Estimated reading time: 8 minutes
When ADHD and aggressive behavior collide, it can feel like your child’s outbursts take over the whole household. Shouting, arguing, hitting, even breaking things—these aren’t signs of bad parenting. They’re signs of a dysregulated brain that still needs coaching, tools, and time to find calm.
In this article, you’ll learn why aggression shows up with ADHD. You’ll know what to do in the heat of the moment. And you’ll be able to build daily habits and treatments that reduce explosions over time. Plus, you’ll get 17 practical strategies you can start today.
What Drives Aggression in ADHD?
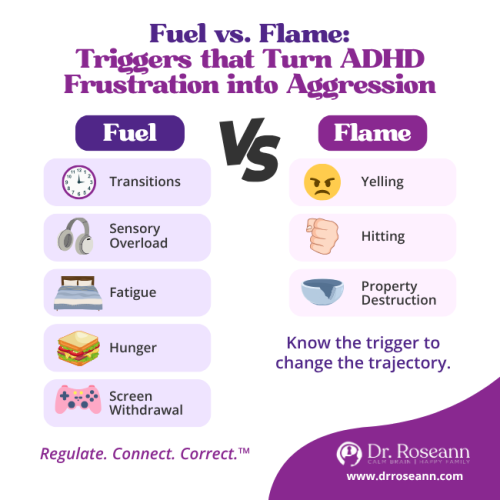
Aggression in ADHD often comes from impulsivity + emotional dysregulation. The brain’s brakes aren’t engaging fast enough when frustration, shame, sensory overload, or boredom spike.
Co-occurring issues like ODD, anxiety, trauma, sleep problems, or learning differences can amplify it. Behavior is communication; your child’s brain is saying, “I’m overwhelmed.”
Spot the Difference
- ADHD-related aggression: fast, impulsive, tied to frustration or transitions.
- ODD-like patterns: arguing with authority figures, chronic refusal, seeking control.
- Anxiety/trauma: aggression follows perceived threat; the child looks fearful more than willful.
Sensory overload: meltdowns after noise, crowds, itchy clothes, or bright lights.
How To Calm Aggression (In The Moment) Without Making It Worse
In the heat of it, regulate → connect → correct. Let’s calm the brain first.
In-the-moment steps (keep it short & neutral):
- Lower your voice + body: Kneel to the side, speak slowly, few words.
- Name and normalize: “Big feelings. I’m here.”
- Offer a regulation cue: Breathe in for 4, out for 6; wall push; stomp then freeze; cold water splash.
- Shrink the demand: “First shoes. Then car.”
- Create safety: Clear siblings, remove breakables; use a pre-taught calm corner.
Parent example:
Riza, mom of a 10-year-old, noticed after-school eruptions. She tried a “no-talk transition”—hug or hand squeeze, snack, 10-minute quiet time—before homework. Explosions dropped within two weeks.
The takeaway: front-load regulation, not lectures.
Quick List: The 17 Ways (at a glance)
- Create predictable routines (visual schedules).
- Use positive reinforcement (praise/points for effort & calm).
- Personal behavior plan (one target at a time).
- Clear rules & consistent, brief consequences.
- Teach self-regulation skills (breathing, wall push, cold water).
- Practice better communication (few words, choices, first-then).
- Daily exercise & movement (outdoors when possible).
- Steady nutrition (protein breakfast; consider omega-3 with your clinician).
- Mindfulness/relaxation habit (2–5 minutes/day).
- Time management & organization (timers, checklists).
- Limit screen time + plan calm transitions.
- Coach social skills (role-play; set up safe peer time).
- Create a safe expression space (calm corner, sensory tools).
- Protect sleep (consistent schedule; tech off 60 min prior).
- Consider natural solutions (QEEG-guided neurofeedback, CALM PEMF®, magnesium with provider guidance).
- Join a support group (reduce isolation; swap strategies).
- Work with professionals (evaluation, parent training, school plan).

Simple Changes At Home That Prevent Blowups
Structure reduces surprises—and surprises light the match.
High-impact home and family-centered tweaks:
- Predictable routines + visual schedules (morning/after-school/bedtime).
- Clear rules and pre-agreed consequences (brief, posted, reviewed).
- Positive reinforcement (catch them being brave/calm/trying).
- Organization & time management supports (timers, checklists, “one-thing baskets”).
- Sensory-friendly environment (noise-reducing headphones, movement breaks, chewy snacks).
Parent example: Miguel, 7, fought tooth-brushing nightly. A first-then card (“First brush 30 sec, then pick the story”) plus a sand timer cuts protests in half.
Lesson: make the task smaller, the success faster.
Do Screens and Video Games Worsen Aggression?
For many kids, yes—especially during transitions or with violent, fast-paced games. The nervous system revs; stopping can feel like slamming the brakes on the highway.
Screen-smart guardrails that actually stick:
- Fixed “on/off” windows (e.g., after homework, never before school/bed).
- Timers + visual countdowns (5-minute + 1-minute warnings).
- Content swap: prefer co-op/non-violent games; avoid M-rated/rapid-reward loops.
- Transition routine: stand, stretch, sip water, 10 slow breaths before the next task.

Parent example:
Aisha’s 12-year-old exploded when Fortnite ended. They switched to co-op building games on weekends only. Then, added a five-minute shutdown routine, and aggression during transitions dropped. Consistency won, not threats.
Natural and Clinical Treatments That Reduce Aggression Over Time
We want skill-building and brain-calming strategies that stick.
Evidence-Informed Options
- Behavioral Parent Training (BPT) teaches parents how to use praise, scaffolding, and set clear limits. It improves parenting outcomes and child behavior in ADHD (Dekkers et al., 2021)
- Omega-3 fatty acids (EPA/DHA) show modest improvements in ADHD symptoms in youths. Aim for diet first and discuss supplements with your provider (Chang et al., 2018).
- Neurofeedback can support attention and self-regulation in some children. Follow protocols with experienced clinicians and integrate with behavioral work (Van Doren et al., 2019).
Other Regulation Builders
- Exercise & movement (daily—walks, martial arts, swimming).
- Sleep (same bedtime/wake time, dark/cool room, tech off 60 min before).
- Nutrition basics (protein at breakfast, steady meals, limit dyes/high-sugar ultra-processed foods).
- Mindfulness & relaxation (paced breathing, progressive muscle relaxation).
- School supports (breaks, movement jobs, reduced workload bursts, calm pass).
As psychologist Russell Barkley often emphasizes, ADHD is a disorder of self-regulation. Skills grow best with scaffolding, structure, and reinforcement, not shame.
What To Do After An Outburst?
After everyone’s calm, keep it brief, specific, and future-focused.
The 3-Minute Repair
- Name the win: “You took space—good choice.”
- Teach the micro-skill: “Next time, fist-press + three breaths when your brother grabs the controller.”
- Practice once (in low stakes).
- Re-enter connection: high-five, short game, or movement break.
When To Seek Professional Help
Seek support if aggression is frequent, dangerous, or escalating. Or if school relationships are suffering.
Ask for:
- A complete evaluation (ADHD, emotional dysregulation, learning, sleep, trauma, defiant disorder/ODD, mood/anxiety).
- A multimodal plan: BPT + school supports; consider nutrition, omega-3, neurofeedback, and—when appropriate—medication decisions with a trusted prescriber.
- Providers who understand co-regulation and regulation-first care.
Moving Forward: Hope and Next Steps
ADHD and aggressive behavior aren’t a life sentence. They’re signals that your child’s brain is overwhelmed. The good news is that when we calm the brain first, build connections, and practice small daily skills, children gain control over their emotions. And families finally breathe easier.
Start simple: choose just two strategies from the list and try them this week. Tiny changes compound into big wins when done consistently.
Remember, it’s not bad parenting, it’s a dysregulated brain. Progress is always possible.
Next Step: Explore the BrainBehaviorReset program to create a personalized plan for your child.
FAQs About ADHD and Aggressive Behavior in Children
How can I tell if it’s “won’t” vs. “can’t”?
Assume “can’t yet” when dysregulation is high. If skills improve with structure, coaching, and breaks, it’s capacity—not attitude.
What do I say when my child is screaming?
Use a few words + safety: “I’m here. Breathe with me. We’re safe.” Save teaching for later.
Are rewards “bribes”?
No. Rewards teach the brain what to repeat. Keep them immediate, small, and tied to effort (not perfection).
Should I remove all screens?
You don’t need to go zero-screen. Predictable limits + calm transitions beat all-or-nothing.
Terminology
- Co-regulation: Your calm nervous system is helping your child’s nervous system settle.
- QEEG: Brain mapping that guides personalized neurofeedback plans.
- Neurofeedback: Training the brain’s activity patterns (via EEG) to improve self-regulation skills.
- ODD (Oppositional Defiant Disorder): A pattern of arguing, refusal, and irritability with authority figures.
- Emotional dysregulation: Difficulty managing strong feelings; common driver of aggression in ADHD.
Citations
Chang, J. P.-C., Su, K.-P., Mondelli, V., & Pariante, C. M. (2018). Omega-3 polyunsaturated fatty acids in youths with attention deficit hyperactivity disorder: A systematic review and meta-analysis of clinical trials and biological studies. Neuropsychopharmacology, 43(3), 534–545. https://www.nature.com/articles/npp2017160 Nature
Dekkers, T. J., Hornstra, R., van der Oord, S., Luman, M., Hoekstra, P. J., Groenman, A. P., & van den Hoofdakker, B. J. (2022). Meta-analysis: Which components of parent training work for children with attention-deficit/hyperactivity disorder? Journal of the American Academy of Child & Adolescent Psychiatry, 61(4), 478-494. https://doi.org/10.1016/j.jaac.2021.06.015
Van Doren, J., Arns, M., Heinrich, H., Vollebregt, M. A., Strehl, U., & Loo, S. K. (2019). Sustained effects of neurofeedback in ADHD: A systematic review and meta-analysis. European Child & Adolescent Psychiatry, 28(3), 293–305. https://doi.org/10.1007/s00787-018-1121-4
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge










