges multiply. How can we best support a child navigating a world that seems fraught with everyday demands that trigger anxiety? Let’s decode the PDA framework so we can empower those affected by it.
Table of Contents
Chapter 1: Understanding Pathological Demand Avoidance
Chapter 3: Pathological Demand Avoidance: Symptoms Overview
Chapter 4: Connection to Autism Spectrum Disorder
Chapter 5: Identifying Pathological Demand Avoidance in Children
Chapter 6: Common Behaviors and Signs of PDA
Chapter 7: Potential Misdiagnoses
Chapter 8: PDA and Overlapping or Similar Clinical Issues
Chapter 9: Pathological Demand Avoidance Parenting: A Journey of Understanding and Adaptation
Chapter 10: Strategies for Treating Pathological Demand Avoidance PDA in Children
Chapter 11: Coping Mechanisms and Therapeutic Interventions
Chapter 12: The Diagnostic Process for PDA
Chapter 13: Pathological Demand Avoidance Syndrome and Why It Isn't Accepted in the US
Key Takeaways
- What does PDA mean? PDA is Pathological Demand Avoidance, a behavioral profile characterized by extreme avoidance of ordinary demands caused by intense anxiety.
- Does my child have PDA? Identification involves recognizing resistance to everyday demands, difficulty with social interactions, mood swings, and imaginative emotional outbursts.
- What is PDA in kids? Parenting kids with PDA means learning all the strategies to support them, such as low-demand parenting/teaching approaches, building trust and connection, encouraging flexibility and adaptability as well as coping mechanisms and therapeutic interventions.
Chapter 1
Understanding Pathological Demand Avoidance
A term coined by British psychologist Elizabeth Newson in the 1980s, Pathological Demand Avoidance is a behavioral profile characterized by extreme avoidance of ordinary demands. Newson, associated with the National Autistic Society, observed a consistent pattern of behaviors in children under her care, which included a marked aversion to everyday tasks and the utilization of social tactics to avoid demands.
Such aversion is characterized by a leap into an imaginary world of role-play, a dive into obsessive behavior, or a sprint towards intense control. The creative avoidance strategies employed by children with PDA are too many and too creative.
Anxiety, fueled by the anticipation of demands and a lack of control, forms the foundation of the Pathological Demand Avoidance profile. The very thought of ordinary demands, be it getting dressed for school or finishing a meal, can trigger a cascade of anxiety in children with PDA. Given that PDA is a pervasive developmental disorder, these children face a unique challenge —the necessity to navigate an anxiety-laden world filled with everyday demands.
Chapter 2
What is PDA?
Every child with PDA carries a distinct set of characteristics etched into their behavioral profile. The most prominent among these is their tendency to resist ordinary demands, which is often paired with an overwhelming need for control.
Imagine a child caught in a whirlwind of instructions, their anxiety levels escalating with each demand. The child seeks refuge in a shell of control, using it as a shield against the barrage of demands.
A distinguishing trait of the PDA disorder is ‘surface sociability,’ where individuals appear to have stronger social skills than they genuinely do. They might dazzle you with their eye contact and conversational abilities, but beneath the surface, they grapple with complex social interactions and responsibilities.
If your child has PDA meaning their struggles often extend to their understanding of social hierarchies, then it will lead to challenges in social interactions, particularly in acknowledging or adhering to traditional authority figures or social norms.
Their emotional responses can range from introverted behavior to more open expressions of anger or anxiety, often as a result of pervasive demand avoidance, where the child tries to avoid demands that cause them stress.
Chapter 3
Pathological Demand Avoidance: Symptoms Overview
Before we delve further into the connection between autism and PDA, it's crucial to understand the wide-ranging Pathological Demand Avoidance symptoms. This PDA symptoms overview will help us better understand the behaviors and responses of PDA children, thus equipping us with the knowledge to provide them with the appropriate support and care.
- Extreme Resistance to Ordinary Demands: Children with PDA show extreme resistance to everyday demands. Even the simplest tasks such as getting dressed or eating a meal can trigger an intense reaction.
- Social Interaction Difficulties: Despite appearing sociable on the surface, children with PDA often struggle with social interactions. They may have difficulty understanding social cues and norms, leading to awkward or inappropriate interactions.
- Mood Swings: Children with PDA can have severe mood swings, ranging from periods of intense joy to periods of profound sadness or anger. These mood swings can occur without any apparent trigger and can be very difficult for the child to manage.
- Imaginative Emotional Outbursts: Children with PDA often have imaginative emotional outbursts. They may create elaborate fantasies or stories to avoid dealing with reality or to escape from demands.
- Obsessive Behavior: Children with PDA may exhibit obsessive behavior, often focused on a particular subject or activity. This obsession can serve as a coping mechanism to help them manage their anxiety.
- Difficulty with Routine: Children with PDA often struggle with routine and structure. They may resist following a set schedule and become anxious or upset when their routine is interrupted.
- Difficulty with Transitions: Transitions, whether it's transitioning from one activity to another or transitioning to a new environment, can be particularly challenging for children with PDA. They may resist or become anxious during transitions, leading to meltdowns or tantrums.
- Need for Control: Children with PDA often have a strong need for control. They may resist following instructions or rules and may become upset if they feel they are not in control.
- Difficulty with Authority: Children with PDA often struggle with authority figures due to underlying anxiety. They may resist following instructions from teachers, parents, or other authority figures, which causes conflicts and power struggles.
- Sensory Sensitivities: Many children with PDA have sensory sensitivities. They may be overly sensitive to certain sounds, textures, tastes, or smells, which can add to their anxiety and PDA avoidance behaviors.
What Causes Pathological Demand Avoidance?
The exact cause of PDA is not well-established, and it is an area of ongoing research within the broader context of autism spectrum disorder. Here are some factors that may contribute to the development of PDA:
- Neurobiological Factors: Like other forms of autism, PDA is believed to have a neurobiological basis, with differences in brain structure and function. However, the specific neural mechanisms underlying PDA are not yet fully understood.
- Genetic Factors: There is evidence to suggest a genetic component in the development of autism spectrum disorders, including PDA. Research indicates that certain genetic factors may contribute to an increased risk of ASD, although the exact genes involved are complex and not fully identified (Rylaarsdam & Guemez-Gamboa, 2019).
- Environmental Factors: Environmental influences during prenatal and early postnatal development may play a role in the development of PDA. Factors such as prenatal exposure to certain substances, complications during birth, or early life stressors could contribute.
- Interactions between Genetic and Environmental Factors: The development of PDA is likely influenced by a combination of genetic and environmental factors. The interplay between genetic predisposition and environmental influences may contribute to the expression of PDA traits.
- Social and Developmental Factors: Challenges in social communication and interaction are central to ASD, including PDA. Difficulties in understanding and responding to social cues may contribute to the development of PDA behaviors.
Chapter 4
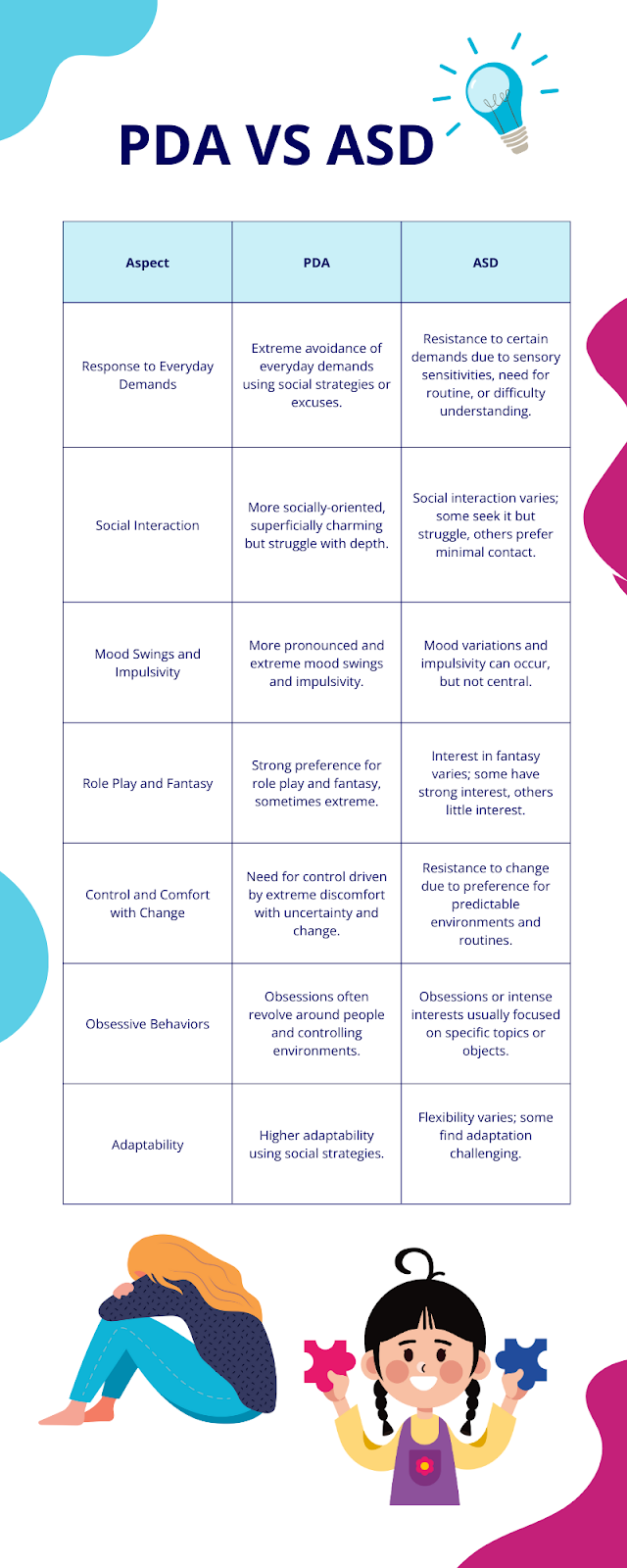
Connection to Autism Spectrum Disorder
The complex tapestry of PDA weaves a connection to Autism Spectrum Disorder, albeit a debated one. While some view PDA as a distinctive profile within the spectrum of autism, others argue it is a separate diagnosis altogether. But when an autistic child refuses to do anything, it’s most likely PDA autism.
There’s ongoing research into the link between PDA, autism spectrum disorder, and developmental disabilities (Woods, 2020). Knowing more about ASD and PDA will enrich our comprehension of this intricate behavioral profile.
Chapter 5
Identifying Pathological Demand Avoidance in Children

- Resisting and avoiding everyday demands
- Appearing sociable on the surface but struggling with social interactions
- Experiencing extreme mood swings and emotional overload
- Showing excessive and imaginative emotional outbursts
These behaviors often come to the forefront during preschool or early school years, paving the way for a PDA autism diagnosis, as PDA is considered an autism spectrum profile. Interestingly, when using a PDA autism test, PDA does not discriminate based on gender, with its prevalence being equal in boys and girls.
PDA is unique among childhood mental health conditions due to its hallmark behaviors of high anxiety and resistance to routine demands. A PDA kid frequently employs social manipulation to evade these demands and display behaviors that may be more externalized and physically aggressive or controlling.
Chapter 6
Common Behaviors and Signs of PDA
PDA is often the chameleon of behavioral disorders, mimicking the symptoms of other conditions such as Oppositional Defiant Disorder (ODD) or ADHD, which may cause misdiagnosis. The emotional outbursts that are a hallmark of these disorders often stem from the fight-flight or freeze response seen in children with PDA. However, PDA stands distinct in its intensity and pervasiveness. While ODD is characterized by deliberate defiance, PDA is driven by an overwhelming and consistent need to avoid or resist demands, placing it within the realm of autism spectrum profiles, unlike ODD.
Some anecdotal reports and studies provide some support for a connection between PDA and ADHD. Both conditions can result in attention difficulties, impulsivity, and hyperactivity. However, in the case of PDA, these symptoms are often exacerbated by the persistent demand avoidance behavior, making the diagnostic process even more complex (Malik & Baird, 2018).

Chapter 7
Potential Misdiagnoses
Incorrectly diagnosing PDA is similar to confusing a chameleon with a leaf. The potential misdiagnoses for PDA encompass oppositional defiant disorder (ODD), Attention Deficit Hyperactivity Disorder ADHD, and epilepsy, as PDA may exhibit traits similar to these conditions. The extreme resistance to everyday demands exhibited by individuals with PDA, characterized by a pathological avoidance of demands, is not typically seen in individuals with ADHD.
The potential misdiagnosis of PDA as epilepsy can be attributed to the similarity in symptoms between the two conditions, including neurological issues and anxiety-related behaviors.
Chapter 8
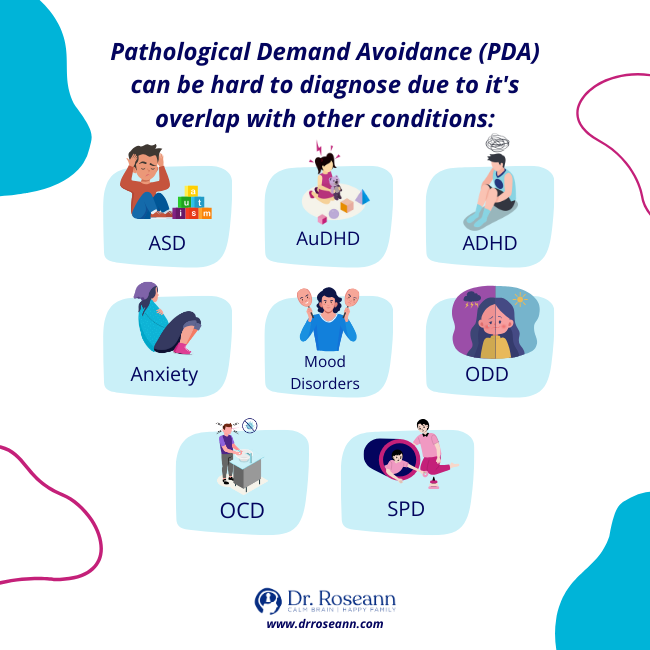
PDA and Overlapping or Similar Clinical Issues
Pathological Demand Avoidance (PDA), while unique in its presentation, shares similarities with several other clinical issues. Understanding these similarities and differences is crucial for accurate diagnosis and effective intervention strategies, especially when conditions like PDA and AuDHD overlap. These include:
- Autism Spectrum Disorder (ASD): PDA is often considered a profile within the autism spectrum, sharing common traits like social communication difficulties and repetitive behaviors.
- Attention Deficit Hyperactivity Disorder (ADHD): Similarities include difficulties with impulse control and maintaining attention, although the motivations and responses can differ.
- AuDHD: AuDHD represents a complex blend of ASD and ADHD characteristics.
- Anxiety Disorders: PDA involves a significant anxiety component, especially related to demands and expectations, much like various anxiety disorders.
- Obsessive-Compulsive Disorder (OCD): There can be overlaps in the need for control and the presence of compulsive behaviors, although the underlying reasons may differ.
- Oppositional Defiant Disorder (ODD): Both PDA and ODD involve resistance to authority, but the motivation behind this resistance is different (anxiety-driven in PDA versus power struggle in ODD).
- Sensory Processing Disorder: Individuals with PDA may also experience sensory sensitivities, common in those with sensory processing issues.
- Executive Functioning Disorders: Challenges with organization, planning, and flexibility seen in PDA are also characteristic of executive functioning disorders.
- Eating Disorders: In some cases, the need for control inherent in PDA can manifest in eating patterns, leading to eating disorder-like behaviors.
- Mood Disorders: Mood swings and emotional dysregulation in PDA can resemble symptoms of mood disorders like depression or bipolar disorder.
- Social (Pragmatic) Communication Disorder: Difficulties with the social aspects of communication seen in PDA are also a feature of this disorder.
Chapter 9
Pathological Demand Avoidance Parenting: A Journey of Understanding and Adaptation
PDA parenting is a journey filled with challenges, learning, patience, and immense love. It requires understanding the unique behavioral profile of your child, adapting your parenting strategies to meet their needs, and providing a supportive environment that promotes their growth and development. It's about more than just managing behaviors – it's about understanding the root causes of those behaviors and finding ways to alleviate the PDA anxiety that drives them.
This journey, while challenging, can also be incredibly rewarding. It can deepen your understanding of your child and strengthen your bond with them. It can also lead to personal growth as you learn to navigate the complexities of PDA and develop resilience and adaptability.
Exploring various strategies for supporting and disciplining children with PDA, including low-demand parenting and teaching approaches, building trust and connection, and encouraging flexibility and adaptability can help. Developing coping mechanisms is key as well as including therapeutic interventions that can assist in managing PDA and even prevent the Failure to Launch Syndrome.
Chapter 10
Strategies for Treating Pathological Demand Avoidance PDA in Children

Establishing trust and connection with children with PDA creates a secure environment that diminishes their anxiety and provides a sense of understanding and support. Promoting flexibility and adaptability in children with PDA enhances their ability to cope with changes and minimizes their anxiety.
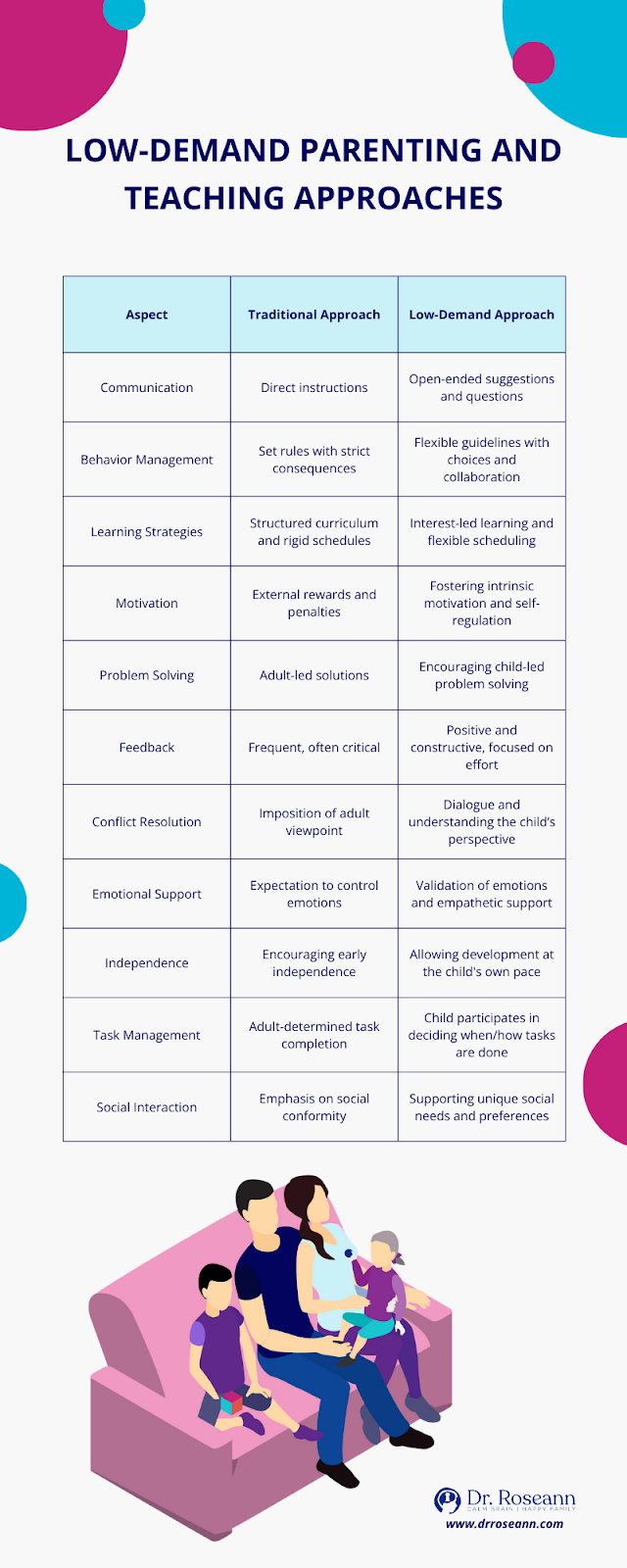
What is Low-Demand Parenting?
Low-demand parenting and teaching strategies hinge on eschewing demand words like ‘must,’ ‘should,’ ‘have to,’ ‘need to,’ ‘now,’ and ‘immediately,’ as they can incite anxiety and avoidance behaviors in children with PDA. It’s like trying to coax a cat out of a tree. The cat won’t go down if you issue a direct order. But it might budge if you offer it a choice of treats.
Requests can be depersonalized by utilizing written notes or visual prompts, which make demands feel less direct and oppressive. Moreover, using humor can reduce the personal feel of the requests, making them more acceptable to the child.
Indirect praise also plays a crucial role in teaching children with PDA. It offers positive reinforcement and appreciation in a way that avoids placing direct demands on them. The low demand lifestyle autism approach can result in higher levels of engagement and motivation compared to direct praise or rewards, which may not effectively resonate with children who have the autism PDA profile.
Building Trust and Connection
Building Pathological Demand Avoidance relationships is a journey marked by trust and connection. Establishing trust is akin to building a bridge over the chasm of anxiety, creating a secure environment that diminishes their fear and provides a sense of understanding and support. Strategies to cultivate trust include establishing a more equal relationship based on collaboration and respect and using humor, playfulness, and goofiness to foster a bond.
Also, providing choices and allowing the child to have a sense of control can contribute to the development of trust. The impact of trust on the behavior of a child with PDA is significant. It enables the child to:
- Feel understood
- Feel accepted
- Feel supported
- Improve
- Cooperate
- Engage in activities
This leads to improved cooperation and engagement in activities.
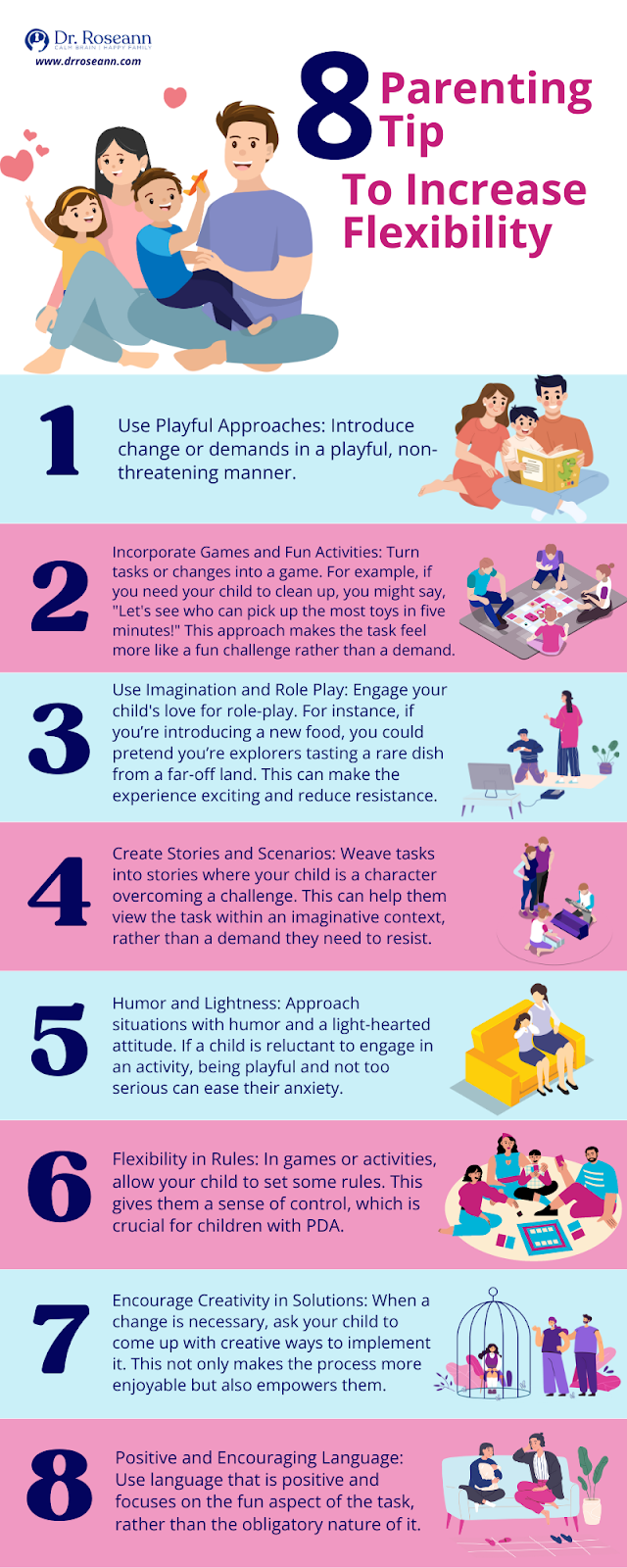
Encouraging Flexibility and Adaptability
Fostering flexibility and adaptability in children with PDA equates to teaching them to embrace change. It enhances their ability to cope with shifts in routine and minimizes their anxiety. Strategies encompass:
- Preparing the child for changes
- Employing non-confrontational language
- Introducing novelty and variety
- Engaging them in problem-solving
Just like a river adjusting its course in response to a boulder, children learn to adapt to changes and transitions.
A structured routine, akin to the riverbed guiding the water, offers a predictable and consistent schedule, providing a sense of security and stability that can reduce anxiety and resistance to demands.
Chapter 11
Coping Mechanisms and Therapeutic Interventions

Professional guidance and support from a PDA psychologist or therapist can provide valuable insights, support, and coping strategies.
Mindfulness Techniques
For those with PDA, mindfulness techniques serve as a calming anchor amidst the storm. They aid in enhancing emotional regulation, decreasing stress, and offering coping mechanisms for emotional reactions. By enhancing their awareness of emotions and physiological responses, mindfulness enables them to:
- Make deliberate choices when faced with demands and triggers
- Stay present in the moment
- Practice self-compassion and self-care
- Cultivate a sense of acceptance and non-judgment
These techniques can be powerful tools for individuals with PDA to navigate their daily lives with greater ease and resilience.
Specific mindfulness techniques for individuals with PDA include:
- Mindful breathing exercises
- Body scan meditation
- Mindful movements such as yoga or tai chi
- Mindful eating
- Practices of mindful self-compassion
Neurofeedback and PDA: How Brain Training Reduces Resistance
Neurofeedback, also known as EEG Biofeedback, is a groundbreaking approach that offers a new perspective on managing PDA. This non-invasive technique involves direct training of the PDA brain, allowing it to function more efficiently. The process is akin to physical training, but instead of muscles, it strengthens the neural pathways in the brain.
The premise of this technique is to provide real-time feedback to the brain, enabling it to self-regulate and optimize its performance. The brain is rewarded for changing its activity to more appropriate patterns. This reward system encourages the brain to learn new patterns and pathways, helping to alleviate symptoms associated with PDA psychology.
Neurofeedback has been shown to reduce resistance in individuals with PDA by promoting relaxation, enhancing focus, and improving overall cognitive function. It helps the brain self regulate. The technique can also help to manage anxiety, a key trigger for PDA, by teaching the brain to recognize and respond to stress more effectively (Dalkner et al., 2017).
In neurofeedback sessions, sensors are placed on the scalp to measure brainwave activity. This information is displayed on a monitor in real-time, allowing the individual to see their brain's activity and learn how to control it. By viewing their brainwave patterns, individuals can learn to modify their brain function, reducing PDA symptoms in children.
Magnesium to Improve Motivation and Cognitive Processing
Magnesium, though often overlooked, is a mineral that plays a pivotal role in our body. It is involved in over 300 enzymatic reactions within the body, including the metabolism of food, the synthesis of fatty acids and proteins, and the transmission of nerve impulses.
In the context of Pathological Demand Avoidance (PDA), magnesium can have a significant impact on motivation and cognitive processing. Magnesium is essential for the proper functioning of the nervous system and brain functions, affecting our level of alertness and cognitive abilities (Mathew & Panonnummal, 2021).
Magnesium deficiency can lead to a reduction in motivation, and energy, and an increase in anxiety levels. On the other hand, maintaining optimal levels of magnesium can improve cognitive processing and boost motivation. This is particularly beneficial for individuals with PDA, as they often struggle with these areas.
Incorporating magnesium-rich foods into the diet or taking magnesium supplements, under the guidance of a healthcare professional, can help manage the symptoms of PDA and improve the overall quality of life.
However, it is important to note that while magnesium can help improve motivation and cognitive processing, it is not a standalone solution for managing PDA. It should be part of a comprehensive management plan that includes a variety of strategies and interventions.
Professional Guidance and Support
Professional guidance, much like a lighthouse guiding ships to safety, is essential in managing PDA. Education professionals offer guidance and support to both the child and their families in comprehending and addressing the difficulties linked with PDA. A PDA-informed professional should possess:
- Familiarity with the practice guidance for identifying and assessing a PDA profile
- Experience and expertise in working with individuals with PDA
- Knowledge of mindful skills to support individuals with PDA
- Attendance at therapy or training sessions with PDA-informed professionals
Cognitive behavioral therapy and occupational therapy have been identified as effective Pathological Demand Avoidance treatments.
Chapter 12
The Diagnostic Process for PDA

Assessment Tools and Questionnaires
The Extreme Demand Avoidance Questionnaire (EDA-Q) and other assessment tools are like a compass in the diagnostic process of PDA. They play a role in identifying PDA traits in individuals, although they should not be solely relied upon for definitive PDA diagnosis.
The EDA-Q is a 26-item questionnaire specifically designed for research and diagnostic purposes in school-age children, aiming to measure behaviors and traits associated with extreme/pathological demand avoidance disorder (O’Nions et al., 2013).
However, it should be noted that while a Pathological Demand Avoidance checklist assesses traits and behaviors associated with Pathological Demand Avoidance, it is not intended for diagnostic purposes and should not be utilized as such.
Challenges in Pathological Demand Avoidance Diagnosis
The challenges in the diagnosis of PDA are like trying to find a specific tree in a dense forest. The debate about the relationship of autism with PDA and the latter’s absence from the major diagnostic manuals complicates its identification. The absence of official recognition in diagnostic manuals results in the absence of standardized diagnostic criteria or guidelines, complicating the process for healthcare professionals to identify and diagnose the condition accurately.
Furthermore, the challenge of diagnosing PDA arises from:
- Its spectrum nature
- The extreme behavior pattern to resist everyday demands
- The overlap with other conditions, such as ODD and ADHD
- The underlying motivations for the avoidance behavior.
Chapter 13
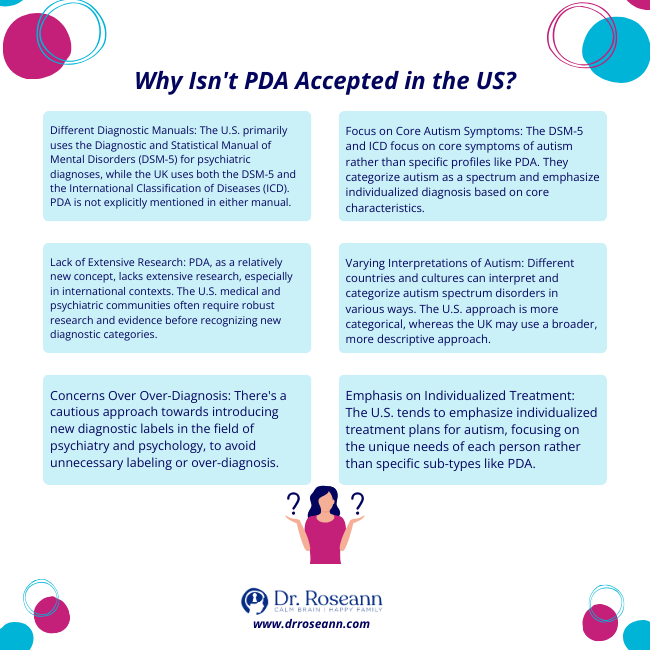
Pathological Demand Avoidance Syndrome and Why It Isn't Accepted in the US
In the US, the lack of PDA recognition resembles a puzzle missing a piece. Its absence from the major diagnostic manuals, including the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), and the International Classification of Diseases, Tenth Revision (ICD-10), contributes to this.
However, in the US, the measures to attain recognition of Pathological Demand Avoidance Syndrome in children involve continuous research and advocacy efforts focused on enhancing understanding of the condition and advocating for its inclusion in diagnostic manuals.
The Future of PDA Research and Recognition
The future of PDA research and recognition resembles a photograph developing, slowly unveiling a more precise image. The current level of awareness about PDA in the United States is relatively low compared to other regions, but there are active research initiatives focused on Pathological Demand Avoidance.
Advancing studies and raising awareness is vital for securing official recognition and assistance for individuals with PDA. This recognition will improve the diagnosis, treatment, and overall quality of life for those impacted by PDA.
Ongoing Research and Development
The ongoing research and developments in PDA are like pieces of a jigsaw puzzle coming together to form a more complete picture. The most recent discoveries indicate that PDA is a multifaceted profile within the autism spectrum marked by significant avoidance of demands (Kildahl et al., 2021).
The primary areas of focus in the ongoing studies on PDA include diagnosis, treatment methodologies, and a holistic comprehension of PDA.
Advocacy for Official Recognition
Campaigning for official PDA recognition can be compared to embarking on a voyage of change. Organizations such as the PDA North America and the PDA Society in the UK are at the forefront of this movement. Individuals can engage in advocating for PDA recognition through various means such as raising awareness, joining support groups, and communicating with policymakers.
Navigating the challenges of PDA in kids is a complex journey. However, with an understanding of the condition, identification of common signs and behaviors, the implementation of supportive strategies, and the application of effective coping mechanisms, we can make this journey less daunting. The ongoing research and advocacy for official recognition of PDA promise a brighter future for those affected by this condition.
What is P.D.A.?
Pathological Demand Avoidance is a behavioral profile where individuals experience extreme avoidance of everyday demands. It is associated with autism but is not officially recognized as a distinct diagnosis.
What is Demand Avoidance?
It's important to note that while demand avoidance is a characteristic associated with PDA, not everyone who exhibits demand avoidance necessarily has PDA. Demand avoidance can be present in various conditions or situations, and it is not exclusive to any specific diagnostic category. In some cases, demand avoidance may be a behavioral response to anxiety, sensory issues, or other underlying factors.
What is PDA in Children?
PDA kids may avoid and resist routine tasks causing difficulties in various aspects of their daily lives. They often experience high levels of anxiety, especially in response to demands or expectations placed on them. Common examples of PDA in toddlers are difficulty getting dressed, eating specific foods, or transitioning between activities.
What is a PDA Profile?
A PDA profile refers to a specific set of characteristics and behaviors observed in individuals, particularly children, with autism spectrum disorder, characterized by heightened anxiety, an intense need for control, and strong resistance to routine demands and requests.
What are Avoidance Behaviors?
Avoidance behaviors refer to actions or strategies that individuals use to prevent or escape from situations, stimuli, or demands that they find distressing, anxiety-provoking, or overwhelming. Some examples include avoiding social situations, procrastination, and sensory avoidance.
What are Examples Of Pathological Demand Avoidance in Children?
An example of a PDA child uses strategies like making excuses, distracting, procrastinating, using threats, and physically incapacitating themselves to avoid demands. There are other pathological demand avoidance examples such as emotional outbursts or meltdowns, resistance to authority, and superficially sociable behavior.
What is PDA Autism?
PDA Autism describes a particular profile within the autism spectrum characterized by an extreme need to avoid external demands due to anxiety. The autistic with PDA often struggle with traditional strategies for managing behavior, as they may react strongly to demands, requests, or even seemingly simple tasks.
How Can You Determine an Autism PDA Syndrome?
Diagnosing PDA in autism involves a comprehensive assessment by qualified professionals. These experts determine pathological demand avoidance in autism through observation of behavior, consideration of diagnostic criteria for Autism Spectrum Disorder, clinical interviews, behavioral assessments, collaboration with school and home environments, and the exploration of co-occurring conditions.
Can You Have PDA Without Autism?
Some individuals who exhibit features of PDA may not meet the criteria for a traditional autism diagnosis. It’s why there’s an ongoing debate among professionals about the relationship between PDA and autism. Some argue that it might represent a distinct subcategory within the broader autism spectrum, effectively making it an autistic PDA profile.
Do Children Grow Out of Pathological Demand Avoidance?
Although there is no definitive cure for Pathological Demand Avoidance, good teaching and encouragement can help children improve their abilities over time. Kids with autism and pathological demand avoidance may show different symptoms compared to other children within the spectrum.
Is Pathological Demand Avoidance in DSM-5?
Pathological Demand Avoidance (PDA) is not a formal diagnosis in the DSM-5 or ICD-10 and is not well known in the U.S., though it is widely acknowledged in the U.K. An anxiety-driven, persistent demand for autonomy is at its core, causing someone to avoid demands and expectations to remain in control.
What is a PDA Diagnosis?
As PDA is not yet officially recognized as a separate diagnostic category in the DSM-5, it follows the autism diagnostic criteria. A PDA diagnosis includes persistent deficits in social communication and social interaction, as well as restricted, repetitive patterns of behavior, interests, or activities.
Why is Pathological Demand Avoidance not recognized in the US?
Pathological Demand Avoidance is not officially recognized in the US as it is yet to be included in DSM-5 and ICD-10, and lacks international recognition. This has led to arguments that the label pathologizes and punishes self-advocacy among individuals with avoidant autism.
Citations
ReferencesDalkner, N., Unterrainer, H. F., Wood, G., Skliris, D., Holasek, S. J., Gruzelier, J. H., & Neuper, C. (2017). Short-term Beneficial Effects of 12 Sessions of Neurofeedback on Avoidant Personality Accentuation in the Treatment of Alcohol Use Disorder. Frontiers in Psychology, 8. https://doi.org/10.3389/fpsyg.2017.01688
Kildahl, A. N., Helverschou, S. B., Rysstad, A. L., Wigaard, E., Hellerud, J. M., Ludvigsen, L. B., & Howlin, P. (2021). Pathological demand avoidance in children and adolescents: A systematic review. Autism, 25(8), 136236132110343. https://doi.org/10.1177/13623613211034382
Malik, O., & Baird, G. (2018). Commentary: PDA – what’s in a name? Dimensions of difficulty in children reported to have an ASD and features of extreme/pathological demand avoidance: a commentary on O’Nions et al. (2017). Child and Adolescent Mental Health, 23(4), 387–388. https://doi.org/10.1111/camh.12273
Mathew, A. A., & Panonnummal, R. (2021). “Magnesium”-the master cation-as a drug—possibilities and evidences. BioMetals, 34(5), 955–986. https://doi.org/10.1007/s10534-021-00328-7
O’Nions, E., Christie, P., Gould, J., Viding, E., & Happé, F. (2013). Development of the “Extreme Demand Avoidance Questionnaire” (EDA-Q): preliminary observations on a trait measure for Pathological Demand Avoidance. Journal of Child Psychology and Psychiatry, 55(7), 758–768. https://doi.org/10.1111/jcpp.12149
Rylaarsdam, L., & Guemez-Gamboa, A. (2019). Genetic causes and modifiers of autism spectrum disorder. Frontiers in Cellular Neuroscience, 13(13). https://doi.org/10.3389/fncel.2019.00385Woods, R. (2020, August 5). PDA – a new type of disorder? Thepsychologist.bps.org.uk. https://openresearch.lsbu.ac.uk/item/8v10v
Dr. Roseann is a mental health expert in Neurodivergence who frequently is in the media:
- Helping Children Thrive Podcast Benefits of Neurofeedback for children with ADHD
- Very Well Mind What Is Asperger Syndrome?
- Parents Are Your Kid's Meltdowns a Sign of Rejection Sensitive Dysphoria?
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of
147 Therapist-Endorsed Self-Regulation Strategies for Children: A Practical Guide for Parents
Dr. Roseann is a Children’s Mental Health Expert and Licensed Therapist who has been featured in/on hundreds of media outlets including The Mel Robbins Show, CBS, NBC, PIX11 NYC, Today, FORBES, CNN, The New York Times, The Washington Post, Business Insider, Women’s Day, Healthline, CNET, Parade Magazine and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She coined the terms, “Re-entry panic syndrome” and “eco-anxiety” and is a frequent contributor to media on mental health.
Dr. Roseann Capanna-Hodge has three decades of experience in working with children, teens and their families with attention-deficit hyperactivity disorder (ADHD), autism, concussion, dyslexia and learning disability, anxiety, Obsessive Compulsive Disorder (OCD), depression and mood disorder, Lyme Disease, and PANS/PANDAS using science-backed natural mental health solutions such as supplements, magnesium, nutrition, QEEG Brain maps, neurofeedback, PEMF, psychotherapy and other non-medication approaches.
She is the author of three bestselling books, It’s Gonna Be OK!: Proven Ways to Improve Your Child's Mental Health, The Teletherapy Toolkit, and Brain Under Attack. Dr. Roseann is known for offering a message of hope through science-endorsed methods that promote a calm brain.
Her trademarked BrainBehaviorResetⓇ Program and It’s Gonna be OK!Ⓡ Podcast has been a cornerstone for thousands of parents facing mental health, behavioral or neurodevelopmental challenges.
She is the founder and director of The Global Institute of Children’s Mental Health, Neurotastic™Brain Formulas and Dr. Roseann Capanna-Hodge, LLC. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Mental Health Professional (CIMHP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF).
© Roseann-Capanna-Hodge, LLC 2024


