OCD (Obsessive-Compulsive Disorder) and ADHD (Attention-Deficit Hyperactive Disorder) are two entirely different conditions. However, children and teens are misdiagnosed to have one condition over the other. Most of it is because these mental health issues have overlapping symptoms.
Many symptoms associated with concentration with attention have very similar effects on children and teens with either one of these conditions. However, the clinical presentation and brain activity of a child or teen with ADHD are very different from one that has OCD.
What is OCD?
A child or teen with OCD exhibits irrational thoughts and fears, also called obsessions, that lead to compulsive behaviors. Compulsions are the behaviors that OCD-affected individuals engage in to get rid of their obsessions or decrease their distress.
Almost everyone has obsessive thoughts and compulsive behaviors at some point in their lives, but that does not mean they have OCD. To be diagnosed with an obsessive-compulsive disorder, one must be unable to function normally daily and these behaviors must occur one more hour a day.
There is a tendency for children and teens with OCD behaviors to display a more inhibited temperament and to avoid situations that they may perceive as harmful or risky. Their mental rituals and intrusive thoughts often keep them from pushing into new situations. Additionally, individuals diagnosed with OCD tend not to act impulsively due to their oversensitivity to the consequences of their actions and worried fearful thoughts.
General OCD Symptoms
All OCD fears and intrusive thoughts are unique but there are some common themes that impact children and teens. OCD intrusive thoughts are rarely logical and can be dark and scary. Children and teens can be quite adept at hiding these internal worries, so parents can be surprised when they are revealed.
Some of the most common OCD obsessions and compulsions children and teens experience are:
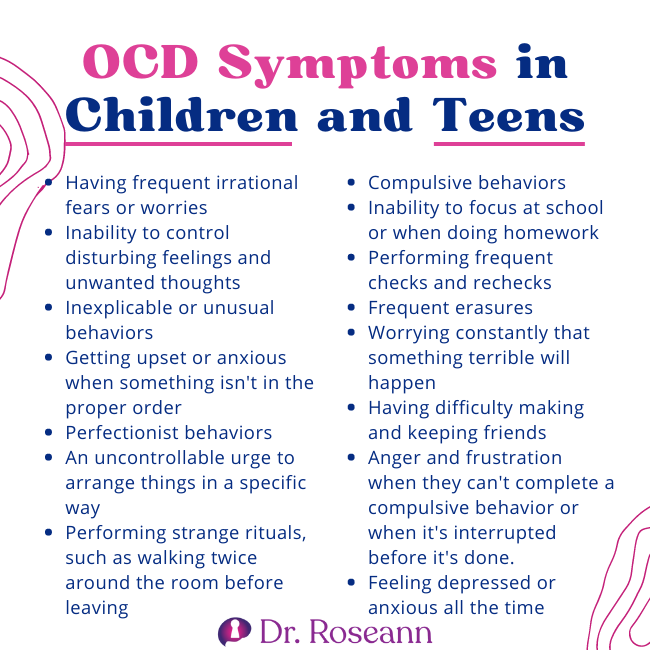
- Having frequent irrational fears or worries
- Inability to control disturbing feelings and unwanted thoughts
- Inexplicable or unusual behaviors
- Getting upset or anxious when something isn't in the proper order
- Perfectionist behaviors
- An uncontrollable urge to arrange things in a specific way
- Performing strange rituals, such as walking twice around the room before leaving
- Compulsive behaviors
- Inability to focus at school or when doing homework
- Performing frequent checks and rechecks
- Frequent erasures
- Worrying constantly that something terrible will happen
- Having difficulty making and keeping friends
- Anger and frustration when they can't complete a compulsive behavior or when it's interrupted before it's done.
- Feeling depressed or anxious all the time
What is ADHD?
ADHD is more than a lack of focus. Children with Attention Deficit Hyperactivity Disorder may have difficulties with hyperactivity and impulsive behavior, sustaining attention, or both. Additionally, they suffer from poor executive functioning, which adversely impacts their academic, social, and personal lives.
There is a misconception that ADHD children cannot focus. But, in reality, they may be hyperfocused when they are interested. Their ability to hyperfocus is due to the stimulation their brain receives when they are excited or interested.
General ADHD Symptoms
There is different types of ADHD, but the hyperactive and impulsive symptoms tend to be more identifiable with OCD. The most common symptoms of hyperactivity are:
- Fidgeting
- Nonstop talking
- Moving constantly
- Impatience
- Talking too loudly and interrupting
- Emotionally charged
- Group activity problems
- inappropriate social behavior
- Problems with friendships
- Having difficulty transitioning
- High error rates
- Avoiding schoolwork
How are OCD and ADHD the Same?
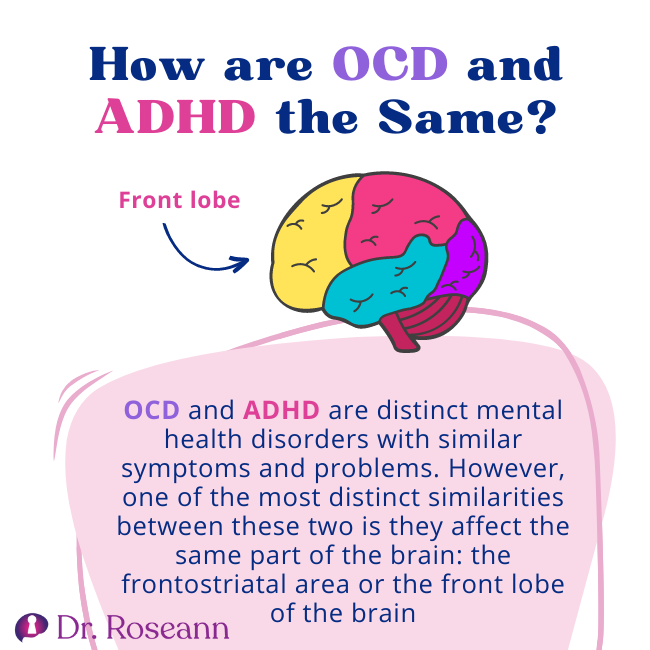
OCD and ADHD are distinct mental health disorders with similar symptoms and problems. However, one of the most distinct similarities between these two is they affect the same part of the brain, particularly the frontostriatal area or the front lobe of the brain.
The biology of OCD and ADHD is that it impacts the frontal lobes or the job management of the brain that helps to organize thinking and behavior. For OCD, it is the orbito-frontostriatal region and the frontoparietal area for ADHD. The deficits in cortical inhibition or disinhibition may facilitate the perseverative, compulsive behaviors seen in OCD patients and also explain the impulsive, inattentive, and disinhibited behavior of ADHD patients (Brem et al., 2014).
Another similarity between children and teens with OCD and ADHD is that they both have difficulty paying attention. ADHD kids with attention issues can't sustain their focus for long. Those with OCD, on the other hand, maybe inattentive because they are too preoccupied with their obsessions and compulsions that they don't have the chance to focus on the things happening around them.
OCD and ADHD can also trigger the major depressive disorder, stress, anger, and anxiety disorders, thus worsening their symptoms. They may also display physical symptoms such as sleep problems and gastrointestinal issues. As a result, children and kids with these conditions may have strained relationships with family and peers.
Similar Symptoms of OCD and ADHD
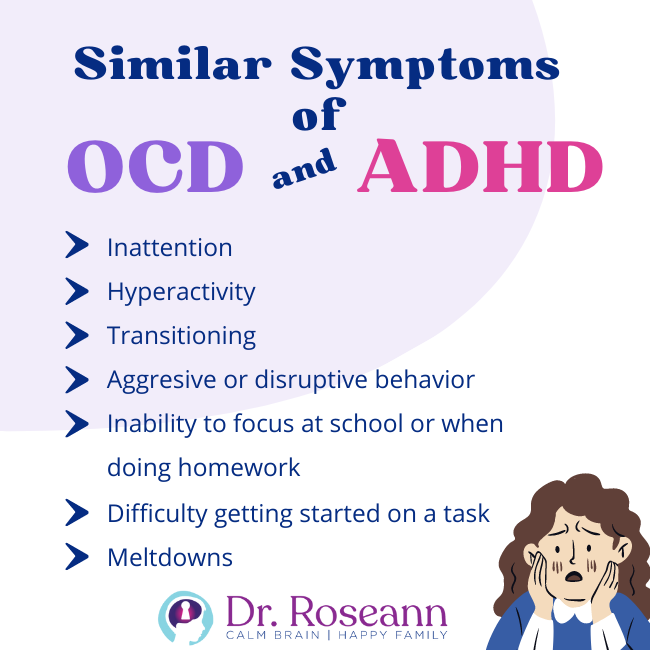
OCD and ADHD are often misdiagnosed because they share several similar symptoms. When you have intrusive thoughts, paying attention is hard because you are locked in a stressful fear loop. Here's a closer look at their similarities:
Inattention
Inattention is one of the most common symptoms of ADHD. It is because an ADHD mind gets distracted by many random thoughts. On the other hand, if a child has OCD, they may exhibit inattention due to their minds getting filled with obsessive thoughts.
Hyperactivity
Hyperactivity is another primary symptom of children with ADHD, and it is commonly characterized by fidgeting and having endless energy running around the room in an effort to disperse anxious energy. For those with OCD, hyperactivity might be exhibited by behaviors such as pacing back and forth, flapping the arms, nail picking, and hair pulling.
Transitioning
A child with ADHD and OCD often has problems transitioning or shifting to another activity. For a kid with ADHD, it's because they are too hyperfocused on doing the task that interests them. For those with OCD, it's because they are intricately working on something to make it look perfect or completing a mental ritual before moving on to another task, which may take a very long time.
Aggressive or disruptive behavior
ADHD children act impulsively, which is why they are regarded as disruptive. It means that they don't necessarily think through the consequences of their actions and act on impulse. On the other hand, those with OCD have the compulsion to do something to address their anxiety or distress. They may become upset and angry when their fear causes emotional dysregulation or they are stopped from completing a ritual.
Inability to focus at school or when doing homework
Children with ADHD tend to lose focus or can't concentrate on school activities that don't interest them because their brains are under-stimulated. They always seem to zone out or daydream instead of doing the task until an adult helps them get back on track. Children with OCD, on the other hand, will do their homework but keep repeating what they started or have frequent erasures. They are slow to or never finish because they feel they must do it perfectly.
Difficulty getting started on a task
Children with ADHD experience problems starting a task because they think it is too complicated or involves many complex steps. They also just may simply be distracted. Children with OCD, on the other hand, will exhibit rigidity. They overfocus on doing the task correctly. Hence, they won't start working on it.
Meltdowns
Meltdowns may happen in children with ADHD when they get frustrated due to failing to accomplish a task or chore assigned to them or wanting to avoid it altogether. Those with OCD experience meltdowns when they are overloaded by fearful thoughts and compulsions that make them feel out of control.
How are ADHD and OCD Different?
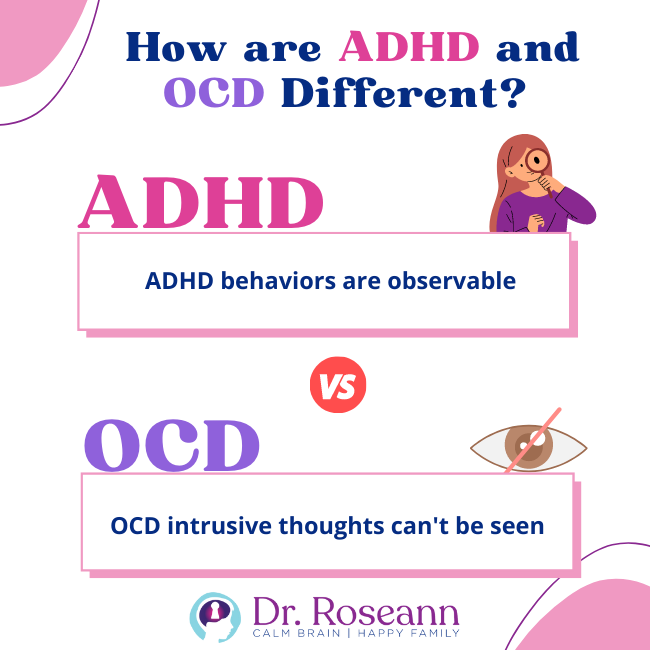
ADHD is largely an externalizing disorder. It means the condition affects how a child or teen relates outwardly to the people around them and their environment. As a result, kids and teens with ADHD may display inattention and disruptive or impulsive behaviors. Even when a child is inattentive, their behaviors can be quite observable.
On the other hand, OCD is a type of internalizing disorder. It means that children and teens with OCD turn inward when responding to anxiety triggered by their environment. Kids and teens with OCD exhibit repetitive obsessive and compulsive thoughts. Their intrusive thoughts can be easily hidden until compulsive behaviors show up.
Can my child have ADHD and OCD?
Yes, ADHD and OCD may be comorbid conditions, meaning a child may have both. For example, one study involving 94 teens and children diagnosed with OCD discovered that 25.5% also have ADHD.
These findings suggest that children with OCD should also get screened for ADHD because some symptoms may be partly due to ADHD. Screening for ADHD helps the child get the right kind of treatment (Masi et al., 2006). Making sure you get an ADHD assessment from a professional who also understands OCD too is important.
Treatment for OCD and ADHD
Pharmacology is not the only route to treat OCD and ADHD. There are natural solutions for OCD and ADHD, particularly brain-based tools such as neurofeedback and PEMF. Treatment options for these disorders may include noninvasive brain regulation techniques, which work to normalize the situational imbalance between cognitive persistence and cognitive flexibility (Colzato et al., 2022).
Neurofeedback helps treat OCD and ADHD by reinforcing the subconscious and teaching the brain to alter its behavior. It trains the brain to produce brain waves that induce concentration, calming the mind and putting it in a focused state. When performed regularly on ADHD kids, it results in increased motivation and focus, as well as reduced impulse control and distractibility.
Neurofeedback helps children with OCD in almost the same way. Children get better control of the intrusive thoughts and sensations that hijack their brains. A recent study shows that neurofeedback can help reduce obsessions and compulsions without using medication or causing harmful side effects (Barzegary et al., 2011).
At our Ridgefield clinic and virtually, we help children and teens with OCD, ADHD, and other mental health conditions. It is critical that your child must get a correct diagnosis early to get a proper treatment plan that truly addresses their condition.
We use natural, science-backed solutions to treat mental health issues to get the brain working optimally without subjecting your child to the toxic side effects of stimulant medications. Aside from neurofeedback brain scans, we also use the gold standard of OCD treatment, exposure response prevention (ERP) combined with PEMF, cognitive behavioral therapy, and nutritional supplementation in order to help improve your child's quality of life and reduce OCD symptoms.
Citations
Barzegary, L., Yaghubi, H., & Rostami, R. (2011). The effect of QEEG- guided neurofeedback treatment in decreasing of OCD symptoms. Procedia – Social and Behavioral Sciences, 30, 2659–2662. https://doi.org/10.1016/j.sbspro.2011.10.519
Brem, S., Grünblatt, E., Drechsler, R., Riederer, P., & Walitza, S. (2014). The neurobiological link between OCD and ADHD. ADHD Attention Deficit and Hyperactivity Disorders, 6(3), 175–202. https://doi.org/10.1007/s12402-014-0146-x
Colzato, L. S., Hommel, B., Zhang, W., Roessner, V., & Beste, C. (2022). The metacontrol hypothesis as diagnostic framework of OCD and ADHD: A dimensional approach based on shared neurobiological vulnerability. Neuroscience and Biobehavioral Reviews, 137, 104677. https://doi.org/10.1016/j.neubiorev.2022.104677
Masi, G., Millepiedi, S., Mucci, M., Bertini, N., Pfanner, C., & Arcangeli, F. (2006). Comorbidity of obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Comprehensive Psychiatry, 47(1), 42–47. https://doi.org/10.1016/j.comppsych.2005.04.008
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.