Estimate reading time: 8 minutes
PANS diagnosis and treatment begins by noticing a sudden change—like our 8-year-old Gracie’s abrupt OCD and food refusal—then ruling out other causes, treating triggers (often infections), calming brain inflammation, and easing symptoms with therapy, school supports, and family-centered care.
Quick Overview of PANS Diagnosis and Treatment:
- Diagnosis: Based on abrupt onset of OCD/food restriction plus at least two other neuropsychiatric symptoms. Involves ruling out other conditions and testing for triggers like strep.
- Infection Treatment: Antibiotics for bacterial infections like strep.
- Inflammation Treatment: Anti-inflammatories (NSAIDs), steroids, or immunomodulatory therapies (IVIG).
- Symptom Management: Cognitive Behavioral Therapy (CBT), neurofeedback, and psychiatric medications.
- Key to Success: Early intervention and a multidisciplinary team approach.
When Your Child Changes Overnight: Understanding PANS
When your child suddenly develops intrusive thoughts, severe anxiety, or refuses to eat, it can feel like they “changed overnight.” This isn’t your imagination; it could be PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). If linked to a strep infection, it’s known as PANDAS, a subtype of PANS.
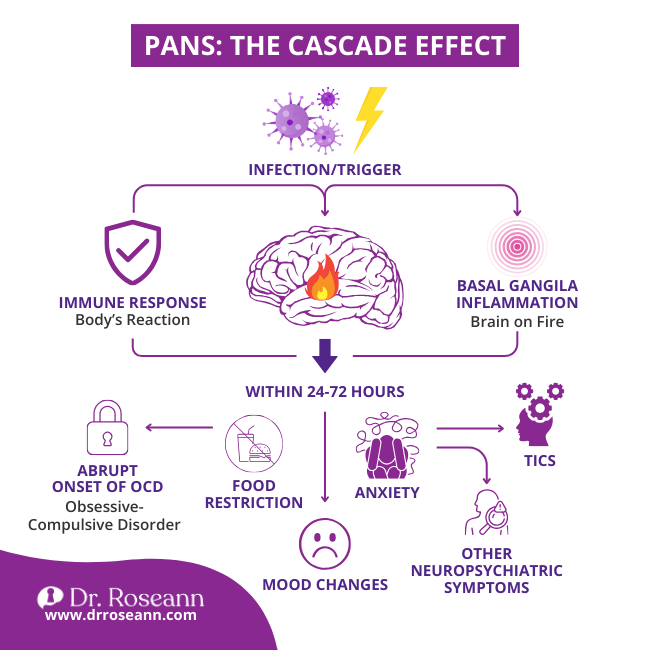
PANS occurs when a trigger, like an infection, causes the immune system to mistakenly attack the brain’s basal ganglia. This inflammation results in a sudden, dramatic onset of severe obsessive-compulsive disorder (OCD) or restrictive eating, plus a host of other neuropsychiatric symptoms.
I know how terrifying this is, but I want you to know: You’re not alone, and there is hope. PANS and PANDAS are treatable. With a proper diagnosis and a comprehensive plan, many children recover. The key is to understand the root cause and calm the brain first.
I’ve spent over three decades helping families steer PANS diagnosis and treatment using science-backed, natural approaches that address the root causes of dysregulation. My team and I specialize in calming the brain so kids can thrive—and we’re here to guide you.
A Roadmap for PANS Diagnosis and Treatment
When your child is struggling with PANS, it’s easy to feel overwhelmed by medical terminology and conflicting advice. But you don’t have to figure this out alone. Think of PANS diagnosis and treatment as a roadmap that guides you from symptoms to diagnosis to effective treatment. Our approach focuses on finding the root cause, supporting the immune system, and calming the brain so healing can happen.
Uncovering the Clues: Key Symptoms and Causes
Remember: Behavior is communication. The sudden shifts you’re seeing are your child’s brain telling you something is wrong. The hallmark signs are an abrupt, dramatic onset of obsessive-compulsive disorder (OCD) or severely restricted food intake. For a PANS diagnosis, your child must also have at least two of the following concurrent symptoms:
- Anxiety: Severe separation anxiety, panic attacks, or new, irrational fears.
- Emotional Lability or Depression: Extreme mood swings, sudden tearfulness, or overwhelming sadness and irritability.
- Aggression and Oppositional Behaviors: A previously gentle child becomes uncharacteristically aggressive or defiant.
- Behavioral Regression: A return to younger behaviors like “baby talk” or temper tantrums.
- Deterioration in School Performance: Sudden difficulty with concentration, memory, or previously mastered academic skills, like math or handwriting.
- Motor or Sensory Abnormalities: New onset of tics, clumsiness, or extreme sensitivity to light, sound, or textures.
- Somatic Symptoms: New onset of sleep problems, bedwetting, or frequent urination.
What Research Says
- A 2019 observational cohort study by Johnson et al. followed children aged 4 to 14 who met criteria for PANS at their worst point of symptoms. The researchers found that these children showed a rapid onset of complex neuropsychiatric changes, including mood shifts, anxiety, oppositional behaviors, and cognitive difficulties. Their symptoms did not develop slowly over time — they appeared abruptly and often after infection, confirming what many parents witness at home.
- In 2021, Murgia and colleagues conducted a metabolomic study examining children diagnosed with PANS. Their findings revealed distinctive metabolic and immune patterns, suggesting that the behavioral and emotional symptoms are tied to underlying neuroinflammatory and neuroimmune disruption. This helps explain why kids may suddenly experience tics, sensory issues, clumsiness, sleep problems, urinary issues, or dramatic mood swings — the brain is inflamed and struggling to regulate itself.
- A 2024 study by Bleibach et al. validated a PANS/PANDAS symptom questionnaire designed to measure the full spectrum of challenges these children face. The tool demonstrated strong reliability across ten symptom domains, including emotional instability, anxiety, behavioral regression, academic decline, somatic symptoms, and functional impairment. This means clinicians and researchers alike acknowledge PANS as a condition that affects far more than obsessive-compulsive behaviors.
At its core, PANS is a misdirected immune response where the body attacks healthy brain tissue, causing inflammation. While PANDAS is a specific subtype linked to streptococcal bacteria, PANS can be triggered by other infections (Mycoplasma pneumonia, influenza, Lyme disease), immune dysfunction, or environmental factors.
| Feature | PANDAS | PANS |
|---|---|---|
| Trigger | Specifically Group A Streptococcus | Various infections, metabolic issues, or other inflammatory reactions |
| Primary Symptoms | Abrupt onset of OCD or tics | Abrupt onset of OCD or severely restricted food intake |
| Concurrent Symptoms | At least two additional neuropsychiatric symptoms | At least two additional neuropsychiatric symptoms |
| Age of Onset | Typically prepubertal | No age limitation, though often appears in childhood |
The Path to Clarity: How PANS is Diagnosed
Getting a PANS diagnosis is a clinical process of exclusion, meaning other conditions must be ruled out. It requires a provider who understands PANS. The process involves:
- Comprehensive History: We start with your story, focusing on the abrupt onset of symptoms and any recent illnesses. Your observations are crucial.
- Physical and Neurological Exam: To check for signs of infection, inflammation, and nervous system function.
- Lab Testing: This helps identify triggers. We test for active infections and past exposure to triggers like strep (throat/perianal cultures, ASO and Anti-DNase B titers) and Mycoplasma pneumonia. We also run blood work to check for inflammation (CRP, ESR) and immune function.
No single test confirms PANS (Chang et al., 2015). The diagnosis is based on the entire clinical picture. If your provider is unfamiliar with PANS, seek a specialist.
Charting a Course for Recovery: PANS Diagnosis and Treatment Options
Once we have a diagnosis, we can start helping your child heal. Our guiding principle is simple: Let’s calm the brain first. A calmer brain is better equipped to respond to treatment. We focus on three key areas:
- Treating the Underlying Trigger: If a bacterial infection like strep is identified, antibiotics are essential to eradicate it. For other triggers, antivirals or antifungals may be used.
- Calming Brain Inflammation: We use immunomodulatory therapies to quiet the misdirected immune attack. This can include anti-inflammatory drugs (NSAIDs), a short course of corticosteroids, or for more severe cases, Intravenous Immunoglobulin (IVIG) to help reset the immune system.
- Managing Symptoms: While treating the root cause, we must support your child’s current struggles.
- Cognitive Behavioral Therapy (CBT): Especially Exposure and Response Prevention (ERP), is a cornerstone for managing OCD and anxiety.
- Neurofeedback: This is a powerful, non-invasive tool we specialize in that helps the brain self-regulate. It calms anxiety, improves focus, and improves emotional regulation, often providing game-changing results.
- Medications & Parent Support: SSRIs may be used for severe symptoms, and we provide you with strategies to manage challenging behaviors and reduce family stress.
![]()
Dr. Roseann’s Expert Quick Tip
In my 30+ years of clinical practice, I’ve learned that PANS symptoms aren’t random — they’re signals from an inflamed and overwhelmed brain.
What I tell parents:
Start by stabilizing your child’s nervous system before you try to address behaviors. A dysregulated brain can’t think clearly, follow directions, or calm down, no matter how hard a child tries. When you focus first on reducing inflammation and creating predictability, you give their brain the safety it needs to begin healing.
Try this today:
Pick one predictable routine — bedtime, mealtime, or homework time — and make it calm, consistent, and sensory-friendly. Use the same steps, same tone of voice, and same order each day.
Why it works:
PANS disrupts the brain’s ability to self-regulate. Predictable routines act like “neural anchors,” lowering threat responses and calming the limbic system. When a child’s brain expects what comes next, it can finally shift out of fight-or-flight and into healing mode.
Remember:
You aren’t trying to fix everything at once — you’re creating small pockets of calm that add up. Your child’s brain can heal, and every moment of safety you create moves them toward recovery.
Navigating the Journey to Recovery and Finding Hope
The journey with PANS can be challenging, but you’re not alone, and there is real hope for recovery. The prognosis is often very encouraging, especially with early intervention. I’ve seen children who were completely debilitated return to their vibrant, happy selves.
Early intervention is key. The sooner we calm the brain inflammation, the better the chance for a full recovery. As a parent, you are your child’s best advocate. Trust your instincts and persist in finding a knowledgeable, multidisciplinary care team.
Recovery isn’t always a straight line, so it’s important to celebrate small wins—they are signs of healing. This journey is a marathon, so please remember to take care of yourself, too. Advocating for school accommodations, like a 504 plan or IEP, can also significantly reduce stress for your child.
At Dr. Roseann, our PANS and PANDAS program digs deep to uncover root causes. We specialize in natural, effective therapies like neurofeedback that help calm the brain and support healing from the inside out. We believe in empowering parents and restoring hope. Your child can thrive again.
If you’re ready for answers and a clear path forward, we’re here to help.
Frequently Asked Questions
What is the difference between PANS and PANDAS?
PANS is the broader umbrella term for the sudden onset of severe OCD or food restriction, plus other neuropsychiatric symptoms. PANDAS is a specific subtype of PANS where the trigger is confirmed to be a Group A Strep infection. All PANDAS cases are PANS, but PANS can be triggered by many things other than strep.
Can PANS be cured?
With early and comprehensive PANS diagnosis and treatment, many children experience a full remission of symptoms. While symptoms can sometimes flare up, our goal is to manage them effectively, reduce flare frequency, and support the brain’s healing. I’ve seen many children return to their full, vibrant selves.
How can I best support my child with PANS?
Your support is powerful. Create a calm, predictable home environment. Work closely with a knowledgeable care team and remember that behavior is communication. Try to see past the symptoms to the child who is struggling. Most importantly, take care of yourself—you can’t pour from an empty cup.
How long does PANS treatment take?
The timeline varies. Some children improve within weeks of starting antibiotics and anti-inflammatory treatments. Others with more complex cases may need several months of comprehensive therapy. Early intervention is the most critical factor for a faster recovery.
Citations
Bleibach, A., Sørensen, CB., Skov, L, Christensen, KB., Debes, NM. (2024)/ Reliability and validity of a newly developed PANDAS/PANS questionnaire. Eur J Paediatr Neurol. 52:109-130. https://doi.org/10.1016/j.ejpn.2024.07.008.
Chang, K., Frankovich, J., Cooperstock, M., Cunningham, MW., Latimer, ME., Murphy, TK., Pasternack, M., Thienemann, M., Williams, K., Walter, J., Swedo, SE. (2015). Clinical evaluation of youth with pediatric acute-onset neuropsychiatric syndrome (PANS): recommendations from the 2013 PANS Consensus Conference. J Child Adolesc Psychopharmacol. 25(1):3-13. https://doi.org/10.1089/cap.2014.0084
Johnson, M., Fernell, E., Preda, I., Wallin, L., Fasth, A., Gillberg, C., Gillberg, C. (2019). Paediatric acute-onset neuropsychiatric syndrome in children and adolescents: an observational cohort study. Lancet Child Adolesc Health, 3(3):175-180. https://doi.org/10.1016/S2352-4642(19)30404-8
Murgia, F., Gagliano, A., Tanca, MG., Or-Geva, N., Hendren, A., Carucci, S., Pintor, M., Cera, F., Cossu, F., Sotgiu, S., Atzori, L., Zuddas, A. (2021). Metabolomic characterization of Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS). Front Neurosci. 15:645267. https://doi.org/10.3389/fnins.2021.645267
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!



_compressed.jpg?alt=media&token=c68bcc7e-3d87-4bc5-acfe-5b293da1fcda)
_compressed.jpg?alt=media&token=cb23dee5-7205-4b9d-9c06-c6c9c82e40da)







