Estimated reading time: 12 minutes
You watch your child fidget, worry, or freeze — and you wonder, is it ADHD or anxiety?
These two conditions can look almost identical on the surface, but they come from different places in the brain.
A child who seems distracted may actually be anxious, and one who can’t start a task might be overwhelmed, not inattentive.
Understanding the difference is key. When we know what’s driving the behavior, we can calm the brain first, respond with empathy, and choose the right supports to help our kids focus, cope, and thrive.
Why Do Parents (Even Pros) Confuse ADHD and Anxiety?
On the surface, both can look the same. These are distractibility, meltdowns, school resistance, irritability, and sleep issues. But the why behind those behaviors is different:
- Anxiety pulls attention into “what if…” loops, leading to avoidance, freeze, or perfectionism.
- ADHD disrupts executive functions (planning, working memory, inhibition). Kids know what to do but can’t do it consistently—especially for boring or complex tasks.
- When both co-occur, anxiety magnifies ADHD challenges (and vice versa). This creates a cycle that erodes confidence and family calm.
Parent Story:
At school, Maya (11 yrs old) rarely finished classwork. Teachers suspected ADHD. At home, she rewrote assignments “to make them perfect” and panicked about tiny mistakes.
Once we targeted her worry loops with predictable routines and calming tools, her productivity rose. A calm brain can focus.

How Brain Science Separates Anxiety From ADHD in Children
Great evaluations don’t just tally symptoms. They examine the nervous system and executive functions. Here’s what research tells us:
- Kids with ADHD struggle more than anxious peers to stop automatic responses when working memory demands increase. This shows a core performance problem, not a lack of motivation (Kofler et al., 2024).
- Anxious children can often hold information but get attention hijacked by threat—“Did I mess up?” This looks like inattention, yet stems from fear processing (Michelini et al., 2014).
“ADHD is a disorder of performance—of doing what you know rather than knowing what to do.” — Russell A. Barkley, PhD
“ADHD reflects impaired executive function—the brain’s management system—not a lack of effort.” — Thomas E. Brown, PhD
Clinician tip: If attention returns after calming, anxiety may be primary. If disorganization and inhibition problems persist even when calm, ADHD likely needs direct support.
Everyday Patterns That Reveal Truth
Real life offers the best clues. Notice consistent patterns:
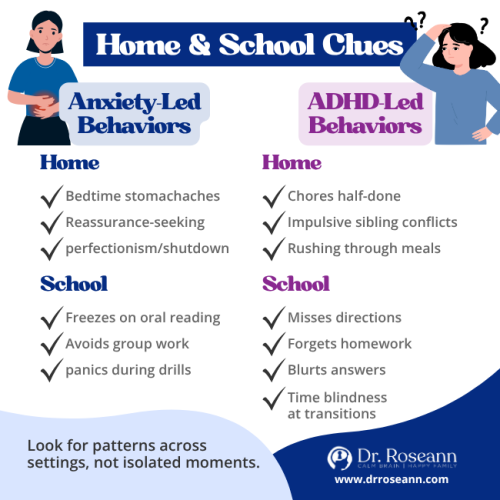
School Patterns
- Anxiety-led: Freezes on oral reading; avoids group work; panics during fire drills.
- ADHD-led: Misses multi-step directions; blurts; loses materials; time blindness at transitions.
Home Patterns
- Anxiety-led: Night-before stomachaches; reassurance-seeking (“Are you sure you’ll pick me up?”); perfectionism leading to shutdown.
- ADHD-led: Chores started but were half-finished; impulsive sibling conflicts; fast-talking/rushing through tasks.
Parent Story
Jordan, a dad of a 13-year-old once shared, “My son could map out a perfect homework plan — but he’d never follow through. He’d get stuck before even starting.”
Once they introduced timers, a visual checklist, and a quick 15-minute movement break before sitting down, everything shifted. The routine gave his son a clear path to begin, helped his brain settle, and turned planning into real progress.
Takeaway:
External structure bridges the gap between knowing and doing.
Daily-Life Differences
| Situation | More Anxiety-Led | More ADHD-Led |
|---|---|---|
| Starting homework | Procrastinates from worry about mistakes | Starts quickly but veers off or forgets steps |
| Group tasks | Avoids, fears judgment | Interrupts, misses cues |
| After calming | Focus improves | Disorganization persists |
Simple, 7-Day Plan That Works
I teach Regulation First Parenting™: Regulate → Connect → Correct.
Because you can’t teach a dysregulated brain, start small and stack wins.
Day 1–2: Regulate the Body
- 3 minutes of belly breathing before homework and bedtime.
- 10–20 minutes of movement (walk, trampoline, dance) after school. Regular exercise supports attention and emotion regulation in ADHD (Sun et al., 2022).
Day 3–4: Connect to Safety
- Validate the feeling: “I can see your brain is going fast. Let’s get it calm together.”
- Role-play one stressful scenario (asking a teacher for help; starting math) and rehearse one coping line.
Day 5–7: Correct With Structure
- Chunk tasks into 15–20 minute blocks; use a visual checklist.
- Externalize time with a visual timer. Praise the effort and completion of each chunk.
- For anxiety, set a micro-exposure goal (e.g., raise a hand once). For ADHD, add a 1-minute reset between chunks (water, stretch).
Skills grow in calm brains. Regulation opens the door to learning.
When and How to Get An Evaluation
Signals it’s time:
- School reports ongoing inattention/avoidance across subjects
- Daily worry or physical anxiety symptoms (stomachaches, headaches)
- Home routines remain hard despite consistent structure
Who to see:
- Pediatric neuropsychologist (comprehensive cognitive/EF testing)
- Clinical psychologist or psychiatrist (diagnosis, treatment planning)
- Consider QEEG and neurofeedback as part of a broader plan—not as stand-alone fixes.
What to expect:
- History + rating scales from parents/teachers
- Cognitive tests for working memory and inhibition (helpful in teasing apart anxiety vs ADHD)
Which treatments actually calm the brain first?
Every brain is unique. We stack supports instead of swapping one for another:
- Neurofeedback + CBT: retrains brainwave patterns and reframes worry; excellent combo for co-occurring anxiety/ADHD.
- Lifestyle pillars: sleep, nutrition, movement, gentle detox supports—your foundation for regulation. Evidence shows exercise benefits attention and executive skills in ADHD (Sun et al., 2022) and helps mood regulation, too.
- School supports: movement passes, written directions, chunking, extended time, and quiet testing space.
- Medication: often helpful—best when layered on top of regulation strategies.
Parent Story
Ellie (9 yrs old) panicked before school and shut down under surprise changes (fire drills, schedule shifts). After neurofeedback, CBT, and predictable routines, meltdowns eased and attention improved. Her mom said, “We finally had a roadmap.”
Takeaway:
Calm the nervous system, and the right strategies finally “stick.”

How To Partner With Teachers
Keep it simple and collaborative:
Share 3 Essentials on One Page
- Triggers (transitions, noise)
- Tools that help (noise-reducing headphones, movement pass, written directions)
- One priority goal for the month
Teacher-Friendly Scripts
- “When transitions sneak up, a 2-minute warning helps Jordan shift.”
- “He does better with written steps and a visual timer—we’re using the same at home.”
Pro tip: Celebrate tiny gains (one raised hand, one finished chunk). That builds self-efficacy and reduces avoidance.
Your Calm-First Roadmap Forward
When it comes to anxiety vs ADHD, what looks like defiance is usually a dysregulated brain asking for safety. Remember: Regulate → Connect → Correct.™
Pick one calming practice this week—like belly breathing before homework or a short family walk. Notice patterns, and if struggles continue across settings, consider a thoughtful evaluation.
Most importantly: your child isn’t broken. With the proper support, their brain can find calm, and your family can find hope.
Next Step: Download our ADHD Parent Kit, a step-by-step roadmap to help your child focus and succeed, without medication.
FAQs
Can anxiety be mistaken for ADHD?
Absolutely. Worry can look like distractibility or avoidance. That’s why assessing working memory and inhibition (not just symptoms) matters (Kofler et al., 2024).
Which should we treat first—anxiety or ADHD?
Calm the brain first. Regulation makes every other tool work better. Often, reducing anxiety improves attention, and EF helps confidence rebound.
Does exercise really help kids with ADHD and anxiety?
Yes. Meta-analyses show exercise improves attention and executive function in ADHD and supports mood regulation (Sun et al., 2022; Song et al., 2024).
What’s one quick change we can make at home?
Add a 10-minute movement break and 3 minutes of belly breathing before homework, then use a 3-step checklist with a timer.
Terminology
- Executive function (EF): The brain’s “manager”—planning, organizing, starting/finishing tasks.
- Working memory: Holding info in mind while you do something else (e.g., directions while packing).
- Inhibitory control: The brain’s “pause button.”
- Co-regulation: Your calm helps your child’s calm.
- Dysregulation: Nervous system stuck in fight/flight/freeze; learning and behavior suffer until calm returns.
- Time blindness: Difficulty sensing how long things take; common in ADHD.
Citations
Kofler, M. J., Groves, N. B., Chan, E. S. M., Marsh, C. L., Cole, A. M., Gaye, F. R., Cibrian, E. A., Tatsuki, M. R., & Singh, L. J. (2024). Working memory and inhibitory control deficits in children with ADHD: An experimental evaluation of competing model predictions. Frontiers in Psychiatry, 15, 1277583. https://doi.org/10.3389/fpsyt.2024.1277583
Michelini, G., Eley, T. C., Gregory, A. M., & McAdams, T. A. (2014). Aetiological overlap between anxiety and attention deficit hyperactivity symptom dimensions in adolescence. Journal of Child Psychology and Psychiatry, 56(4), 423–431. https://doi.org/10.1111/jcpp.12318
Sun, W., Yu, M., & Zhou, X. (2022). Effects of physical exercise on attention deficit and other major symptoms in children with ADHD: A meta-analysis. Psychiatry Research, 311, 114509. https://doi.org/10.1016/j.psychres.2022.114509
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge











