Estimated reading time: 6 minutes
When you’re raising a child with ADHD, the pressure to medicate can feel overwhelming. Doctors, schools, even other parents may suggest it’s the only answer. But medication isn’t always the best first step—and it’s not the only way to help your child.
In this article, I’ll share five important reasons to pause before turning to prescriptions, and how calming the brain first can open the door to real, lasting change.
What Are the Hidden Dangers of ADHD Medications?
ADHD meds are often prescribed like a quick bandage, but what parents often aren’t told are the hidden trade-offs.
Sure, they can sharpen focus for a bit, but research shows those same pills almost always bring side effects that ripple through mood, growth, or even brain development (Mosholder et al., 2009). Parents deserve the whole story before making such an important decision.
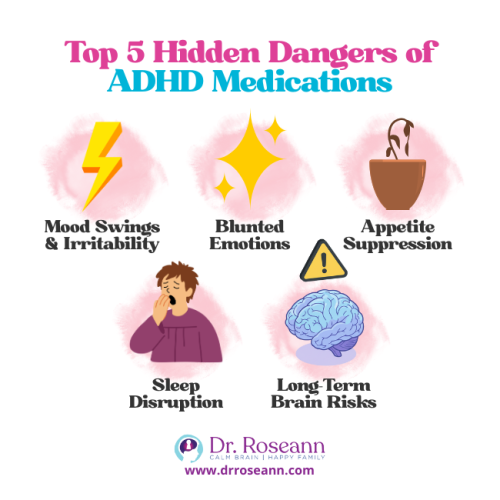
Top 5 Reasons Why Not To Medicate Your ADHD Child:
| Mood swings and irritability | Kids may get more emotional, edgy, or withdrawn. |
| Blunted emotions | That natural sparkle, creativity, or goofy joy can fade away. |
| Appetite suppression | Meals shrink, growth slows, like a plant with less water. |
| Sleep disruption | Nights turn restless, mornings start foggy, and learning takes the hit. |
| Long-term brain risks | Studies warn of possible impacts on how the brain matures and self-regulates (Volkow & Swanson, 2013). |
Here’s the thing—behavior is communication, not the root problem.
QEEG brain mapping digs deeper, showing ADHD with up to 89% accuracy versus only 47–58% for traditional rating scales (Kim et al., 2015). Instead of guessing, we can actually watch brainwaves tell their story and then target the treatment where it counts.
Parents often turn to meds because no one offers another path. Yet stimulants can alter brain chemistry, reinforce dependence, and even raise the risk of later addiction. It’s like patching a leaky pipe with tape—sooner or later, the water bursts through.
Parent Story
Emily, mom of a 9-year-old, thought meds would finally bring peace. And yes, her son sat still in school. At home though, he skipped dinner, snapped easily, and the pounds slipped away. “It felt like we traded one problem for another,” she sighed.
Takeaway: Short-term gains can hide long-term costs. You have choices, and when we calm the brain first—everything follows.
Why Do Doctors Prescribe ADHD Medications So Often?
Doctors often overprescribe stimulants like Ritalin or Adderall because they can quickly improve focus and reduce impulsivity. But what’s often missed is that these medications don’t treat the root cause—a dysregulated nervous system.
- Meds manage symptoms, not brain regulation.
- Once the medication wears off, behaviors often return.
- Many children cycle through multiple prescriptions, searching for the “right fit.”
Research confirms that while stimulants may reduce core ADHD symptoms in the short term, they don’t address underlying brain regulation—and their effectiveness often fades over time (Molina et al., 2009).
That’s why I remind parents: behavior is communication, and until we calm the brain first, true change can’t happen.
Do ADHD Medications Affect My Child’s Personality?

Yes, for some children. Parents often report their once-joyful child becoming withdrawn, quiet, or even “flat.”
- Blunted emotions – kids may lose their spark. Research notes that emotional blunting and personality changes are recognized side effects of stimulant treatment (Storebø et al., 2015).
- Heightened anxiety – some feel jittery or “on edge.”
- Loss of creativity – daydreaming and play can decline.
Parent Story
Mark, dad to 12-year-old Ava, noticed she stopped singing and drawing—her favorite outlets—after starting meds. “She was calm, but she wasn’t Ava anymore.”
The takeaway? When a child’s spark dims, it’s often a sign of nervous system dysregulation—not misbehavior. Let’s calm the brain first so their true self can shine again.
Are ADHD Medications Safe Long-Term?
This is one of the most common concerns parents ask me. The truth: We don’t have enough research on the long-term effects.
- The American Academy of Pediatrics warns of appetite suppression and the need for growth monitoring.
- Studies also raise concerns about brain development when stimulants are used for years, and the risks of dependency or misuse increase in adolescence (Faraone & Buitelaar, 2010).
The bottom line? Parents deserve the full picture, and there are safe, natural ways to calm the brain first—without relying on long-term medication.
What Are Natural Alternatives to ADHD Medications?
The good news? You have real options. Natural supports can calm the brain, lift mood, and improve focus—without the hidden risks of medication.
Brain-Calming Supports
- Magnesium – the “calm mineral” that eases hyperactivity
- Omega-3s – build brain connections for sharper focus
- Inositol (B8) – balances mood and repetitive thoughts
- Neurofeedback – trains the brain to regulate itself
- Lifestyle pillars – sleep, movement, nutrition, and reducing toxins
ADHD behaviors start in a dysregulated nervous system. Once you understand that, the right tools become clear. Neurofeedback, for example, teaches the brain how to self-regulate with virtually no side effects and has shown measurable benefits in reducing ADHD symptoms (Cortese et al., 2016).
Also, The American Academy of Pediatrics has given Neurofeedback a Level 1 effectiveness rating for ADHD—the same as medication—yet most physicians don’t share this with parents.
At my Ridgefield, CT office—and virtually with families worldwide—we pair nervous system regulation with new learning through tools like Neurofeedback, PEMF therapy, Psychotherapy, Executive Functioning support, and Parent Coaching.
The goal isn’t just to hand parents tools but to teach them how to use them so their child’s brain and body can thrive. This is the foundation of my BrainBehaviorReset™ Program—helping kids reduce symptoms while learning healthier ways to respond.
Food choices matter too.
- Diets high in sugar and processed foods can worsen symptoms, while boosting nutrients or removing irritants often helps the brain settle.
- Lab testing frequently uncovers hidden deficiencies or toxins that disrupt regulation.
Other gentle supports, like homeopathy, may also help. Parents often tell me how even small changes unlocked more calm, creativity, and joy in their child.
Bottom line: Behavior is communication. When we calm the brain first, focus, mood, and learning naturally follow.
How Can I Support My Child Without Relying on Medication?
Parenting a dysregulated child is exhausting, but you’re not failing—your strategies just won’t work until the brain is calm.
Here’s what helps:
- Co-regulation: Your calm is their anchor.
- Structure and routine: Predictability helps ADHD brains thrive.
- Sensory breaks: Movement or breathing resets the nervous system.
- Regulation First Parenting™: Regulate → Connect → Correct.
Parent Story
Sarah, mom of twins with ADHD, added daily “reset breaks” like jumping jacks or short walks. She saw fewer meltdowns and smoother homework time.
The takeaway? When you calm the brain first, everything else—learning, behavior, connection—finally starts to flow.
Parent Action Steps
FAQs
Do ADHD medications stunt growth?
Yes. Stimulants can reduce appetite, which may slow growth if not carefully monitored. Regular check-ins with your pediatrician can help keep your child healthy and thriving.
Can my child stop ADHD meds suddenly?
No. Always consult a doctor first. Stopping abruptly can trigger mood swings, fatigue, or other withdrawal effects.
Do children’s vitamins interfere with ADHD?
No. Nutrients like zinc and magnesium support brain function and focus. Ensuring balanced nutrition helps your child’s nervous system regulate naturally.
Are natural options safe with medication?
Often, yes. Always check with a healthcare provider before combining supplements with prescriptions to ensure safety and effectiveness.
Will ADHD go away without meds?
ADHD stems from nervous system dysregulation. With proper supports, many children learn self-regulation and thrive without long-term medication.
Citations
Cortese, S., Ferrin, M., Brandeis, D., Holtmann, M., Aggensteiner, P., Daley, D., Santosh, P., Simonoff, E., Stevenson, J., Stringaris, A., Sonuga-Barke, E. J., & European ADHD Guidelines Group (EAGG) (2016). Neurofeedback for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes From Randomized Controlled Trials. Journal of the American Academy of Child and Adolescent Psychiatry, 55(6), 444–455. https://doi.org/10.1016/j.jaac.2016.03.007
Kim, J., Lee, Y., Han, D., Min, K., Kim, D., & Lee, C. (2015). The utility of quantitative electroencephalography and Integrated Visual and Auditory Continuous Performance Test as auxiliary tools for the Attention Deficit Hyperactivity Disorder diagnosis. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology, 126(3), 532–540. https://doi.org/10.1016/j.clinph.2014.06.034
Molina, B. S. G., Hinshaw, S. P., Swanson, J. M., Arnold, L. E., Vitiello, B., Jensen, P. S., Epstein, J. N., Hoza, B., Hechtman, L., Abikoff, H. B., Elliott, G. R., Greenhill, L. L., Newcorn, J. H., Wells, K. C., Wigal, T., Gibbons, R. D., Hur, K., Houck, P. R., & MTA Cooperative Group (2009). The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry, 48(5), 484–500. https://doi.org/10.1097/CHI.0b013e31819c23d0
Mosholder, A. D., Gelperin, K., Hammad, T. A., Phelan, K., & Johann-Liang, R. (2009). Hallucinations and other psychotic symptoms associated with the use of attention-deficit/hyperactivity disorder drugs in children. Pediatrics, 123(2), 611–616. https://doi.org/10.1542/peds.2008-0185
Storebø, O. J., Ramstad, E., Krogh, H. B., Nilausen, T. D., Skoog, M., Holmskov, M., Rosendal, S., Groth, C., Magnusson, F. L., Moreira-Maia, C. R., Gillies, D., Buch Rasmussen, K., Gauci, D., Zwi, M., Kirubakaran, R., Forsbøl, B., Simonsen, E., & Gluud, C. (2015). Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). The Cochrane database of systematic reviews, 2015(11), CD009885. https://doi.org/10.1002/14651858.CD009885.pub2
Volkow, N. D., & Swanson, J. M. (2013). Clinical practice: Adult attention deficit-hyperactivity disorder. The New England journal of medicine, 369(20), 1935–1944. https://doi.org/10.1056/NEJMcp1212625
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
Grab your complimentary copy of












