If your child explodes at the smallest request or melts down when asked to do something simple, you may be wondering what’s going on—and how to help.
Parenting a child with Pathological Demand Avoidance (PDA) can feel overwhelming and confusing. PDA is a profile often seen in children on the autism spectrum. It is marked by extreme anxiety-driven avoidance of everyday demands.
The good news? There are science-backed strategies and compassionate approaches that can make a real difference.
In this guide, I’ll walk you through what PDA is, what Pathological Demand Avoidance treatment looks like. And most importantly, on how you can support your child with love and confidence.
What is Pathological Demand Avoidance?
Pathological Demand Avoidance (PDA) is a behavioral profile. It’s most often linked to autism spectrum disorder.
Children with PDA experience extreme anxiety when faced with everyday demands. It can lead to avoidance, meltdowns, or defiance.
Instead of being “stubborn” or “oppositional,” kids with PDA are reacting to perceived threats to their sense of control. Their nervous system is in fight-or-flight mode. This makes it difficult for them to follow even simple requests like brushing teeth or putting on shoes.
Behavior is communication. PDA behaviors are a way for kids to manage overwhelming anxiety, not a reflection of bad parenting.
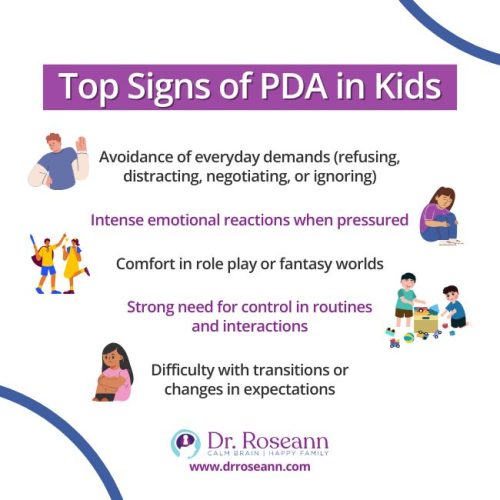
What are the Signs of PDA in Children?
Children with PDA may look very different from one another, but there are some common patterns:
- Avoidance of everyday demands (refusing, distracting, negotiating, or ignoring)
- Intense emotional reactions when pressured
- Comfort in role play or fantasy worlds
- Strong need for control in routines and interactions
- Difficulty with transitions or changes in expectations
Megan, a mom of a 12-year-old with PDA, shared that mornings were the hardest. Something as simple as asking her son to get dressed could result in a 45-minute meltdown. Once she understood his avoidance came from anxiety, not defiance, she was able to shift her approach and mornings became calmer.
Why Do Kids with PDA Avoid Demands?
At its core, Pathological Demand Avoidance (PDA) is an anxiety-driven response, not a sign of defiance. When a child with PDA is asked to do something—even something simple like getting dressed or joining a family activity—their nervous system can register the request as a threat. In that moment, they feel trapped or powerless, and their brain shifts into “survival mode.”
Common triggers include:
- Sudden changes in routine that strip away predictability
- Overwhelm from sensory input like noise, lights, or crowded spaces
- Social anxiety or fear of getting something wrong
- A perception of losing control or independence
The avoidance you see—whether it’s refusal, distraction, or even a meltdown—isn’t about being difficult. It’s the nervous system’s way of saying, “I don’t feel safe right now.” Understanding this shift helps parents reframe the behavior as biology, not willfulness, and opens the door to strategies that focus on calming the brain first instead of escalating the struggle.
What Treatment Options Work for Pathological Demand Avoidance?
There isn’t one single treatment for PDA, but there are proven approaches that help calm the brain and reduce anxiety-driven avoidance.
1. Neurofeedback and Brain-Based Therapies
These treatments help regulate the nervous system, improve self-regulation, and reduce anxiety symptoms.
2. Cognitive-Behavioral Approaches (CBT, ACT)
When adapted for PDA, therapy can help children understand their feelings. As a result, they build coping tools without triggering more avoidance.
3. Parent Coaching and Support
Equipping parents with strategies to reduce power struggles and create a calmer home environment is crucial.
4. School Accommodations
Individualized Education Programs (IEPs) or 504 plans can help. It reduces unnecessary demands and creates flexibility in learning.
“Traditional behavioral approaches often backfire with PDA kids. What works is a low-arousal, collaborative approach that prioritizes the child’s sense of autonomy.” – Dr. Elizabeth Newson, developmental psychologist who first identified PDA.
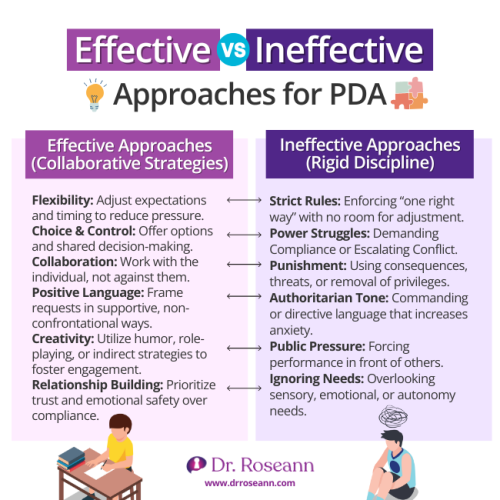
How Can Parents Support a Child with PDA at Home?
Parents are the most important part of the treatment team. The key is to reduce demand pressure and help your child feel safe.
Practical PDA Strategies:
- Offer choices instead of commands (“Do you want to brush teeth before or after pajamas?”)
- Use humor, play, and role play to diffuse stress
- Break tasks into small steps
- Build in predictable routines with flexibility
- Model calm behavior during meltdowns
Carlos noticed that asking his daughter directly to start homework always led to explosions. But when he gave her choices about where to work (at the kitchen table or in her room) and included breaks, she was able to complete her assignments with less resistance.
PDA Triggers vs. Parent Responses
| Common PDA Triggers | Parent Responses that Help |
|---|---|
| Sudden changes in routine | Give advance warnings, use visual schedules, and prep your child for transitions. |
| Sensory overwhelm (noise, crowds, lights) | Give advance warnings, use visual schedules, and prep your child for transitions. |
| Social anxiety or fear of failure | Break tasks into small steps, praise effort (not outcome), and use humor or play. |
| Feeling a loss of control | Offer choices instead of commands and use collaborative language. |
| Too many demands at once | Prioritize, space out tasks, and build in downtime. |
What Mistakes Should Parents Avoid with PDA Kids?
Even the most loving parents can accidentally make PDA behaviors worse by using traditional parenting methods.
- Avoid: Power struggles, ultimatums, rigid consequences
- Avoid: Labeling your child as “manipulative” or “lazy”
- Avoid: Overloading with too many demands at once
Instead, focus on collaboration, flexibility, and calming the nervous system first.
What is the Long-Term Outlook for Kids with PDA?
With the right support, kids with PDA can thrive. While they may always struggle with demand sensitivity, they can learn coping skills. They can build resilience and find environments where they flourish.
Early intervention, parent support, and school accommodations make a big difference in long-term outcomes.
Graphic: Quote block – “It’s not bad parenting—it’s a dysregulated brain.” – Dr. Roseann
Alt text: Inspirational quote from Dr. Roseann about PDA.
FAQ About Pathological Demand Avoidance
What causes Pathological Demand Avoidance?
PDA is not caused by parenting. It’s linked to underlying neurodevelopmental differences, often associated with autism, anxiety, or nervous system dysregulation.
Is PDA the same as Oppositional Defiant Disorder (ODD)?
No. PDA behaviors are anxiety-driven, while ODD involves deliberate defiance.
Can PDA improve with age?
Yes, with the right support, children can learn coping strategies and become more flexible over time.
What role does school play in PDA treatment?
Schools that offer flexibility, reduced demands, and sensory supports can significantly improve a child’s daily experience.
Parent Takeaway about PDA
Parenting a child with PDA isn’t easy, but you are not alone. Understanding that avoidance comes from anxiety—not defiance—can change everything. With Pathological Demand Avoidance treatment, parent support, and brain-based tools, your child can feel safer, calmer, and more capable.
Remember: Calm the brain first, and the behavior will follow.
Ready to learn more? Download our Free PDA Checklist and take the first step toward creating peace at home.
Terminology Simplified
- PDA (Pathological Demand Avoidance): A behavioral profile often linked to autism where kids avoid demands due to anxiety.
- Neurofeedback: A therapy that trains the brain to self-regulate.
- IEP/504 Plan: School-based supports that help children succeed academically and emotionally.
Citations:
O’Nions, E., Gould, J., Christie, P., Gillberg, C., Viding, E., & Happé, F. (2015). Identifying features of “pathological demand avoidance” using the Diagnostic Interview for Social and Communication Disorders (DISCO). European Child & Adolescent Psychiatry, 25(4), 407–419. https://doi.org/10.1007/s00787-015-0740-2
Shanmugam, H., Ganguly, S., & Priya, B. (2021). Plant food bioactives and its effects on gut microbiota profile modulation for better brain health and functioning in Autism Spectrum Disorder individuals: A review. Food Frontiers. https://doi.org/10.1002/fft2.125
Yasinski, C., Hayes, A. M., Ready, C. B., Abel, A., Görg, N., & Kuyken, W. (2019). Processes of change in cognitive behavioral therapy for treatment-resistant depression: psychological flexibility, rumination, avoidance, and emotional processing. Psychotherapy Research, 30(8), 1–15. https://doi.org/10.1080/10503307.2019.1699972
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to provide health advice. It is recommended to consult with a physician before beginning any new wellness program. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge











