Estimated reading time: 7 minutes
If your child is stuck thinking about their breathing, blinking, or heartbeat—and it’s starting to take over their day—you’re not alone.
This lesser-known type of OCD, called Somatic OCD (or sensorimotor OCD), can be incredibly distressing, making kids hyperaware of things most of us don’t even notice.
In this blog, we’ll break down what somatic OCD is, how it shows up in kids, and how you can help your child feel calm and in control again.
What is Somatic OCD, and How Does it Differ From Other Types of OCD?
Somatic OCD—sometimes called sensorimotor OCD—isn’t your typical type of OCD.
Instead of worrying about germs or something bad happening, kids with somatic OCD get stuck on what’s going on inside their own body.
Things like their breathing, blinking, or heartbeat suddenly become front and center—and they can’t tune it out.
Most of us never notice those things, right? But for these kids, it’s all they can think about. And the more they notice it, the more anxious they feel.
Here’s what makes it different:
- They’re hyperaware of things that should be automatic. Like, a child might say, “I can’t stop thinking about my blinking—it’s driving me nuts.”
- They try to stop the thoughts, but that usually makes it worse.
They feel stuck in a loop, and it’s incredibly distressing—for them and for you as a parent watching it happen.
Signs and Symptoms of Somatic OCD in Children?
Children with somatic OCD may exhibit:
- Obsessive focus on bodily functions: Constantly thinking about breathing, blinking, or heartbeat.
- Distress over inability to ignore sensations: Expressing frustration about not being able to stop noticing certain bodily functions.
- Compulsive behaviors: Engaging in rituals or seeking reassurance to alleviate distress.
- Avoidance behaviors: Avoiding situations that might trigger focus on bodily sensations.
| Somatic Obsessions | Somatic Compulsions |
|---|---|
| Breathing: Constantly focused on how fast or deep they’re breathing. Worries it might stop if they don’t pay attention. | Checking breathing or pulse: Using devices or asking others to make sure they’re “okay.” |
| Heartbeat: Obsessing over the feeling or rhythm of their heartbeat. Afraid something’s wrong. | Seeking medical reassurance: Asking for frequent doctor visits or tests to check their body. |
| Blinking or swallowing: Noticing every blink or swallow—and can’t stop thinking about it. | Rituals: Swallowing or blinking in a certain way “just in case.” |
| Digestion: Hyperaware of tummy gurgles or how food feels moving through. | Mirror checking: Watching themselves breathe, blink, or swallow in the mirror. |
| Muscle tension: Constantly scanning for tightness in their neck, back, or jaw. | Touching or tapping: Repeating physical actions to reset or “fix” sensations. |
| Skin sensations: Noticing every itch, tingling, or temperature change and worrying it’s something serious. | Counting or timing: Counting breaths, swallows, or blinks to feel in control. |
| Posture or balance: Obsessing about how their body feels standing or sitting. | Avoidance behaviors: Steering clear of quiet places where bodily sensations feel louder. |
Is Your Child’s Focus OCD or a Medical Issue?
Distinguishing between somatic OCD and a medical condition can be challenging. Consider the following:
- Medical evaluation: Always rule out medical conditions first.
- Pattern of focus: OCD-related focus is persistent and distressing, often without a medical basis.
- Behavioral signs: Look for compulsive behaviors or rituals associated with the focus.
What Causes Somatic OCD in Kids?
The exact cause of somatic OCD is not fully understood, but factors may include
- Family history: If someone in your family has OCD or anxiety, your child might be more likely to develop it too.
- Brain wiring: Some kids’ brains naturally process sensations differently, making it hard to “turn off” those body-focused thoughts.
- Stress or tough experiences: Big changes, trauma, or ongoing stress can trigger or make symptoms worse.
What Treatments Are Effective for Somatic OCD?
Somatic OCD can be effectively treated with the right mix of therapies and brain-calming tools, many kids improve dramatically.
We’ve seen the best results with a combined approach—supporting the brain while also changing how it reacts to obsessive thoughts.
Key Tools That Support Healing:
- ERP Therapy (Exposure and Response Prevention): The gold standard for OCD. Kids learn to face the sensations they fear—without giving in to compulsions.
- CBT (Cognitive Behavioral Therapy): Helps reframe scary or intrusive thoughts and break the thought-behavior cycle.
- Neurofeedback: Calms an overstimulated brain and supports better focus and emotional regulation.
- PEMF Therapy: Sends soothing pulses to the brain and body to help with self-regulation and calm.
- Supplements and Nutrition: Certain nutrients support brain health and emotional regulation.
- Lifestyle changes: Diet, sleep, and movement all matter when you’re rewiring the brain.
What Does Somatic ERP Therapy Look Like?
Somatic ERP helps kids get comfortable with being uncomfortable. It gently guides them to notice a body sensation—like their breath—without doing something to “fix” or avoid it. Over time, their brain learns: This sensation isn’t dangerous. I don’t have to react.
It breaks the cycle. Every time your child resists a compulsion, the brain learns that the discomfort isn’t dangerous. And with enough practice, the obsession loses its power.
Examples of Somatic ERP Exercises:
| Exposure Type | What It Might Look Like |
|---|---|
| Focused Awareness | Have your child sit quietly and notice their breathing or heartbeat—without changing it or checking it. |
| Delay Rituals | Encourage waiting 1 minute before blinking intentionally or swallowing on purpose—then increase to 3, 5, and 10 minutes. |
| Mindfulness Exercises | Walk barefoot and notice the ground, then shift attention to the trees or sounds outside. Learn to move in and out of body awareness. |
| Skip the Doctor | Help your child practice not asking to go to the doctor for every new body sensation (with therapist support). |
| Body Sensation Tolerance | Use warm/cool showers or gentle exercise to increase awareness of the body—then practice staying calm without reacting. |
| Imaginal Exposures | Work with a therapist to imagine scary “what ifs” (like “What if I always notice my breathing?”) and sit with the discomfort. |
| Technology Tools | Try an app or guided meditation that draws attention to the body—then have your child practice shifting their focus away. |
How Can I Support My Child at Home?
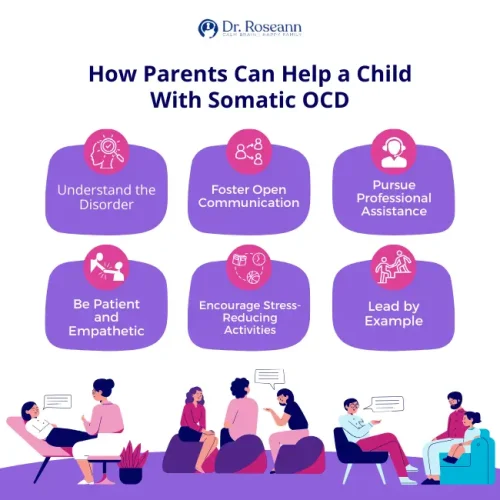
Supporting your child at home involves:
- Open communication: Encourage your child to talk about their feelings without judgment.
- Avoiding reassurance rituals: Refrain from repeatedly reassuring your child, as it can reinforce OCD behaviors.
- Establishing routines: Consistent daily routines can provide a sense of stability.
- Modeling coping strategies: Demonstrate healthy ways to manage anxiety.
When Should I Seek Professional Help?
Seek professional help if:
- Persistent distress: Your child’s focus on bodily sensations causes significant distress.
- Interference with daily life: The obsessions and compulsions interfere with school, social activities, or family life.
- Lack of improvement: Symptoms persist or worsen over time.
Parent Action Steps
FAQs
What is the difference between somatic OCD and health anxiety?
Somatic OCD involves obsessive focus on normal bodily sensations, while health anxiety centers on fears of having a serious illness.
Can somatic OCD go away on its own?
While symptoms may fluctuate, professional treatment is often necessary for significant improvement.
Is somatic OCD common in children?
Somatic OCD is less common than other OCD subtypes but can occur in children.
How long does treatment take?
Treatment duration varies, but many children show improvement within several months of consistent therapy.
Can diet or supplements help?
While not a primary treatment, a healthy diet and certain supplements may support overall mental health.
Citations
Freeman, J. B., Sapyta, J., Garcia, A., Franklin, M. E., Khanna, M., Moore, P., … & March, J. S. (2014). Family-based treatment of early childhood obsessive-compulsive disorder: The Pediatric Obsessive-Compulsive Disorder Treatment Study for Young Children (POTS Jr)—a randomized clinical trial. JAMA Psychiatry, 71(6), 689–698. https://doi.org/10.1001/jamapsychiatry.2014.170
Franklin, M. E., Sapyta, J., Freeman, J. B., Khanna, M., Compton, S., Almirall, D., … & March, J. S. (2011). Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive-compulsive disorder: The Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. JAMA, 306(11), 1224–1232. https://doi.org/10.1001/jama.2011.1344
Piacentini, J., Bergman, R. L., Keller, M., & McCracken, J. T. (2003). Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology, 13(Suppl 1), S61–S69. https://doi.org/10.1089/104454603322126359
Storch, E. A., Merlo, L. J., Lack, C., Geffken, G. R., Goodman, W. K., Murphy, T. K., & Lehmkuhl, H. D. (2008). Cognitive-behavioral therapy promotes long-term change in youth with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 47(5), 533–539. https://doi.org/10.1097/CHI.0b013e31816765d6
Dr. Roseann Capanna-Hodge is a licensed mental health expert that is frequently cited in the media:
- Single Care Controlling the uncontrollable: Living with OCD during a pandemic
- Holistic Counseling Podcast: Effective Treatments for OCD
- Epidemic Answers: Neurofeedback for ADHD, anxiety, OCD and mood
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Take our free quiz to assess OCD symptoms
©Roseann Capanna-Hodge LLC 2025










