
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!













Henry was a 12 yr-old-boy with a history of poor attention, impulse control issues, peer relation difficulties and non compliant behavior. His parents and grandmother reported that, “Henry came out difficult.”
He was the product of prolonged labor and was born “blue” but no concerns from the physician were noted. Colic, sleep problems, constipation, picky eating, and sensory issues were present in early childhood. Henry was easily upset and had difficulties getting along with his older sister and younger brother, as well as kids in school.
At age four, his preschool teacher expressed concerns about Henry's behavior and recommended that they speak to their pediatrician about Attention-Deficit Hyperactivity Disorder (ADHD). After a visit to the pediatrician and completion of the Vanderbilt Rating Scales, Henry was diagnosed with ADHD and prescribed Concerta for ADHD.
Henry's behavior improved for the remainder of preschool with noticeable improvement in focus and seat work. By the end of the summer and just before kindergarten, Henry's side effects from the medication, low appetite, caused him to not eat to the point that he was lethargic and losing weight. At the pediatrician's suggestion, they added PediaSure, which helped Henry gain weight but worsened his constipation (he was only eliminating a couple of times a week).
In Kindergarten, an IEP plan was put in place under the Other Health Impairment (OHI) category. His impulsiveness and mood was getting in the way of transitioning, work completion, and peer relationships. Although Henry was bright with an above average IQ of 117, his work production was poor. Throughout the years, a variety of school-based interventions were put into place. They all seemed to alleviate the problem to some degree but nothing ever seemed to really work.
Henry switched ADHD medications, which resulted in ups and downs behaviorally. His parents tried to get him to eat healthy but Henry would hoard cookies and soda and other carb foods. They would find wrappers in his room and he only stopped when the whole family gave it up. They noticed a positive shift when they cleaned up his diet and switched to soda and 100 percent juice.
Henry participated in private social skills groups in later elementary school and into middle school. Peer and sibling relations were hard for Henry because he was so impulsive that he didn't slow down enough to connect with others. He was also easily angered, which wore out other kids. He did best socially in highly structured activities and when his parents were close by to intervene.
In middle school, coupled with hormone changes, Henry's mood worsened, so his pediatrician recommended a consult with a psychiatrist. Risperdal, an antipsychotic medication to address his mood, was added but his diagnosis of ADHD did not change. Henry became very flat and gained twenty pounds in a short period of time. His parents became concerned and sought help from me at this point.
Henry's QEEG Brain Map reflected a high amount of Delta and High Beta brainwave activity wrapped around his frontal lobes, which is often seen in birth trauma and other head injury. Henry also had high levels of Alpha brainwaves, which is common in those with mood regulation issues and disorders. He had excessive brain communication in Alpha. Overall, his brain reflected exactly what his behavior looked like, high levels of dysregulation.
Phase one of his program focused on calming his brain first through a combination of neurofeedback, PEMF, dietary supplements, gut support, and psychotherapy and parent coaching to manage his moody and easily frustrated behaviors. Once the intensity and frequency of his outbursts and noncompliant behaviors subsided, one to one therapy was added.
Phase two focused wellness and nutritional coaching to support Henry and his family in making more dietary changes, as well as integrating lifestyle and stress management changes into their daily routines.
QEEG Brain Map Comparison from QEEG #1 to #3 after 47 sessions of Neurofeedback,
3 to 7 times a week of PEMF/BRT mobile port, and parent and individual therapy
in our BrainBehaviorReset™ Program. Henry was able to calm his excessive Alpha brain communication.
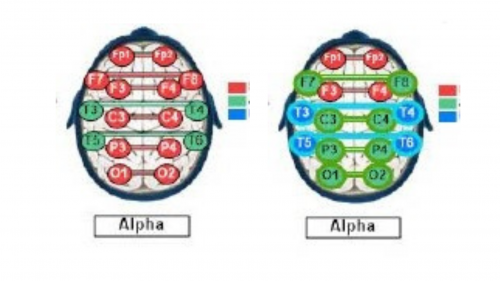
With 47 sessions of neurofeedback, 3 to 7 times a week of PEMF/BRT mobile port, parent coaching and psychotherapy, Henry’s amplitude (overactive brain wave activity) decreased on average by more than 60% in his frontal lobes.
Behaviorally, Henry’s impulsive behaviors, difficulty transitioning, behavioral outbursts, and noncompliant behaviors decreased 50% to 60%. Friction with his siblings and parents also improved with his parents working hard to reinforce the behaviors they wanted from Henry and not being so critical of his mistakes.
Socially, there were noticeable improvements in his attempts to engage with peers but he lacked skills and confidence, so he returned to social skills groups at school and privately.
In therapy, Henry had more insight into his behavior without being so defensive. He also asked for help in situations at home and school, which resulted in him attempting to or successfully resolving problems on his own some of the time.
These case studies are a description of the experiences of our clients. We have changed the names and some details to protect their privacy. Each client experience and protocol is unique in our trademarked BrainBehaviorReset™ Program.

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
