Estimated reading time: 8 minutes
Why Understanding ADHD Child Development Matters
ADHD child development is really about understanding how a child’s growing brain navigates attention, impulsivity, and emotional dysregulation at every stage from toddlerhood to the teen years. When you understand this developmental journey, you can spot shifting symptoms early and give your child the age-appropriate support their brain genuinely needs to thrive.
ADHD is a common neurodevelopmental disorder affecting 5-10% of children in the U.S. It involves differences in brain development that impact focus, impulse control, and self-regulation. Key characteristics include:
- Core Symptoms: Inattention, hyperactivity, and impulsivity appearing before age 12.
- Changing Presentation: Symptoms evolve with age; hyperactivity often lessens while inattention persists.
- Developmental Delays: A child's self-regulation skills may lag about 30% behind their peers.
While more than half of children with ADHD experience symptoms as adults, early diagnosis and effective treatment can lead to incredible success.
I've spent over 30 years helping families steer ADHD with science-backed, natural solutions. At our center, we focus on each child's unique development to create targeted interventions that calm the nervous system and build self-regulation.
Understanding the Core of ADHD in Children
Noticing ongoing distractibility or nonstop energy can be unsettling, and it's okay to ask, "Is this ADHD or just being a kid?" ADHD child development reflects a neurodevelopmental pattern of inattention and/or hyperactivity-impulsivity that disrupts daily life. For diagnosis, symptoms persist at least six months, show up in two or more settings (home and school), and several begin before age 12 (Tuncer-Ebeturk, et al., 2025).
Here's what the core symptoms look like:
- Inattention: More than just daydreaming, this involves a consistent struggle to maintain focus, making careless mistakes, seeming not to listen, losing items, and avoiding tasks that require sustained mental effort.
- Hyperactivity: This is excessive motor activity, like fidgeting, squirming, running or climbing inappropriately, and talking excessively. It can feel like a child has an internal motor that won't turn off.
- Impulsivity: This means acting without thinking, such as blurting out answers, having trouble waiting for a turn, and interrupting others frequently.
When these symptoms significantly impact school, relationships, and self-esteem, it's time to seek support.
https://www.youtube.com/watch?v=DH8La7sEtFo
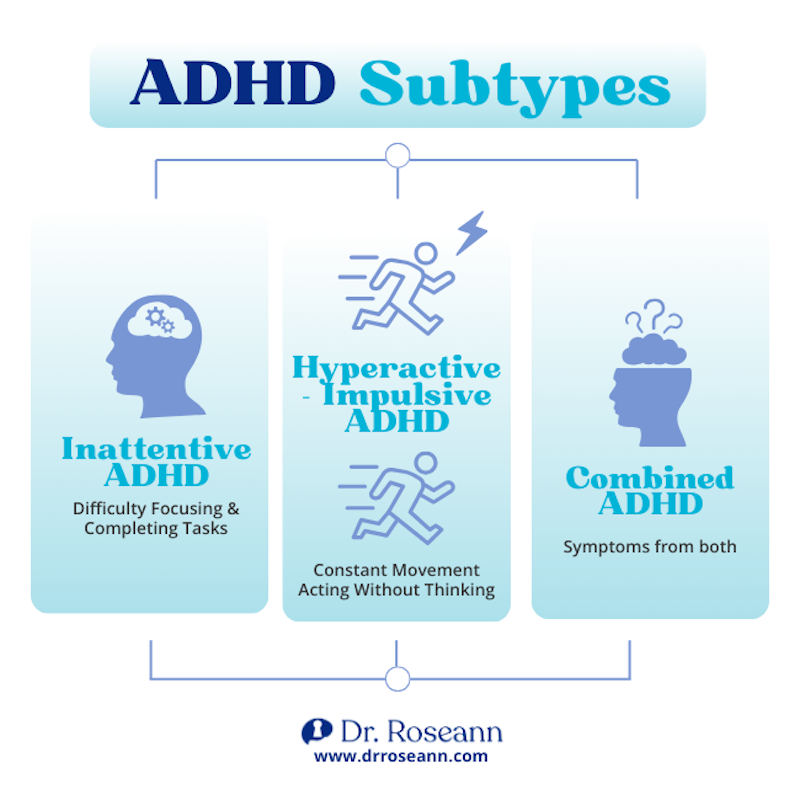
ADHD Subtypes
ADHD presents in three distinct ways, and understanding your child's subtype helps create the right support plan:
- Predominantly Inattentive Presentation: Children primarily struggle with focus but aren't significantly hyperactive. They may seem quiet or "spacey" and are often overlooked, especially girls.
- Predominantly Hyperactive-Impulsive Presentation: These children are in constant motion and act impulsively but may not have major issues with attention.
- Combined Presentation: The most common type, where children meet the criteria for both inattention and hyperactivity-impulsivity.
Inattentive Symptoms (Primary)Hyperactive-Impulsive Symptoms (Primary)Difficulty focusing on tasksFidgets or squirms frequentlyEasily distractedHas trouble staying seatedAppears not to listenOften runs or climbs inappropriatelyMakes careless mistakesHas difficulty playing quietlyStruggles with organizationIs often "on the go" or acts as if "driven by a motor"Avoids tasks requiring sustained mental effortTalks excessivelyLoses necessary itemsBlurts out answers before questions are completedForgets daily activitiesHas difficulty waiting their turn Interrupts or intrudes on others
Co-occurring Conditions
ADHD rarely appears alone. Many children also experience other conditions that can complicate diagnosis and treatment. Common co-occurring conditions include anxiety disorders, depression, and learning disabilities. Behavioral issues like Oppositional Defiant Disorder (ODD) or Conduct Disorder can also be present. Others may include Disruptive Mood Dysregulation Disorder (DMDD), substance use disorders (in teens), OCD, and Autism Spectrum Disorder (ASD). Addressing these is crucial for a child's well-being. You can find more info about co-occurring conditions we treat on our site.
Potential Causes and Risk Factors
Let's be clear: ADHD is not caused by poor parenting, sugar, or screen time. Research points to a complex interplay of factors:
- Genetics: This is the strongest risk factor. ADHD runs in families, influenced by genes affecting brain development and neurotransmitters like dopamine.
- Brain Development: Research shows differences in brain structure and function in areas responsible for executive functions like attention and impulse control.
- Environmental Factors: While not primary causes, prenatal exposure to toxins, alcohol, or tobacco, as well as premature birth, can increase risk (Rattay and Robinson, 2024). A stressful family environment can worsen symptoms, while a supportive one can help manage them.
How Gender Influences ADHD Presentation
One of the most frustrating aspects of ADHD child development is how it differs between boys and girls. For years, ADHD was seen as a "boy's disorder" because they are diagnosed more often.
Boys are more likely to show externalized hyperactivity and impulsivity—the disruptive behaviors that get noticed quickly in a classroom.
Girls with ADHD often show the inattentive type. Symptoms are more inward: daydreaming, disorganization, quiet struggles to focus. Many work hard to hide it - called social masking. That camouflage fuels underdiagnosis in girls, who get tagged as shy or unmotivated, which erodes confidence and delays care into adulthood.
I remember Jena, a girl I know who was the straight-A daydreamer that always looked put together. After school, she spent hours redoing lost assignments and apologizing for "being lazy." When a thoughtful teacher flagged her distractibility, she finally got evaluated - and the right support changed everything.
The Evolving Journey of ADHD Child Development
ADHD child development is a winding road, not a straight line. Symptoms transform as a child grows and faces new demands. A key concept is developmental delays. This means the brain areas controlling self-regulation, emotional control, and executive functions are developing at a different pace. A 10-year-old with ADHD might have the emotional or organizational skills of a typical 7-year-old, lagging about 30% behind their peers. This isn't a choice; it's a difference in developmental timing.
This delay affects:
- Self-regulation: The ability to manage thoughts, feelings, and actions.
- Emotional control: Intense emotional reactions and difficulty bouncing back from frustration.
- Executive function: The brain's management system for planning, organizing, and starting tasks.
Long-term Outlook
Parents often ask, "Will my child outgrow this?" While ADHD is typically a lifelong condition, symptoms do change. Hyperactivity often decreases with age, becoming more of an internal restlessness. Inattention, however, tends to remain stable. More than half of children with ADHD continue to experience symptoms as adults. The good news is that with effective strategies, individuals can learn to manage their symptoms and lead successful, fulfilling lives.
Key Milestones in ADHD Child Development: Toddlers to Teens
ADHD symptoms look different at every age. Recognizing these presentations helps you provide the right support at the right time.
- Preschoolers (Ages 3-5): Hyperactivity and impulsivity are most prominent. Expect constant motion, difficulty with quiet play, grabbing toys, and acting without thinking of safety. For children ages 4-5, parent training in behavior therapy is the recommended first-line treatment.
- School-Age Children (Ages 6-12): As academic demands increase, inattention becomes more obvious. This can lead to academic struggles, with difficulty completing homework, following directions, and staying organized. Social challenges also emerge due to impulsivity (interrupting, trouble taking turns) or inattention (missing social cues).
- Teenagers (Ages 13-18): While physical hyperactivity may lessen, challenges with inattention and impulsivity can have more serious consequences. This can manifest as risk-taking behavior (substance use, reckless driving), significant time management issues, and intense emotional mood swings. The demands on executive functions for planning and organization peak during these years.

The Impact of Early Diagnosis on ADHD Child Development
Early diagnosis can change a child's life. It allows intervention to begin before negative patterns become ingrained, leading to improved academic, social, and emotional outcomes.
Most importantly, an early diagnosis helps build self-esteem. It provides an explanation for their struggles, reframing them as a neurological difference rather than a personal failure. This understanding is the foundation for building a healthy self-image. Early support also prevents a negative cycle of academic failure and social rejection, reducing the risk of co-occurring conditions like anxiety and depression. With the right tools, children can thrive. We are passionate about providing families in Ridgefield, CT, and worldwide with timely interventions. Learn more info about our ADHD treatment approach and how we empower children to succeed.
Getting a Clear Diagnosis: The First Step to Support
If you suspect your child has ADHD, seeking a comprehensive evaluation is a courageous first step. A diagnosis isn't a label; it's a key that open ups understanding and effective support.
There's no single test for ADHD. Instead, diagnosis is a multi-step process that gathers information from multiple sources to create a complete picture.
The process typically includes:
- A Medical Exam: A pediatrician or family doctor will conduct an exam, including vision and hearing tests, to rule out other conditions that can mimic ADHD symptoms, such as thyroid issues or sleep disorders.
- Gathering Behavioral History: You, your child's teachers, and other caregivers will complete standardized rating scales (like the Vanderbilt or Conners assessments). This is crucial because symptoms must be present in at least two settings (e.g., home and school) for an accurate diagnosis.
- A Comprehensive Review: A healthcare provider will review your child's developmental history, family history, and current life circumstances. They will evaluate all this information against the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
For a diagnosis, symptoms must have started before age 12, been present for at least six months, and cause significant impairment in daily life. Your pediatrician may refer you to a specialist, such as a child psychologist or developmental pediatrician, for a more in-depth evaluation. An accurate diagnosis is the cornerstone of an effective treatment plan.

I've guided countless families through this process. Each step brings you closer to understanding your child and getting them the support they deserve.
A Holistic Approach to Treatment and Management
After a diagnosis, the question is, "What now?" The most effective path is a holistic approach that addresses your child's brain function, behaviors, and overall well-being, not just their symptoms.
Our game-changing solutions are for families who find traditional approaches aren't enough. A comprehensive plan often includes behavioral therapy to teach practical skills and parent training to empower you with effective strategies at home. For some, medication can be a helpful tool for reducing core symptoms. These decisions are always made in partnership with your healthcare provider. Watch a video on ADHD treatment recommendations to learn more about comprehensive care.
The Role of Natural and Integrative Solutions in Managing ADHD
I've seen profound changes when families use non-medication approaches to address the root causes of dysregulation. Instead of just managing symptoms, these natural and integrative solutions work to optimize brain function from the inside out.
Techniques like neurofeedback train the brain to self-regulate more effectively, improving focus and calm. We also use targeted nutritional interventions and supplements to address deficiencies or inflammation that impact brain health. These evidence-based interventions can be powerful standalone options or complement traditional treatments. Our goal is to deliver rapid, effective results by working with your child's biology. You can find Information about our integrative ADHD solutions that have helped thousands of families.
Beyond Pills: Effective Therapies and Healthy Habits
Medication is never the whole story for ADHD child development. The most successful outcomes involve a broader approach that includes therapies and healthy habits.
- Neurofeedback: I'm particularly passionate about this non-invasive therapy that trains the brain to improve self-regulation. By providing real-time feedback on brainwave activity, it helps the brain learn to maintain patterns associated with focus and calm, leading to lasting improvements. Find More info about Neurofeedback and see why it's a cornerstone of our approach.
- Healthy Habits: These are foundational for managing ADHD.
- Healthy Diet: Fuel the brain with whole foods, protein, and healthy fats. Minimizing processed foods can help stabilize mood and energy.
- Adequate Sleep: Poor sleep dramatically worsens ADHD symptoms. A consistent bedtime routine is critical.
- Regular Physical Activity: Exercise is like medicine for the ADHD brain, improving focus and mood.
- Limited Screen Time: Establishing healthy boundaries around digital devices is important for attention and sleep. You can find guidance on.
Empowering Your Child: Practical Strategies for Home and School
As a parent, you are your child's most powerful coach and advocate. The strategies you use at home and the partnerships you build at school can transform your child's ADHD child development journey.
Creating Structure and Daily Routines
Children with ADHD thrive on predictability. Consistent routines for mornings, homework, and bedtime act as scaffolding for their day. Use visual schedules and checklists to give your child a roadmap to follow independently. A simple chart showing "Wake up -> Brush teeth -> Get dressed -> Eat breakfast" reduces nagging and builds autonomy.
The Power of Positive Reinforcement
Aim for at least five positive comments for every one criticism. Notice and praise specific behaviors, like "I saw you started your homework right away—that was great planning!" A simple reward system tied to specific goals can also be a powerful motivator.
Clear Communication That Actually Works
Get your child's attention with eye contact before speaking. Keep instructions simple and brief. Instead of "Clean your room," break it down into manageable chunks like, "First, put the dirty clothes in the hamper." Use timers to create short, focused work periods followed by a break.
Building Connection Through Quality Time
Plan for regular, conflict-free, screen-free time together. This isn't about teaching; it's about connection. Playing a game or going for a walk strengthens your relationship and builds positive memories.
Here are five effective behavioral strategies:
- Praise and reward good behavior at least five times more often than you criticize.
- Give practical, brief, and simple directions, making eye contact first.
- Ensure adequate sleep, healthy diet, and daily exercise.
- Develop routines for homework and chores using checklists and planners.
- Spend special, conflict-free time with your child regularly.
School Support and Accommodations
Effective school support is transformative. Collaborate with teachers by sharing what you know about your child's ADHD, what works at home, and what triggers difficulties. Regular check-ins keep everyone on the same page.
If your child needs formal support, two legal frameworks can help: an Individualized Education Program (IEP) or a 504 Plan. A 504 Plan provides accommodations to level the playing field, such as extended time on tests or preferential seating. An IEP provides specialized instruction for children who need modified curriculum or direct support. You can Learn about special education services to understand your rights.
Effective classroom accommodations might include seating near the teacher, breaking assignments into smaller parts, providing written instructions, or allowing movement breaks. These aren't special treatment; they are necessary adjustments that help your child access their education.
Dr. Roseann's Quick Tip
Understanding ADHD child development is a journey with challenges and opportunities for growth. From the constant motion of a preschooler to the organizational struggles of a teen, ADHD evolves at every stage. But with patience and the right support, children with ADHD can truly thrive.
Frequently Asked Questions
How common is ADHD in children?
ADHD is one of the most common neurodevelopmental disorders, affecting approximately 5% to 10% of children in the United States. This means in a typical classroom, at least one or two students likely have ADHD. While it’s diagnosed more often in boys, we now know it presents differently in girls, who are often underdiagnosed. For many, it’s a lifelong condition.
Can a child outgrow ADHD?
Children don’t typically “outgrow” ADHD, but symptoms often shift with age—hyperactivity tends to decrease while inattention and internal restlessness can persist. More than half have symptoms into adulthood, yet with targeted supports and strong coping strategies they can manage ADHD and thrive by leveraging their strengths.
What are the first steps if I suspect my child has ADHD?
Trust your instincts. Early action can make a huge difference.
Start by talking with your pediatrician and sharing specific observations so they can rule out other conditions and discuss next steps. Document when and where behaviors occur, seek a comprehensive evaluation (your doctor may refer you to a child psychologist), and contact your child’s school so teachers can provide observations and begin discussing support and accommodations.
Citations
Rattay K, Robinson LR. Identifying risk factors for Attention-Deficit/Hyperactivity Disorder (ADHD): a public health concern and opportunity. Prev Sci. 25(2):195-202. http://doi.org/10.1007/s11121-024-01667-w.
Tuncer-Ebetürk, I., Kim, J., and Soysal, Y. (2025). The global rise in children’s attention-deficit/hyperactivity disorder prevalence: a macro-sociological explanation, Social Forces. https://doi.org/10.1093/sf/soaf153
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to provide health advice. It is recommended to consult with a physician before beginning any new wellness program. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions—so you are in the right place!

%20.png)