Estimated reading time: 7 minutes
Finding the right ADHD and OCD treatment can feel overwhelming. Your child’s brain is racing with intrusive thoughts while darting from one distraction to the next.
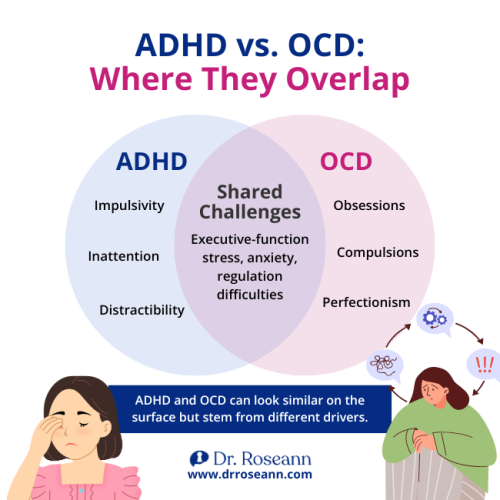
Parenting a child with both ADHD and OCD can feel like navigating two different worlds. One is filled with impulsivity and inattention, while the other is ruled by perfectionism and relentless worries. The clash of these conditions often leaves families exhausted, confused, and searching for answers.
Here’s the good news: behavior isn’t the enemy—it’s communication. Once we calm the brain and address the nervous system first, kids can learn, heal, and thrive.
In this article, you’ll learn how ADHD and OCD overlap and why diagnosis can be tricky. You’ll also discover which treatments are backed by science and the daily steps that bring more calm and hope into your home.
What Makes ADHD and OCD Show Up Together in Kids?
ADHD and OCD are different conditions, but they co-occur more than most parents realize. Studies report meaningful overlap. And when both are present from childhood, symptoms are usually more severe and persistent. So, a thorough evaluation is crucial (Cabarkapa et al., 2019).
Key Takeaways:
- Comorbidity is common and can worsen overall functioning.
Treating only one condition often isn’t enough—plans must address both.
How to Tell What’s ADHD, OCD, and Dysregulation
Think like a detective: behavior is communication. ADHD brings difficulty with attention and executive function. OCD brings intrusive thoughts and rituals that lower anxiety. Dysregulation is the nervous system being too revved up (or too shut down) to cope.
Try this quick sort
- Likely ADHD: can’t start/finish, forgetful, distracted across situations.
- Likely OCD: has to do things “just right” (checking, erasing, washing) to feel safe.
- Dysregulation overlay: big emotions, shutdowns, or sensory overload that amplify both.
Parent story:
Emma, a middle-schooler, jumped from assignment to assignment (ADHD) yet erased and rewrote until it felt “perfect” (OCD). That combo left her stuck and overwhelmed. Our first step wasn’t more willpower—it was regulating her nervous system, so focus and flexibility could return.
What To Stabilize First So Behavior Change Can Stick?
Before we correct behavior, we Regulate → Connect → Correct. When your nervous system is calm, your child’s brain borrows that calm (co-regulation). You aren’t failing—strategies don’t work until the brain is calm.
Stabilizers that help right away
- Rhythm + routine: predictable wake/sleep, meals, and homework rhythm
- Micro-regulators: movement breaks, breath (4-7-8), sensory input (chewy, weighted lap)
- Connection scripts: “I’m here. Your brain feels unsafe. Let’s breathe together.”
“ADHD is not a disorder of knowing what to do; it’s a disorder of doing what you know.” — Russell A. Barkley, PhD

Therapies Proven To Help in ADHD and OCD Treatment
For OCD, CBT with Exposure and Response Prevention (ERP) is strongly supported, including pediatric trials. It reduces symptoms and changes brain activation patterns (Reid et al., 2021; AAP Pediatrics review, 2025).
The AAP also defines ERP as gradually facing obsessions while resisting rituals—clear, coachable steps for families.
For ADHD, evidence supports behavioral parent training, school supports, and (when needed) medication, with benefits and side effects weighed carefully in shared decision-making (AAP, 2024).
Combining Care Safely
- OCD first, then ADHD: Many clinicians stabilize OCD with ERP ± SSRI, then layer ADHD supports (coaching, school plans, possible stimulant) to reduce ritual-driven interference.
- Watch interactions: Some stimulants can spike anxiety for certain kids; close monitoring and sequencing matter.
- Team up: Therapist + prescriber + school + parent = faster progress.
What Treatment Looks Like Day to Day
Make it visual and tiny. Kids with ADHD + OCD do best with clear visuals and micro-steps that lower anxiety and increase follow-through.
| Time | Routine |
| AM | 5-minute stretch → breakfast protein → 1 “must-do” task card |
| After School | Snack → 10-minute movement → ERP homework → reward |
| PM | Screens off → 4-7-8 breath → lights down |
How ADHD Symptoms Change OCD Rituals (and Vice-Versa)
When ADHD and OCD coexist, they can amplify each other:
- Obsessive thinking: ADHD distractibility meets OCD fixation → hyper-focus on worries, avoidance of tasks.
- Impulsivity → more rituals: Quick, repetitive checking or washing increases anxiety cycle.
- Task paralysis: ADHD under-initiation + OCD perfectionism = late nights, tears, and do-overs.
- Emotion storms: Executive-function strain + need for control makes blow-ups more likely.
Parent story:
Jake, in our BrainBehaviorReset® program, was sensory-sensitive (ADHD) and control-seeking (OCD). With neurofeedback, ERP, PEMF, mindfulness, and structured routines, he learned to regulate his brain and then loosen rituals. Daily life got calmer and more focused.
When to Consider Brain-Based Tools Like QEEG or Neurofeedback
QEEG brain mapping can reveal attention-network patterns typical in ADHD (e.g., theta-beta differences), helping personalize care (Cells review, 2025). Evidence is growing, but QEEG complements, not replaces, clinical diagnosis.
Neurofeedback shows promising—but still mixed—results for OCD. Systematic reviews note small trials and heterogeneity. It may help some kids when paired with ERP and emotion regulation routines.
Families should discuss expectations and quality of protocols with a clinician (Systematic review/meta-analysis, 2018–2019).
Plain-Speak Guide
- Consider QEEG when the diagnosis is muddy or ADHD meds aren’t tolerated.
- Consider neurofeedback as an add-on after you’ve established ERP and daily regulators.
How To Partner With School?
You can’t teach a dysregulated brain. Ask for support that lowers cognitive load and anxiety:
School supports that help
- Movement breaks, alternative seating, chunked assignments
- Clear ERP collaboration (nurses/counselors looped in)
- Executive-function scaffolds: visual checklists, timers, 1-thing-at-a-time directions
Script to start the meeting
“My child has ADHD and OCD. We’re working on ERP and regulation at home. Can we create a plan that reduces triggers and uses small, consistent steps?”
Finding Hope and Next Steps for Your Child
When ADHD and OCD appear together, the path forward can feel complicated. But it doesn’t have to be.
The most effective ADHD and OCD treatment begins with calming the brain. Build a connection, and then correct behavior through small, consistent steps.
Start with daily regulators and ERP, layer in ADHD supports. And consider brain-based tools when needed.
Your Next Step Forward: Explore The BrainBehaviorReset® program, a science-backed option tailored to your child.
You are not alone—and it’s going to be OK.
FAQs
How do we prioritize what to treat first?
Stabilize regulation and safety, then target the most impairing symptoms. Many teams start ERP (± SSRI) first to reduce rituals, then layer ADHD supports. (AAP Pediatrics, 2025)
Will stimulants make OCD worse?
Sometimes stimulants can intensify anxiety; sometimes they don’t. That’s why sequencing and close monitoring matter. Your team should adjust in small, data-driven steps.
Is ERP too scary for kids?
ERP is gradual and collaborative. Kids build wins in tiny steps. Meta-analyses support ERP for youth OCD when delivered well (Reid et al., 2021).
Can diet, movement, and sleep really help?
Yes—lifestyle regulators lower allostatic load, so therapy sticks. Think predictable sleep, protein at breakfast, and daily movement to smooth attention and mood.
Terminology
- ERP: Step-by-step practice facing fears while not doing rituals.
- Executive function: Brain skills for planning, starting, shifting, and finishing.
- Co-regulation: Your calm helps your child’s nervous system settle.
- QEEG: Brainwave mapping that can guide pediatric ADHD treatment choices.
- Dysregulation: A nervous system that’s over- or under-activated—not “bad behavior.”
Citations
Cabarkapa, S., King, J. A., Dowling, N., & Ng, C. H. (2019). Co-Morbid Obsessive–Compulsive Disorder and Attention Deficit Hyperactivity Disorder: Neurobiological commonalities and treatment implications. Frontiers in Psychiatry, 10, 557. https://doi.org/10.3389/fpsyt.2019.00557 Frontiers
American Academy of Pediatrics. (2025). Treatment of Obsessive-Compulsive Disorder in Children and Youth: A Systematic Review. Pediatrics, 155(3), e2024068992. https://publications.aap.org/pediatrics/article/155/3/e2024068992/200215
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies from patient to patient and condition to condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge










