Estimated reading time: 12 minutes
You can feel it before they even speak. A heaviness in the air, almost like the house is holding its breath. Then, here it comes — the meltdown that erupts faster than you can say “bedtime.”
For kids dealing with ADHD, anxiety, OCD, autism, or PANS/PANDAS, sleep isn’t just rest. It’s the brain’s nightly reset button, and without it, even tiny frustrations can feel like tidal waves.
The challenge? Dysregulated kids often can’t fall asleep easily, wake up through the night, and greet the morning already running on empty. A tired brain loses its emotional “shock absorbers,” so the smallest bump can send everything flying.
Poor sleep and dysregulation feed off each other like a loop you can’t escape. Break the loop, calm the brain, and watch everything else start to follow.
Key Takeaways
- Poor sleep and regulation struggles often fuel each other.
- Dysregulated kids feel sleep loss more intensely.
- Small changes can improve rest and daily regulation.
- Persistent issues may require professional evaluation.
Why Sleep Disruption Hits Dysregulated Kids Harder
Restorative sleep repairs and resets the brain, especially for a dysregulated nervous system. Without that nightly reset, the brain shifts into survival mode, making it harder to focus, manage emotions, and filter stress.
And as a parent, you’ve probably seen this play out — your child’s tired eyes in the morning, their short fuse by afternoon, and those big emotional waves by evening.
In kids, sleep loss can trigger:
- An overactive amygdala — the brain’s built-in alarm stays on high alert
- Weakened prefrontal cortex function — decision-making and self-control decline
- Neurotransmitter imbalance — mood and attention regulation become harder
For a child already prone to overreacting, these changes can turn everyday challenges into emotional earthquakes (Yoo et al., 2007).
Read more about: Causes of Dysregulation in Kids
The Sleep-Regulation Feedback Loop
Sleep shapes regulation, and regulation shapes sleep — like two dancers who keep tripping over each other’s feet. You fix one step, the other stumbles.
Here’s what that often looks like for dysregulated kids:
- Stress or overstimulation makes it hard to wind down at night.
- Sleep disruption leads to a tired brain that can’t regulate emotions well.
- Poor regulation during the day increases anxiety, irritability, or hyperactivity.
- That heightened state makes it even harder to fall asleep the next night.
Unless you break the cycle, it keeps looping — gaining speed, draining everyone’s energy. Calm the brain first, and you’ll be amazed at what follows.
Hidden Sleep Disruptors That Parents Miss
Sleep struggles sometimes wave a big red flag — like a child who flat-out refuses to get in bed. Other times, the cause hides right in front of you, quietly chipping away at rest.
For dysregulated kids, even the smallest disruption can send the whole night off track — but once we find and address those triggers, sleep (and behavior) start to improve.
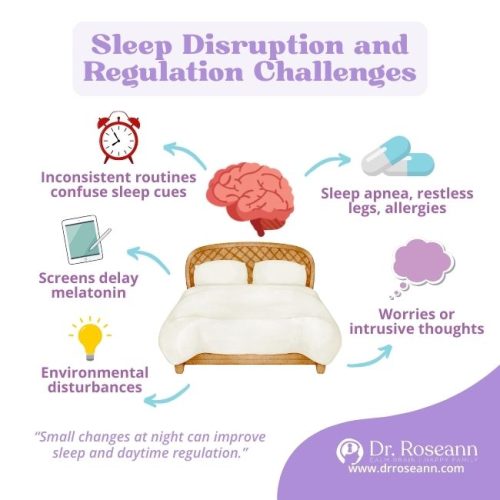
Here are the common culprits:
- Inconsistent bedtime routines that confuse the brain’s sleep cues
- Screens before bed delaying melatonin and keeping the brain alert
- Noise, light, or temperature changes
- Medical issues like sleep apnea, restless legs, or allergies
- Anxiety or intrusive thoughts that keep the brain in overdrive
Parents often focus on daytime strategies, but for many kids, the real breakthroughs start at night.
The Role of Anxiety in Sleep Disruption
When a child worries, replays the day, or anticipates problems before bed, anxiety can quietly hijack their sleep.
An anxious brain can:
- Delay sleep onset (lying awake for hours)
- Cause frequent night wakings from hyper-alertness
- Make mornings miserable because the brain never reached deep sleep
For dysregulated kids, this isn’t about “bedtime fears” — it’s a nervous system stuck in fight-or-flight mode. The good news? We can help the brain learn to feel safe enough to rest.
How Sleep Deprivation Amplifies Regulation Challenges
A tired brain is like a phone running on 3% battery — everything takes more effort, and shutdown can happen without warning.
Here’s how insufficient sleep shows up in dysregulated kids:
- More meltdowns over small frustrations
- Difficulty shifting attention from one task to another
- Lower tolerance for sensory input (noise, touch, lights)
- Increased impulsivity and poor decision-making
- Mood instability — rapid swings between irritable, sad, and hyper
In short: less sleep means less emotional “buffer” between your child and the world. And science backs this up — even moderate sleep loss can seriously shake a child’s ability to regulate emotions (Beattie et al., 2015).
Science-Backed Strategies to Improve Sleep in Dysregulated Kids
Bedtime with a dysregulated child can feel like landing a plane in a thunderstorm — tense, unpredictable, and exhausting. You’re doing everything “right,” but the more you push for sleep, the more their brain pushes back.
Listen to: Restful Sleep, Regulated Behavior: Dr. Roseann’s Sleep Strategies for Kids
It isn’t about forcing the body to rest — it’s about calming the brain first. When the nervous system feels safe, sleep follows naturally.
1. Anchor the Day with Consistency
The brain thrives on predictable patterns.
- Keep wake times, meal times, and bedtime routines as consistent as possible — even on weekends.
- Regular schedules act like a “daily GPS” for the brain, boosting both sleep quality and daytime emotional regulation (Mindell & Williamson, 2018).
And yes, it can feel impossible on busy nights, but even small wins add up over time.
2. Create a Wind-Down Window
About an hour before bed, shift to low-stimulation activities:
- reading
- drawing
- calming music
This gentle slowdown signals the brain to shift gears and tells the nervous system it can stand down. Small, steady habits lead to big changes in a child’s ability to settle.
3. Limit Screen Time in the Evenings
Screens disrupt melatonin, the hormone that invites sleep.
- Shut them off 60–90 minutes before bed (Chang et al., 2015).
- Evening screen use delays sleep onset and shortens total rest (Hale & Guan, 2015).
Think of it as giving the brain time to find the “brake pedal” before trying to rest.
4. Optimize the Sleep Environment
Think cool, dark, and quiet.
- Blackout curtains help.
- A white noise machine can hide random bumps in the night.
- Weighted blankets can be soothing for some children, offering that “deep pressure hug” the nervous system loves.
Finding the right sensory tools for your child can turn bedtime from a battle into a bonding moment.
5. Address Underlying Health Issues
Snoring, mouth breathing, or tossing and turning aren’t just “quirks.”
- They can point toward medical issues that quietly wreck sleep.
- Mention them to your pediatrician before they snowball into behavior or learning struggles.
6. Teach Relaxation Techniques
Breathing exercises, guided imagery, or progressive muscle relaxation can pull a child out of high-alert mode.
If bedtime feels like a battle some nights, it doesn’t mean you’ve failed — it just means your child’s brain needs more practice finding calm.
Better sleep isn’t an overnight fix. The good news? With consistency, gentle support, and a focus on calming the brain first, your child’s nervous system can relearn how to rest — and you can reclaim some peace at night, too.
Breaking the Cycle for Good
If you’ve tried routines and a calm environment but your child still struggles with sleep — and regulation challenges feel like they’re growing — it’s time to dig a little deeper.
Sometimes, what feels like a bedtime battle is actually your child’s brain sending signals that something more is going on.
Sleep difficulties can hint at:
- Chronic anxiety or mood concerns
- Neurological conditions such as ADHD or ASD
- Immune or metabolic issues like PANS/PANDAS
- Sleep disorders needing medical evaluation
A professional can help figure out whether it’s behavioral, medical, or both. Even one small insight can spark meaningful change and shift nights from chaos toward calm.
Sleep isn’t just about bedtime. Calming the nervous system during the day teaches the brain it’s safe to release tension at night.
Pair routines with brain-calming strategies like:
- Co-regulation
- Mindfulness
- Nervous system therapies
Better sleep takes time, but each small win strengthens emotional stability, focus, and well-being.
The Dysregulation Solution guides you step-by-step to calm the brain, improve behavior, and help your child reclaim restful nights — and give the whole family peace.
Calm the Brain First, Everything Follows.
FAQs
What happens when your child’s sleep is disrupted?
Poor sleep affects mood, focus, and emotional regulation. A dysregulated nervous system can lead to irritability, hyperactivity, or meltdowns, making daily life harder for both child and parent. Restoring calm sleep supports brain regulation, learning, and overall well-being, creating a foundation for healthier behavior and emotional stability.
How does daytime stress affect my child’s sleep?
Stress during the day keeps the nervous system on high alert, making it harder for the brain to relax at bedtime. Small interventions like calming routines, predictable schedules, and co-regulation can reduce tension and help your child’s brain feel safe enough to let go and rest.
How can I tell if my child’s sleep issues are linked to dysregulation?
If your child struggles to wind down, has frequent meltdowns, or shows extreme irritability after little rest, their nervous system may be dysregulated. Observing patterns across daytime behavior and nighttime rest can reveal whether sleep struggles are more than just a “phase.”
Citations
Beattie, L., Kyle, S. D., Espie, C. A., & Biello, S. M. (2015). Social interactions, emotion and sleep: A systematic review and research agenda. Sleep medicine reviews, 24, 83–100. https://doi.org/10.1016/j.smrv.2014.12.005
Chang, A. M., Aeschbach, D., Duffy, J. F., & Czeisler, C. A. (2015). Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences of the United States of America, 112(4), 1232–1237. https://doi.org/10.1073/pnas.1418490112
Hale, L., & Guan, S. (2015). Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep medicine reviews, 21, 50–58. https://doi.org/10.1016/j.smrv.2014.07.007
Mindell, J. A., & Williamson, A. A. (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep medicine reviews, 40, 93–108. https://doi.org/10.1016/j.smrv.2017.10.007
Yoo, S. S., Hu, P. T., Gujar, N., Jolesz, F. A., & Walker, M. P. (2007). A deficit in the ability to form new human memories without sleep. Nature neuroscience, 10(3), 385–392. https://doi.org/10.1038/nn1851
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!










