ADHD diagnosis can feel overwhelming, but getting it right is the key to helping your child calm their brain and thrive.
When your child struggles with focus, impulsivity, or daily meltdowns, it’s natural to wonder. Is this ADHD—or something else? The process of an ADHD diagnosis in 2025 has moved far beyond rushed office visits and checklists. Parents deserve clarity, not confusion.
In this guide, you’ll learn how ADHD is diagnosed today—from DSM-5 criteria to multi-source evaluations and QEEG brain mapping. These tools will help you make informed choices and build a hopeful plan forward.
Why Getting the Right ADHD Diagnosis Matters
An accurate ADHD diagnosis is the foundation for any treatment plan. Yet research shows that up to half of children first labeled with ADHD actually have another condition driving their struggles.
“ADHD is a clinical diagnosis that requires evidence across multiple settings—symptoms at school alone aren’t enough,” explains Dr. Samuele Cortese, professor of child psychiatry (Cortese et al., 2020).
When misdiagnosed, kids may be medicated unnecessarily. Or they may miss interventions that address the true cause. When diagnosed correctly, families gain a roadmap for calm and progress.

Who Can Diagnose ADHD—and Who Shouldn’t
Pediatricians sometimes diagnose ADHD, but they are generalists. ADHD is complex, and families benefit from specialists who collect data from multiple sources:
- Child psychologists → complete ADHD evaluations, therapy, and parent coaching
- Psychiatrists → medical diagnosis, medication if appropriate
- Neurologists → rule out seizures, concussions, or other neurological factors
Red flag: If a provider gives an ADHD diagnosis after only a short chat, without gathering teacher input or testing.
Parent story:
Christine, mom of a 9-year-old, was told her son had ADHD after a 20-minute visit. Later, a psychologist uncovered untreated anxiety and poor sleep as the real drivers. With the right plan, his focus and confidence finally grew.
What Happens During an ADHD Clinical Intake?
A true clinical intake typically lasts 60–90 minutes and provides a comprehensive picture. Clinicians gather:
- Family and birth history
- Developmental milestones
- Medical history (including sleep and nutrition)
- Emotional and behavioral patterns
- Teacher observations and school performance
- Parent concerns, strengths, and stressors
Key takeaway: Intake should clarify whether issues reflect true ADHD or nervous system dysregulation. It should also identify if the problem is an environmental mismatch, like the wrong classroom fit.
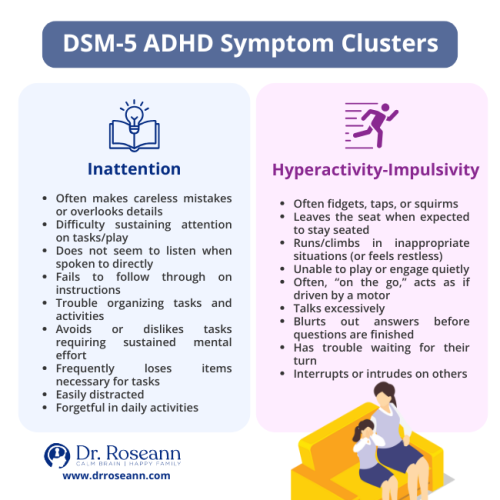
DSM-5, Decoded: What Counts for an ADHD Diagnosis
The DSM-5 ADHD criteria guide every evaluation:
- Symptoms begin before age 12
- Persist for at least 6 months
- Appear in two or more settings (home, school, activities)
- Cause impairment in daily functioning
ADHD subtypes/presentations:
- Predominantly Inattentive
- Predominantly Hyperactive-Impulsive
- Combined presentation
“To make a diagnosis of ADHD, the clinician should confirm DSM-5 criteria are met using information from parents, teachers, and other sources,” stresses Wolraich et al. (2019) in the American Academy of Pediatrics guideline.
Conditions That Can Look Like ADHD
Here’s the challenge: ADHD shares symptoms with many other conditions.
Possible ADHD “look-alikes”:
- Anxiety, depression, OCD, PTSD/trauma
- Learning disabilities (dyslexia, dysgraphia), autism spectrum disorder
- Sleep problems, nutrient deficiencies, thyroid issues
- Concussions, Lyme, PANS/PANDAS
Sometimes, it isn’t clinical at all—it’s a stressful classroom or inappropriate schoolwork.
Parent story: Miguel, age 12, was medicated for ADHD after failing math. But a deeper workup revealed post-concussion slowing and sleep apnea. Once treated, his grades and attention improved dramatically.
Testing That Helps (and What Can Mislead)
A thorough ADHD assessment uses multiple tools:
Helpful:
- DSM-5–based rating scales (parents/teachers)
- Direct tests of attention and executive function
- Psychoeducational testing if academics are impacted
Misleading if used alone:
- Checklists without context
- Quick online screens
- Any tool used without history or observation
“Rating scales help gather observations, but they should never be the sole basis of an ADHD diagnosis,” notes Dr. C. Keith Conners, ADHD researcher (Arns, Conners, & Kraemer, 2013).

QEEG Brain Mapping: What It Can—and Can’t—Tell You
A QEEG (Quantitative EEG) records brainwaves and compares them to healthy databases. In ADHD, it often shows:
- Excess theta (“daydreamer”) waves
- Too few beta (“focus”) waves
- Dysregulation in the frontal lobes (attention + impulse control)
“QEEG provides objective biomarkers that can improve diagnostic accuracy, particularly in differentiating ADHD from other conditions,” highlights Dr. Martijn Arns, a leading ADHD researcher (Arns et al., 2013).
Still, the American Academy of Neurology cautions: “EEG-based ratios are not sufficiently accurate to stand alone as an ADHD diagnostic tool” (Gloss et al., 2016).
Parent story: Sara, mom of a 14-year-old, had years of conflicting labels. A QEEG revealed frontal under-arousal. Guided by neurofeedback plus therapy, Sara finally saw consistent focus and calmer moods.
What to Do Next: A Regulation-First Plan That Works
A solid ADHD diagnosis should lead to a tailored plan—not a one-size-fits-all checklist.
What works best:
- Brain-based tools: QEEG-guided neurofeedback, CALM PEMF®
- Lifestyle supports: better sleep, nutrition, daily movement
- Therapy supports: CBT, occupational therapy, parent coaching
- School accommodations: IEP or 504 plans
Key truth: Regulate → Connect → Correct™. You calm the brain first, then connection and learning follow.
Finding Hope After an ADHD Diagnosis
Getting an ADHD diagnosis may feel like a maze. But it can become a roadmap for healing when done thoroughly. Remember: It’s not bad parenting—it’s a dysregulated brain.
Behavior is communication. Calm the brain first, and everything else follows. Explore the BrainBehaviorReset® Program for science-backed, wraparound support.
FAQs About ADHD Diagnosis
How long does ADHD testing take?
Basic screenings take 1–2 hours. Comprehensive testing may span multiple sessions.
Can ADHD be misdiagnosed?
Yes. Anxiety, trauma, learning issues, and poor sleep can all mimic ADHD. That’s why multi-source evaluation is critical.
Is there a single medical test for ADHD?
No. There is no single test. ADHD diagnosis is clinical, using DSM-5, history, teacher/parent reports, and sometimes QEEG.
Is brain mapping safe for kids?
Yes. QEEG is painless and non-invasive. It measures electrical activity at the scalp.
Terminology
- DSM-5 ADHD criteria: The official symptom checklist for ADHD.
- Executive functioning: Planning, organizing, working memory, and impulse control.
- QEEG brain map: Brainwave analysis tool—helpful for clarity, not a stand-alone test.
- ADHD subtypes: Inattentive, Hyperactive-Impulsive, or Combined.
Citations
Arns, M., Conners, C. K., & Kraemer, H. C. (2013). A decade of EEG Theta/Beta Ratio research in ADHD: A meta-analysis. Journal of Attention Disorders, 17(5), 374–383. https://doi.org/10.1177/1087054712460087
Cortese, S., Coghill, D., & Santosh, P. (2020). Practitioner review: Current best practice in managing adverse events during treatment with ADHD medications. Journal of Child Psychology and Psychiatry, 61(1), 3–20. https://doi.org/10.1111/jcpp.13118
Wolraich, M. L., Hagan, J. F., Allan, C., Chan, E., Davison, D., Earls, M., … Zurhellen, W. (2019). Clinical practice guideline for ADHD diagnosis, evaluation, and treatment. Pediatrics, 144(4), e20192528. https://doi.org/10.1542/peds.2019-2528
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge











