Find out which ADHD treatments work — and which don’t — so you can help your child calm, focus, and succeed without wasted time or guesswork.
If your child’s ADHD feels like a constant struggle, you’re not alone — childhood clinical mental health issues are on the rise. But there are real, brain-based solutions that can make daily life easier. ADHD treatments today go far beyond medication, offering a range of natural, brain-based, and therapeutic options that can make an enormous difference in your child’s life. This guide walks you through what really works — and what often doesn’t — so you can feel empowered to make the best decisions for your family.

Where Should Parents Start With ADHD Treatment?
Learning that your child has ADHD can leave you with dozens of questions and a heart full of worry. Where do you even begin? The first and most important step is understanding that ADHD isn’t caused by poor parenting — it’s a brain-based disorder of regulation. Once you reframe ADHD as a brain difference rather than a behavior problem, it becomes much clearer how to help your child. Building the right foundation early can prevent years of struggle down the road.
| Step | Action | Why it Matters |
|---|---|---|
| 1 | Learn about ADHD | Reduces confusion and guilt |
| 2 | Find trusted help | Creates a treatment roadmap |
| 3 | Start calming the brain | Emotional regulation must come first |

Do I Have to Use Medication for ADHD?
One of the most common questions parents ask is whether they have to put their child on medication. The simple answer: No, you have choices. While ADHD medications can help some kids tremendously by improving focus and reducing hyperactivity, they aren’t the only way to manage ADHD. Understanding all the options allows you to make an informed, personalized decision that fits your child’s needs and your family’s values.
Options for ADHD Treatment in Children
| Common ADHD Treatments | Pros | Cons |
|---|---|---|
| Stimulant Medication | Rapid symptom relief | Possible side effects like appetite loss, sleep issues |
| Behavioral Therapy | Builds skills, no side effects | Takes time to see changes |
| Holistic Options (Neurofeedback, PEMF, Supplements) | Root cause focus | May require more commitment |

Dr. Roseann’s BrainBehaviorReset® Program and ADHD
Oscar’s parents created a structured after-school routine, improved his diet, and added neurofeedback. Within three months, tantrums dropped by 50% without medication. His teacher noticed better focus, and his parents felt empowered.
ADHD Treatment Options: Medication and Beyond
| Medication | Natural Solutions |
|---|---|
| Immediate symptom relief | Supports long-term brain regulation |
| Helps boost focus quickly | Improves emotional resilience and focus naturally |
| Possible side effects (sleep, appetite, mood) | Strengthens overall health without medication side effects |
What is the Best Non Medication Treatment for an ADHD Child?
More families today are seeking alternatives to medication — and for good reason. Natural and brain-based therapies can be incredibly effective in improving attention, impulse control, and emotional regulation. These options often get to the root of the problem: an under- or over-stimulated nervous system. Let’s look at the most effective non-medication treatments for ADHD.
| Treatment | Benefits |
|---|---|
| Neurofeedback | Retrains brainwaves for focus and calm |
| PEMF Therapy | Calms the nervous system naturally |
| Nutrition Changes | Supports brain function (Omega-3s, Magnesium) |
| Executive Function Coaching | Improves planning, organizing, and following through |
| Exercise | Boosts dopamine and reduces hyperactivity |
“ADHD is the most treatable disorder in psychiatry… The biggest problem is, most people don’t get treatment.” — Dr. Russell Barkley
ADHD Treatments Without Medication
If you’re concerned about medication side effects or just want a more holistic approach, you’ll be relieved to know there are many ways to support your child’s ADHD naturally. Calming the brain, regulating the nervous system, and improving nutritional status can have profound effects without any prescription drugs.
| Natural Approach | Benefit |
|---|---|
| Neurofeedback | Trains the brain to regulate focus and behavior |
| PEMF Therapy | Supports cellular healing and stress reduction |
| Mindfulness Practices | Helps emotional regulation and self-awareness |
| Nutrition and Supplements | Corrects deficiencies impacting brain function |
| Behavioral Strategies | Builds executive function and coping skills |

How to Treat An ADHD Child at Home
Home life is the single most powerful environment for a child with ADHD. The routines you set, the emotional climate you create, and the strategies you use daily shape your child’s ability to self-regulate and thrive. Small, consistent changes at home can lead to big shifts in focus, mood, and behavior over time.
| Home Strategy | Impact |
|---|---|
| Neurofeedback at Home | Changing brainwave and neurotransmitter function to improve attention, impulse control and working memory |
| CALM PEMF® | Regulates the brain and improves focus |
| Morning and Evening Routines | Reduces stress and builds predictability |
| Positive Attention | Boosts motivation and cooperation |
| Brain Breaks | Improves focus and reduces frustration |
| Visual Supports (charts, reminders) | Strengthens independence |
| Family Movement Activities | Regulates the nervous system and mood |

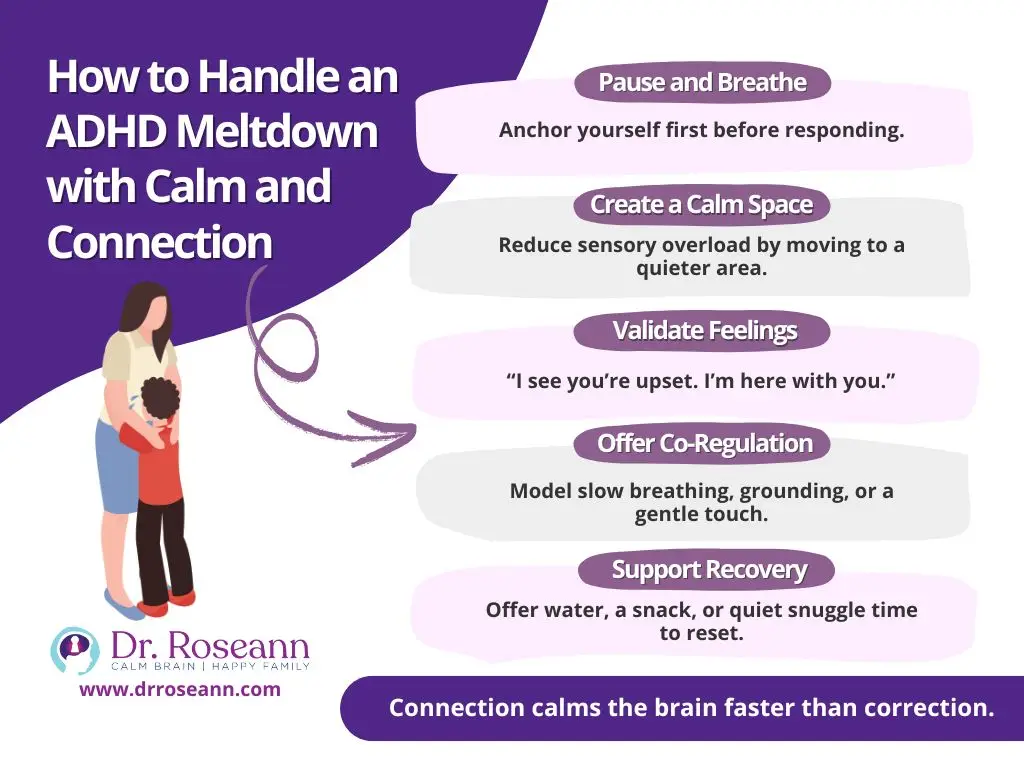
How Can I Help My Child Through ADHD Meltdowns?
When emotions boil over, it can feel like everything is spiraling out of control. Meltdowns are not “bad behavior” — they are a child’s cry for help when their nervous system is overwhelmed. Handling these intense moments with calm, compassion, and simple regulation strategies can make all the difference.
One of the best ways to respond is using Dr. Roseann’s CALMS™ approach:
- C: Co-Regulate First — Calm yourself so your child can match your regulated state.
- A: Avoid Personalizing — Remember, your child’s behavior is not a reflection of your parenting; it’s a dysregulated nervous system.
- L: Look for Root Causes — Dysregulation is a symptom. Ask: is it hunger, overstimulation, anxiety, or exhaustion?
- M: Model Coping Strategies — Show breathing, stretching, or other calming tools.
- S: Support and Reinforce — Praise calming behaviors and reinforce emotional regulation with connection and encouragement.
This framework helps parents stay grounded and teaches children the lifelong skills they need to manage their emotions and behavior effectively.
Choosing your words carefully during a dysregulated moment is just as important as your actions. Certain phrases can escalate a situation, while others can create calm and connection. Here’s a quick guide:
What to Say to a Dysregulated ADHD Kid and What Not to
| Say This | Instead of This |
|---|---|
| "I’m here. Let’s breathe together. | "Calm down right now!" |
| "It’s okay to feel upset. Let’s find a way to feel better." | "Stop acting like a baby!" |
| "Your feelings are big right now. I'm going to help you." | "You’re being ridiculous!" |
| "Let’s take a break together." | "Go to your room until you’re normal!" |
When in doubt, focus on validating feelings, offering co-regulation, and giving your child a clear pathway to reset their nervous system. Validate your child’s feelings without judgment, offer steady co-regulation through your calm presence, and create a simple, predictable pathway for them to reset their overwhelmed nervous system. In their hardest moments, what they need most is your safe, regulating energy — not correction or control.
Simple Steps to Help a Dysregulated Child Regulate
| Step | Action | Tip |
|---|---|---|
| 1 | Stay Calm | Take deep breaths and steady your own emotions first |
| 2 | Reduce Stimulation | Move to a quieter, softer environment if possible |
| 3 | Soothe, Don’t Lecture | Offer simple, reassuring words and supportive touch |
| 4 | Decompress | Provide water, a snack, or a calming physical connection like a hug |
Co-Regulation and Zoe
At a family gathering, six-year-old Zoe became overwhelmed and melted down when it was time to leave the playground. Recognizing that her brain was in “overdrive” and not capable of reasoning in that moment, her dad didn’t demand explanations or insist she “behave.” Instead, he quietly sat with her in the car, regulating his own breathing and energy to offer her the co-regulation she needed.
Within a few minutes, Zoe climbed into his lap and hugged him tightly, her nervous system calming through his presence. Calm leadership and connection, not correction or punishment, are what truly help soothe a dysregulated ADHD brain.
Did I Cause My Child’s ADHD?
When parents first hear that their child has ADHD, a wave of guilt often follows. You may wonder, “Did I parent wrong? Did I miss something?”
Let’s be very clear: ADHD is not caused by parenting. It is a neurodevelopmental condition rooted in genetics, brain structure, and environmental influences — not your discipline methods, not your routines, and not your love.
Knowing this frees you from blame and allows you to focus on what matters: building strategies that help your child thrive.
ADHD Facts Every Parent Should Know
| Fact | Truth |
|---|---|
| ADHD is a brain-based condition | Parenting didn’t cause it |
| Children with ADHD are not "bad" | Their brains process differently |
| Positive parenting improves outcomes | Guilt holds both of you back |
Remember: It’s not bad parenting — it’s a dysregulated brain.
What Therapy Options Are Best for ADHD (Besides Meds)?
Therapy isn’t just about talking through feelings. For kids with ADHD, the right therapeutic interventions can rewire the brain toward better focus, impulse control, and emotional regulation.
Here are top therapy options supported by research:
| Therapy | Why It Helps |
|---|---|
| Behavioral Therapy | Reinforces positive behaviors through rewards and structure |
| Parent Training Programs | Helps parents support emotional and behavioral regulation |
| Executive Function Coaching | Builds skills in organization, memory, and task management |
| CBT (Cognitive Behavioral Therapy) | Teaches emotional self-awareness and coping strategies |
| Social Skills Groups | Supports peer interaction and emotional problem-solving |

Noah and Homework Meltdowns
At 10 years old, Noah dreaded homework time — and so did his parents. Every afternoon ended in meltdowns filled with tears, yelling, and frustration. Starting assignments, staying organized, and managing his emotions felt impossible.
After months of struggle, Noah’s parents enrolled him in Dr. Roseann’s BrainBehaviorReset™ program. Over 12 weeks, Noah worked on calming his nervous system first through neurofeedback and PEMF therapy, while building skills with executive functioning coaching. He learned how to use visual schedules to break down tasks, brain breaks to reset when frustration spiked, and coping phrases like “I can take a breath” to stay regulated.
The transformation was profound. Noah began approaching homework more independently, asking for help when needed instead of melting down. His teachers reported he was turning in assignments more consistently, and his parents found that evenings were calmer, more connected, and far less stressful.
When you calm the brain first and build the right executive functioning skills, even everyday battles like homework can turn into moments of confidence, independence, and success.
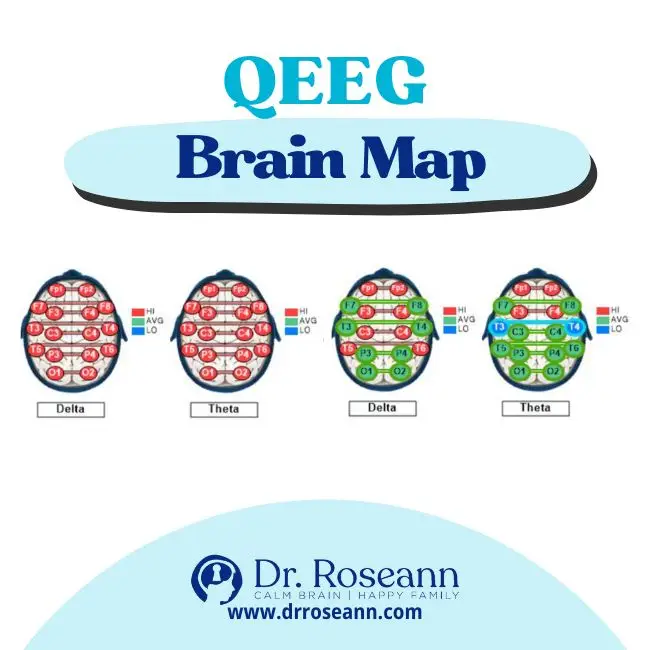
Is Neurofeedback Really Effective for Treating ADHD?
Many parents are curious about neurofeedback — and for good reason. It’s one of the most exciting, research-supported therapies for ADHD today.
Neurofeedback trains the brain to produce healthier brainwave patterns. Instead of simply masking symptoms like medication, it targets the dysregulation at the root of ADHD. Studies show that neurofeedback improves attention, emotional regulation, and executive functioning — often with lasting results.
| Benefits of Neurofeedback |
|---|
| Improves sustained attention |
| Reduces impulsivity |
| Enhances emotional regulation |
| Decreases anxiety symptoms |
| Strengthens brain flexibility and resilience |
The American Academy of Pediatrics rates neurofeedback as a Level 1 “Best Support” intervention for ADHD.
How Long Does it Take to See Improvement with ADHD Treatments?
One of the first questions parents ask is, “How soon will we see changes?”
The honest answer? It depends — on the child, the treatment, and the consistency of support.
Healing a dysregulated brain and building new behavioral and emotional skills isn’t an overnight process. Some treatments, like medication, may bring noticeable changes within days. Others, like brain-based therapies and executive functioning coaching, require time, repetition, and patience to create lasting, meaningful change.
The good news? Consistent, steady action — even small daily steps — leads to real, transformative progress.
Every effort you make to calm the brain, build skills, and foster connection moves your child closer to greater regulation, confidence, and success.
| Treatment | Typical Timeline for Improvement |
|---|---|
| Behavioral Therapy | 1–3 months |
| Neurofeedback | 1–3 months |
| Executive Function Coaching | 3–6 months |
| Nutrition/Supplements | 2 weeks to 3 month |
How Do I Find the Right Treatment Plan for My Child’s Unique Needs?
There’s no one-size-fits-all approach to ADHD. Your child is wonderfully unique, and so should their treatment plan be.
The best plans combine—and the ones that I personally create for my clients include: brain-calming strategies, skill-building supports, and family-centered care.
Here’s how to build the right plan:
- Calm the Nervous System First: Regulation is the foundation. (Think neurofeedback, PEMF, mindfulness.)
- Layer in Targeted Skill-Building: Behavioral therapy, executive functioning coaching, parent training.
- Support the Brain from the Inside Out: Nutritional improvements, supplements, exercise.
- Adjust Over Time: Monitor what works and be flexible. Your child’s needs may shift with growth.
- Trust Your Parental Instincts: You know your child better than anyone else

Why Natural ADHD Treatments are Your Important Next Step
If you’re feeling overwhelmed right now, take a deep breath — you’re exactly where you need to be.
You don’t have to have all the answers today.
You don’t have to do everything perfectly tomorrow.
You just have to keep moving forward.
The fact that you’re here — learning, asking questions, seeking solutions — means you’re already taking powerful action to help your child heal, regulate, and thrive.
Remember:
➡️ Behavior is communication.
➡️ It’s not bad parenting — it’s a dysregulated brain.
➡️ And it’s going to be OK.
Real change doesn’t happen overnight — but it does happen with small, consistent steps that calm the brain, build connection, and strengthen emotional resilience.
You’re not alone in this journey.
And you don’t have to figure it out on your own.
✨ If you’re ready for more guided support, tools, and proven brain-based strategies, explore Dr. Roseann’s resources and programs designed for parents just like you.
Because your child’s bright future is waiting — and it starts with the hope and action you’re taking today.
FAQ: ADHD Treatments
Q: Can ADHD be treated without medication?
A: Absolutely. Behavioral therapies, neurofeedback, nutritional changes, and skill coaching can all make a significant impact.
Q: How long should we try a natural treatment before expecting results?
A: Most brain-based natural treatments (like neurofeedback, PEMF) show improvements within 2–4 months with consistent use.
Q: Will my child eventually grow out of ADHD?
A: Some symptoms may lessen with age, but many people need ongoing coping strategies into adulthood. Early support builds lifelong success.
Q: Is it possible to combine therapies?
A: Yes! In fact, combining brain-based and behavioral supports often gives the best results.
Centers for Disease Control and Prevention. (2020, June 15). Data and Statistics on Children’s Mental Health.
Danielson, M. L., Bitsko, R. H., Ghandour, R. M., Holbrook, J. R., Kogan, M. D., & Blumberg, S. J. (2018). Prevalence of Parent-Reported ADHD Diagnosis and Associated Treatment Among U.S. Children and Adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. https://doi.org/10.1080/15374416.2017.1417860
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
© Roseann-Capanna-Hodge, LLC 2025










