
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!















Brent is a 19 yr-old teen with a history of difficulties with attention, alertness, distractibility, task completion, following directions, impulsiveness, low self-esteem, cannabis use and college failure.
His birth was normal and his history is positive for a fall down the stairs at age three. An “egg on his forehead” was reported and no other known resulting issues were noted.
Difficulties with impulse control, distractibility and work completion were noted in preschool. By the first grade, Brent was brought up to the school Child Study Team (CST) and a support plan was put into place. Some improvements were noted in all areas. By the end of second grade, Brent's difficulty completing work prompted an IEP meeting at the request of his parents. After psychoeducational testing found difficulties with attention switching, distractibility, working memory, and slow processing speed, Brent qualified for special education services as a child with Other Health Impairment due to ADHD.
At the school's suggestion, his parents took Brent to the pediatrician to get support for his ADHD. The pediatrician suggested Concerta for ADHD and play therapy. Brent had some noticeable improvements with focus with Concerta medication but it wasn't until they added play therapy that there were improvements with impulse control.
Brent had generally positive academic success in the third and fourth grades but by the fifth grade, he struggled to keep up with the work and more support in his IEP was added. Socially, even though his impulse control had improved, Brent didn't do well with team sports and gravitated toward playing with the girls at recess. He had a couple of friends though the Boy Scouts but they were on a different team when he entered middle school, so he barely saw them.
During middle school, they changed medication two times and he switched therapists. His mother tried a gluten dairy free diet and cut out most sugar from his diet with marked improvement in focus and behavior but discontinued because, “It was too hard to give Brent a separate diet from the family.”
High school was a rollercoaster with Brent typically doing well the first and third quarter and poorly the second and fourth quarters when he “let his foot off the gas.” With academic modifications, Brent's grades were mostly “B's” so he did well enough to get into college.
Brent struggled with the independent reading, writing papers, and tests in college and was ill pre-prepared to independently manage his school work. He was put on academic probation and begged his parents to remain for the next semester, which they agreed to if he regularly went to the student learning lab. Brent went the first two months and then stopped going and did even worse than the first semester.
Having felt like they exhausted all other options and wanting a good future for their son, Brent's parents decided to seek support and participate in our one-to-one program.
His QEEG Brain Map reflected ADHD brainwave patterning: too many unfocused brain waves (Theta and Delta) and too little focused brain waves (Beta) but it also reflected that he had a frontal head injury.
Since Brent and his family were in a “stuck state,” they traveled to our Connectiuct center and worked with us intensively for five days doing neurofeedback, PEMF/BRT, biofeedback, brain-based exercise, and individual and family psychotherapy. We worked intensively on getting his brain to regulate, breaking Brent's shame-give up pattern, and improving everyone's understanding of ADHD and executive functioning, as well as family communication.
The family committed to changing their diet and walking one to two miles a day. Brent started dietary supplements and shifted from a high carbohydrate diet to a high protein, moderate healthy fats diet.
Brent learned how to use his neurofeedback equipment and then went home with it. He continued neurofeedback more intensively, doing four sessions a week until he got to 20 sessions, where data was collected again and we reviewed his progress. Brent reported slow gradual improvement with his attention and mood but specifically noted that he had a dramatic shift after session 18, which caused him to sleep for more than fifteen hours. Brent explained that a “brain fog lifted” and that he was “way more alert.” He noted that it was easier to walk at night and he was just starting to remember to take his supplements without reminders.
Phase one is focused on neurofeedback, PEMF/BRT, biofeedback, brain-based exercise, and individual and family psychotherapy. We worked intensively on getting his brain to regulate, breaking Brent’s shame-give up pattern, and improving everyone’s understanding of ADHD and executive functioning, as well as family communication.
Phase two focused executive functioning coaching and getting Brent to “see the result” instead of being so overwhelmed and then ashamed. During the second set of sessions, Brent was more engaged and proactive. He benefited from psychoeducation and was looking for ways to increase his focus. Deeper work with Brent and his family on stuck communication patterns continued.
QEEG Brain Map Comparison from QEEG #1 to #3 after 50 sessions of Neurofeedback,
5 sessions of PEMF/BRT and individual and family therapy in our BrainBehaviorReset™ Program.
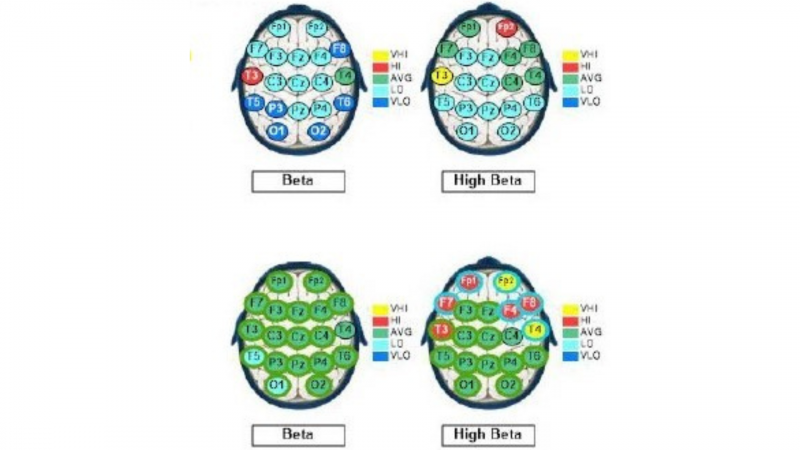
With 50 sessions of neurofeedback, individual and family therapy, dietary changes, supplements and exercise, Brent was able to normalize his focused brain waves (Beta) and reduce his unfocused brain waves (Delta). The frontal region of his brain that reflected head injury resolved.
Behaviorally, changes were noted in Brent’s motivation, task completion at home, independent daily self-care and management of his tasks, and less disagreements at home.
These case studies are a description of the experiences of our clients. We have changed the names and some details to protect their privacy. Each client experience and protocol is unique in our trademarked BrainBehaviorReset™ Program.

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
