Estimated reading time: 8 minutes
When your child experiences a sudden, dramatic shift in their behavior and personality, it can be incredibly unsettling. This abrupt change, often described as a child "turning into a different person overnight," is the hallmark of PANDAS: Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections.
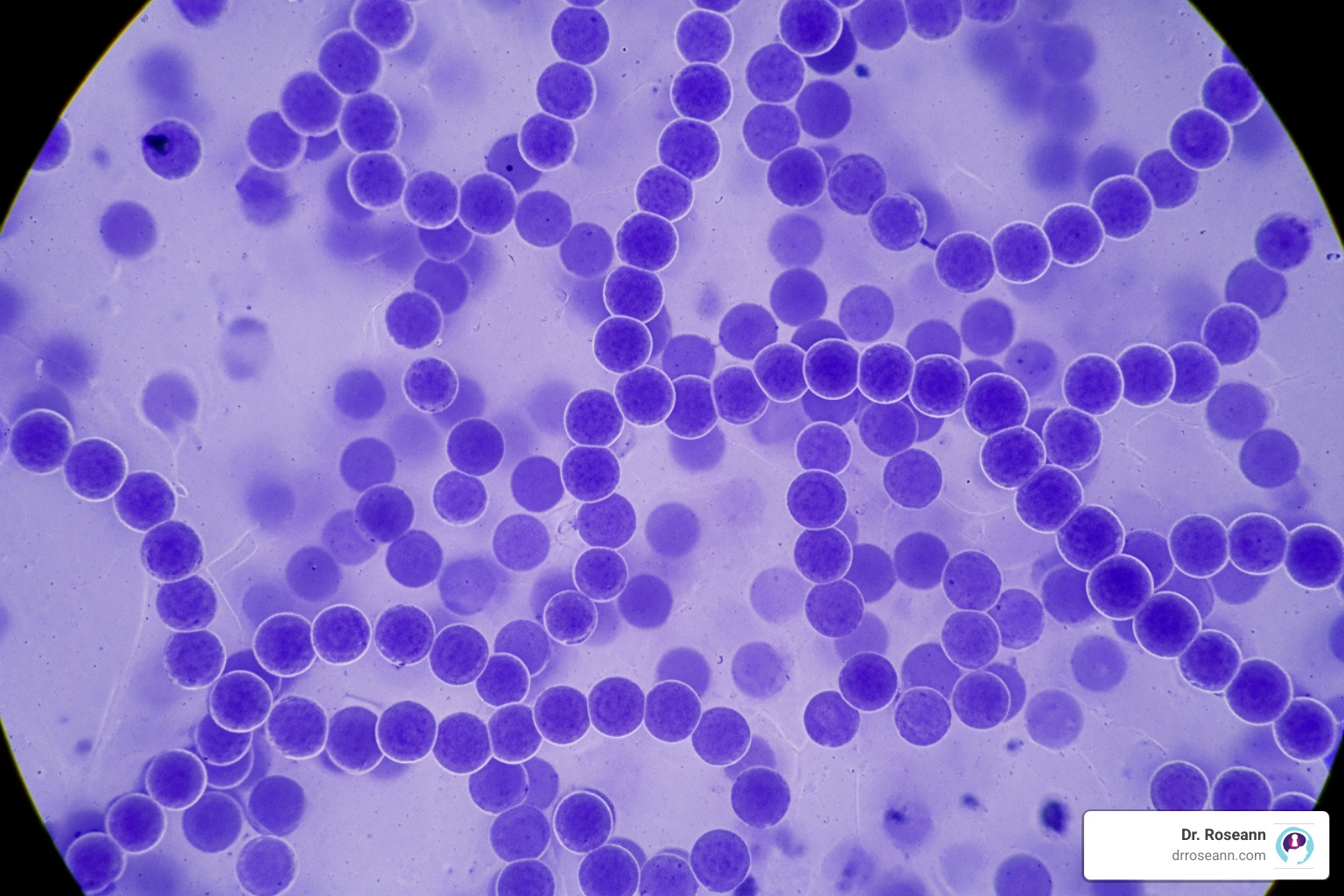
PANDAS is a condition where a Group A Strep infection (like strep throat) triggers an autoimmune reaction. The immune system mistakenly attacks healthy brain cells, particularly in the basal ganglia, leading to a sudden onset of neuropsychiatric symptoms. While considered rare, its impact is profound.
Key signs of PANDAS include:
- Sudden, dramatic onset of obsessive-compulsive disorder (OCD) or tics.
- Symptoms appearing between ages 3 and puberty.
- An episodic course where symptoms flare and recede, often with illness.
- Neurological issues like motor changes, sensory sensitivities, sleep disturbances, and a sudden decline in handwriting.
You're not alone. PANDAS often mimics other conditions like ADHD or primary OCD, leading to misdiagnosis. I've spent decades helping families steer PANDAS diagnosis and treatment. My science-backed approach focuses on calming the brain's inflammatory response first, so children can heal and return to being themselves.

Understanding the intricate process of PANDAS diagnosis is crucial for parents seeking answers. It’s a journey that requires careful observation and thorough medical evaluation. Our goal is to empower you with the knowledge needed to advocate for your child and find the right path to healing.
The Comprehensive PANDAS Diagnosis Process
I've been working with families facing PANDAS diagnosis for decades, and I can tell you that one of the most challenging parts of this journey is that there's no single test that says definitively, "Yes, this is PANDAS." Instead, think of it as detective work—we're piecing together your child's medical history, their symptoms, lab results, and the timeline of when everything changed. It's a clinical puzzle, and your observations as a parent are one of the most valuable pieces.
The PANDAS diagnosis process involves careful clinical evaluation, a thorough review of your child's medical and family history, and specific laboratory tests. But most importantly, it requires a healthcare provider who truly understands these neuroimmune conditions and knows what to look for. Let's walk through each step together.
Recognizing the Sudden Onset: PANDAS Symptoms Checklist
Here's what makes PANDAS so distinctive: symptoms appear almost overnight. Not a slow decline, but an abrupt, dramatic onset or sudden worsening of neuropsychiatric symptoms—parents often say it’s like someone flipped a switch. The course is often episodic—spikes, remissions, then recurrences with new infections.
As my patient Dylan (not his real name), 7, showed: after strep, OCD rituals and tics erupted in a day, eased, then flared again.

Obsessive-compulsive behaviors and motor or vocal tics are at the core of PANDAS. These are new or suddenly intensified intrusive thoughts, repetitive behaviors, or involuntary movements and sounds. What catches many parents off guard is the severe separation anxiety that seems to come out of nowhere, along with dramatic mood swings, irritability, and aggression that are completely out of character.
Many parents first notice something's wrong at school. There's often a sudden deterioration in academic performance, difficulty concentrating, or a sudden decline in fine motor skills, like handwriting becoming nearly illegible overnight. Other common signs include sleep problems, new sensory sensitivities to light, sound, or touch, and urinary frequency or a return to bedwetting.
"Behavior is communication." When your child exhibits these sudden changes, their brain is trying to tell you something. We need to investigate the underlying medical cause.
To formally consider a PANDAS diagnosis, providers look for five distinct criteria from the National Institute of Mental Health:
- Presence of Obsessive-Compulsive Disorder (OCD) and/or a Tic Disorder
- Pediatric Onset (symptoms appear between age 3 and puberty)
- Acute Onset and Episodic Course (sudden onset with a relapsing-remitting pattern)
- Association with Group A Streptococcal (GAS) Infection
- Association with Neurological Abnormalities (like motor hyperactivity or tics)
These criteria provide a framework, but clinical judgment and your parental observations are just as important.
The Role of Strep: Uncovering the Trigger
The "S" in PANDAS stands for Streptococcal, but the triggering infection isn't always obvious. While many think of a classic strep throat, GAS can also cause scarlet fever, skin infections like impetigo, or perianal strep. Critically, many strep infections can be asymptomatic (Barsenga, et al., 2022), meaning your child could have a significant infection without ever complaining of a sore throat.
Detecting strep also has challenges. Rapid strep tests can miss infections, which is why a follow-up culture is recommended. Even throat swabs can yield false negatives if the bacteria are hiding in the sinuses or tonsils. Blood tests for strep antibodies (ASO and Anti-DNase B) can also be misleading, as not all children show a significant rise in these markers after an infection. A high titer doesn't confirm PANDAS, and a low one doesn't rule it out.
The theory behind PANDAS is molecular mimicry. In simple terms, strep bacteria have molecules that look similar to molecules on healthy brain cells. The immune system creates antibodies to fight strep, but these antibodies can get confused and attack the brain tissue, causing inflammation and the sudden onset of symptoms. This is the same mechanism seen in other post-strep conditions like Sydenham chorea. Some children may also have a genetic predisposition to this type of immune response.
_compressed.jpeg)
Your Doctor's Toolkit: A Guide to the PANDAS Diagnosis
Because there's no single definitive test, a PANDAS diagnosis is a diagnosis of exclusion, meaning other conditions must be ruled out. This requires a thorough clinical evaluation by a knowledgeable provider.
Your doctor's toolkit includes:
- A Detailed Medical History: Your observations are invaluable. We need to know exactly when symptoms started, the pattern of flares, and any recent infections or family history of autoimmune conditions.
- Physical and Neurological Exams: These help identify signs of infection and assess for tics, motor abnormalities, or other neurological signs.
- A Psychiatric Assessment: This is crucial to differentiate PANDAS from primary psychiatric disorders like OCD, Tourette's, or ADHD.
- Laboratory Tests: While no single test confirms PANDAS, they provide supporting evidence. This may include:
- Basic blood work (CBC, immune markers, vitamins D and B-12, iron).
- Testing for strep and other infectious triggers like Mycoplasma pneumoniae or Lyme disease.
- Specialized tests like the Cunningham Panel™ or GAD65 antibody testing to look for evidence of autoimmune activity affecting the brain.
Imaging studies like an MRI or EEG aren't routine but may be used to rule out other neurological disorders. The goal is to gather enough evidence to make a clinical diagnosis while ensuring nothing else is missed. As I always say, "Let's calm the brain first," and an accurate diagnosis is the critical first step. For more guidance, the Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome provides excellent recommendations.
https://youtu.be/Z5fs2DwEpbs
PANDAS vs. PANS: Understanding the Difference
It's important to understand PANS—Pediatric Acute-Onset Neuropsychiatric Syndrome. Think of PANS as the larger umbrella, and PANDAS as one specific type underneath it.
PANS is defined by the sudden onset of OCD or severely restricted food intake, plus at least two other neuropsychiatric symptoms. The key difference is that PANS does not require a strep infection as the trigger. It can be caused by other infections (like Mycoplasma pneumoniae, influenza, or Lyme disease), immune dysregulation, or other factors.
Here's a quick comparison:
FeaturePANDASPANSTriggerGroup A Streptococcus (GAS) infection specificallyAny infection, immune trigger, or unknown cause (broader category)Core SymptomsSudden onset of OCD and/or ticsSudden onset of OCD or severely restricted food intake, plus at least 2 other neuropsychiatric symptomsDiagnostic CriteriaRequires evidence of GAS infection and meets 5 NIMH criteriaDoes not require strep; focuses on acute onset and symptom cluster
Understanding this distinction helps ensure your child gets the right diagnosis and treatment, even if the strep piece of the puzzle isn't clear.

What's Next? Navigating Life After a Diagnosis
Receiving a PANDAS diagnosis can bring a mix of emotions – relief at finally having an answer, but also apprehension about what comes next. Our message to you is always one of hope and action. With the right approach, children with PANDAS can experience significant healing and a return to their true selves.
Finding Hope and Healing After a PANDAS Diagnosis
The good news is that with early and appropriate treatment, most children with PANDAS can make a full recovery. The key is a multi-pronged approach to address the infection, calm the immune system, and manage symptoms.
- Treating the Strep Infection: The first step is eradicating any active strep infection, usually with a course of antibiotics. This can significantly reduce the duration and intensity of symptoms.
- Immunomodulatory Therapies: For more severe cases, treatments aimed at the immune response may be considered. These can include anti-inflammatory medications like corticosteroids or NSAIDs. For severe cases, Intravenous Immunoglobulin (IVIG) or Plasmapheresis (Plasma Exchange) may be used to help reset the immune system.
- Symptom Management and Behavioral Support: Addressing the neuropsychiatric symptoms is vital. Cognitive Behavioral Therapy (CBT), specifically Exposure and Response Prevention (ERP), is highly effective for OCD. SSRIs may also be used, though children with PANDAS can be sensitive to them, so low starting doses are key. School accommodations and Occupational Therapy can also provide critical support.
The long-term outlook is generally positive, but symptoms can return if the child is re-exposed to strep, making prevention important.
Dr. Roseann’s Therapist Quick Tip
In my 30+ years of practice, I've learned that diagnosing PANDAS is all about patterns—not just a single test.
What I tell parents:
Bring a clear timeline of your child’s symptoms, behaviors, and any recent strep exposures because it helps your clinician see the sudden-onset changes that define PANDAS.
Try this today:
Spend 5–10 minutes listing recent infections, mood shifts, sleep issues, tics, or OCD-like symptoms.
Why it works:
Doctors rely on clinical patterns to make an accurate diagnosis, and your timeline highlights those patterns quickly.
Finding the right support is essential. Organizations like the PANDAS Network and the International OCD Foundation offer invaluable resources. For those looking for "game-changing solutions" that focus on brain-based healing, we at Dr. Roseann offer comprehensive support for children with PANS/PANDAS. You can find More info about our PANS/PANDAS solutions.
Frequently Asked Questions
Can PANDAS syndrome be prevented?
Preventing PANDAS means preventing strep infections. Good hygiene is key: teach frequent hand-washing, not sharing cups or utensils, and covering coughs. Promptly treating any strep infections in the family can also reduce the risk of a PANDAS flare.
Can teenagers or adults get PANDAS?
While PANDAS typically appears in children before puberty (ages 3-12), it’s not impossible for it to affect older children or teenagers. Post-strep autoimmune reactions in adults are very rare and not as well-studied, but if you see a sudden onset of these symptoms at any age, it’s worth discussing with a knowledgeable provider.
What happens if PANDAS goes untreated?
Untreated PANDAS can lead to significant challenges. The neuropsychiatric symptoms can become more severe and chronic, deeply impacting a child’s school performance, social relationships, and family life. Early and proper treatment is crucial to calm the brain’s autoimmune response and prevent potential long-term complications.
Citations
Barsenga, S., Mitiku, H., Tesfa, T. et al. Throat carriage rate, associated factors, and antimicrobial susceptibility pattern of group A Streptococcus among healthy school children in Jigjiga City, Eastern Ethiopia. BMC Pediatr, 22(227). https://doi.org/10.1186/s12887-022-03294-2
Thienemann, M., Murphy, T., Leckman, J., Shaw, R., Williamsn, K., Kapphahn, C., Frankovich, J., Geller, D., Bernstein, G., Chang, K., Elia, J., and Swedo, S. (2017). Clinical management of Pediatric Acute-Onset Neuropsychiatric Syndrome: part I - psychiatric and behavioral interventions. J Child Adol. Psychopharma, 27(7). http://doi.org/10.1089/cap.2016.0145.
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies from patient to patient and condition to condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
_compressed.jpeg)
%20.png)