Estimated reading time: 15 minutes
When I first met Jonah, a bright six-year-old, his parents were worn out. Mornings were chaotic, afternoons were meltdown zones, and evenings turned into battles over the smallest tasks. His mom said, “We never know what kind of Jonah we’re going to get.”
That’s the reality many families face when AuDHD goes unrecognized.
The truth is yes — autism and ADHD can co-occur. In fact, research shows that many kids who meet criteria for one diagnosis also show signs of the other. This overlap has a name: AuDHD.
AuDHD is more than just a combination of two conditions. It’s a unique experience that affects how a child thinks, feels, learns, and connects.
And because it often gets overlooked, many families don’t get the guidance or support they desperately need.
In this guide, I’ll walk you through:
- What AuDHD actually means
- Common symptoms and signs at different ages
- Why girls and women often get missed
- The realities of AuDHD burnout
- Coping strategies that actually help
- Therapies and supports available to your family
Most importantly, I want you to know this: your child’s behaviors are not your fault — they’re a reflection of a nervous system that needs support. When we calm the brain first, kids can learn, grow, and thrive.
Key Takeaways
- AuDHD is the co-occurrence of autism and ADHD.
- Symptoms overlap but create unique challenges, especially in girls and women.
- Burnout is common but preventable with regulation and support.
- Parents can help by calming the brain first and building daily anchors.
- Therapies and accommodations can dramatically improve quality of life.
What is AuDHD?
For years, clinicians didn’t diagnose both conditions together — it was one or the other. But we now know that many children (and adults) experience traits of both.
Recent studies suggest that up to 30–50% of autistic individuals also meet ADHD criteria and vice versa.
Why does it happen?
Both ADHD and autism are neurodevelopmental conditions, meaning the brain develops and functions differently from the start. They share genetic, neurological, and environmental factors, which explains why traits often overlap.
How is AuDHD different?
- ADHD alone: struggles with attention, impulsivity, hyperactivity, and executive function.
- Autism alone: challenges with social communication, sensory regulation, and repetitive behaviors.
- AuDHD together: kids experience both sets of challenges at once, often creating unique struggles — like being socially interested but unable to regulate impulses, or wanting routine but struggling with organization.
Think of it as two soundtracks playing at the same time — each distinct, but overlapping in ways that change the entire rhythm of daily life.

Diagnosis and Assessment of AuDHD
Getting an accurate diagnosis can be one of the biggest hurdles for families. For years, clinicians weren’t even allowed to diagnose ADHD and autism together, which means many kids were either missed entirely or given only half the picture.
How Clinicians Evaluate
A thorough evaluation usually involves parent and teacher questionnaires, developmental history, behavioral observations, and sometimes neuropsychological testing. A skilled clinician looks at how attention, sensory processing, communication, and regulation all interact.
Common Misdiagnoses
Because AuDHD traits can look like other conditions, kids are often mislabeled as:
- “Just ADHD” — overlooking social communication and sensory challenges.
- Anxious or depressed — when the anxiety is actually secondary to sensory overload or executive dysfunction.
- Oppositional or defiant — when behaviors are really nervous system responses, not intentional misbehavior.
What Parents Can Track at Home
Before an evaluation, you can help by jotting down:
- Patterns of attention and focus
- Sensory triggers (noise, clothing, food sensitivities)
- Emotional responses (meltdowns, shutdowns, or anxiety)
- Social observations (friendships, play, communication struggles)
STORY (CONTINUATION): Jonah’s parents came to me with journals full of notes about his daily struggles and triggers — that clarity helped us piece together the full AuDHD picture and get him the right support.
AuDHD Symptoms: How Autism + ADHD Present Together
Recognizing AuDHD symptoms can be tricky, because autism and ADHD traits can blend together.
Overlapping Symptoms
- Difficulty focusing
- Impulsivity or acting without thinking
- Trouble with transitions and flexibility
- Emotional outbursts or meltdowns
- Executive function challenges (planning, organizing, following through)
Unique AuDHD Traits
- Sensory overwhelm combined with inattention.
- Hyperfocus in some areas, paired with difficulty finishing basic tasks.
- Demand avoidance plus executive dysfunction.
How Symptoms Show Up by Age
| Age | Possible Signs of AuDHD |
|---|---|
| Early Childhood | Sensory meltdowns, short attention span, constant movement. |
| School Age | Trouble following directions, difficulty making friends, struggles with homework. |
| Teens | Social anxiety, disorganization, burnout from masking, identity struggles. |
| Adults | Work challenges, relationship strain, exhaustion from juggling demands. |
STORY (CONTINUATION): For Jonah, this looked like covering his ears at the buzz of classroom lights or melting down when his toy didn’t fit together just right. At the same time, he could hyperfocus on dinosaurs for hours, showing how passion and overwhelm can live side by side in AuDHD.
👉 Remember: Every child is different. Some AuDHD kids are chatty and energetic; others are quiet and shut down. The key is looking at the pattern of traits across both autism and ADHD.
AuDHD in Women: Why It Often Goes Missed
Many moms tell me, “I didn’t realize I was AuDHD until my child got diagnosed.” That’s because girls and women often mask — meaning they camouflage their struggles to fit in socially.
Why Girls Get Overlooked
- They may appear “shy” or “daydreamy” instead of hyperactive.
- They mimic peers to hide social challenges.
- Teachers may see them as “chatty” or “sensitive,” not struggling.
Hormonal Influences
Shifts during puberty, PMS, postpartum, and perimenopause can all worsen AuDHD symptoms.
The Emotional Cost of Masking
Masking may help girls fit in, but it often leads to:
- Exhaustion after holding it together all day.
- Anxiety and depression from constant pressure to perform.
- Burnout after months or years of masking.
- A sense of “not being enough” when they can’t show up as themselves.
This is why recognizing and supporting AuDHD girls is so critical. When we create safe spaces where they don’t need to mask, we not only reduce their stress but also help them grow into authentic, confident young women.
Read more: AUDHD in Women: Signs, Challenges and Support Strategies
AuDHD Burnout: Understanding and Preventing Exhaustion
If your child seems to hit a wall and suddenly can’t cope anymore, you may be seeing AuDHD burnout. This isn’t laziness or weakness. It’s the nervous system sending out a red flag: “I can’t keep up with all of this input, pressure, and effort anymore.”
Signs of AuDHD Burnout
- Withdrawal from friends and family
- Emotional shutdowns or frequent meltdowns
- Loss of interest in hobbies
- Extreme fatigue, even after rest
- Increased anxiety or depression
Causes of Burnout
- Constant sensory and emotional overload
- Pressure to perform
- Chronic masking
- Lack of proper support
Recovery and Prevention
- Rest and downtime without guilt
- Sensory-friendly environments
- Daily nervous system regulation (breathing, movement, PEMF, neurofeedback)
- Emotional support from safe relationships
STORY (CONTINUATION): Jonah’s meltdowns dropped dramatically once his parents added short sensory breaks at home and worked with his school to provide quiet spaces for him to reset.

AuDHD Coping Strategies That Work
Coping isn’t about fixing your child; it’s about giving their nervous system tools to regulate.
1. Calm the Brain First
- Deep breathing, yoga, PEMF therapy, neurofeedback
- Prioritize sleep, hydration, and movement
2. Build Daily Anchors
- Predictable schedules and routines
- Sensory breaks built into transitions
- Nutrition that balances blood sugar
3. Use Practical Supports
- Visual schedules and checklists
- Noise-canceling headphones
- Body doubling for homework or chores
4. Family Systems Approach
- Include siblings in regulation strategies
- Collaborate with schools on accommodations
- Choose therapies that involve parents, not just the child
STORY (CONTINUATION): At the center, Jonah learned to use a “calm corner” stocked with fidgets and soft textures, while his parents used picture checklists at home. These simple tools gave him structure without battles.
The Role of Emotional Dysregulation in AuDHD
Emotional storms aren’t “bad behavior” — they’re signs of a nervous system on overload. Kids may go from calm to explosive in seconds, because their brains struggle to filter input and self-soothe.
Why Emotional Reactions Happen So Fast
- Brain Wiring Differences: The prefrontal cortex is less efficient in both ADHD and autism.
- Sensory Processing Challenges: Background noise, bright lights, or sudden changes can trigger overwhelm.
- Executive Function Struggles: Kids may know what they should do but can’t access skills quickly in the moment.
- Emotional Memory: Past experiences prime stronger reactions to stress.
How Emotional Storms Show Up
- Screaming at small frustrations
- Shutting down when overwhelmed
- Explosive anger followed by regret
- Rapid mood swings
STORY (CONTINUATION): Jonah’s parents often described two extremes: fiery outbursts over tiny frustrations, and sudden shutdowns where he curled up quietly in his room. This push-pull is common in young kids with AuDHD.
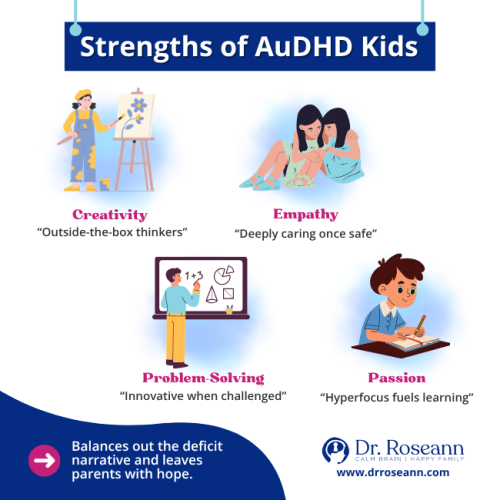
Strengths of AuDHD Kids
It’s easy to get caught up in challenges, but AuDHD also comes with incredible strengths. When we nurture these, kids feel valued for who they are — not just managed for what they struggle with.
- Creativity: Many AuDHD kids think outside the box.
- Empathy: Once they feel safe, they can be deeply compassionate.
- Problem-Solving: Hyperfocus can lead to impressive expertise and innovation.
- Passion: Their enthusiasm for special interests often drives learning and confidence.
STORY (CONTINUATION): For Jonah, his deep passion for dinosaurs became a bridge for learning and connection. Using his interest, we built in math and reading tasks that suddenly felt fun instead of overwhelming.
Highlighting strengths balances the “deficit” narrative and helps kids see themselves as capable and gifted, not broken.

Supporting Parents and Families
Raising an AuDHD child can feel like a full-time job, but you don’t have to do it alone.
- Find parent support groups
- Seek therapies that involve you too
- Give yourself permission to rest
- Celebrate small wins
Therapies and Interventions for AuDHD
There’s no “one-size-fits-all,” but evidence-based and natural supports can help:
- CBT/DBT for emotional regulation
- Occupational therapy for sensory and motor skills
- Speech therapy for communication
- Neurofeedback to retrain brainwave patterns
- PEMF therapy for calming the nervous system
- Supplements (with provider guidance)
- Medication when appropriate
AuDHD and Co-Occurring Conditions
AuDHD rarely exists in isolation. Many kids face additional challenges that intensify struggles.
Common Co-Occurring Challenges
- Anxiety: Worry, panic, or refusal in stressful situations
- Obsessive-Compulsive Disorder (OCD): Intrusive thoughts and compulsive behaviors
- Mood Disorders: Irritability or depression linked to chronic overwhelm
- Learning Disabilities: Dyslexia, dysgraphia, dyscalculia
- PANS/PANDAS: Sudden onset of anxiety, tics, or OCD-like symptoms
Why Early Identification Matters
Co-occurring issues can block progress if left unrecognized. Comprehensive evaluation helps uncover hidden challenges so interventions address the whole child.
Practical Tips for Home and School
At Home
- Create a calm-down corner with sensory tools
- Use visual checklists for routines
- Break tasks into mini-steps
- Plan sensory breaks throughout the day
- Keep routines predictable but allow small choices
At School
- Request IEP/504 accommodations
- Build in sensory-friendly breaks
- Ask for clear, written instructions
- Set realistic expectations
- Stay in close parent-teacher communication
Long-Term Outlook and Hope
AuDHD isn’t something kids outgrow, but with support, they can thrive in every stage of life.
- School: Many flourish when their learning needs are understood.
- Careers: Adults often find meaningful work in fields that value creativity and deep focus.
- Relationships: With safe co-regulation and support, they can form strong, lasting connections.
STORY (CONTINUATION): Jonah’s mom once told me, “For the first time in years, I feel hopeful about his future.” That’s the shift I want every parent to experience — knowing that growth is lifelong, regulation is possible, and your child’s story is still unfolding.
The bottom line: growth is lifelong, regulation is possible, and your child’s story is still unfolding. With consistent support and a focus on strengths, kids with AuDHD don’t just survive — they thrive.
AuDHD may feel overwhelming at times, but please remember: your child is not broken. Their brain simply works differently, and with the right supports, they can flourish.
You are not alone in this journey. The more you understand AuDHD, the more equipped you’ll be to advocate for and support your child.
FAQs about AuDHD
Is AuDHD a real diagnosis?
While AuDHD isn’t an official DSM label, it’s widely recognized in clinical practice and research.
Can a child outgrow AuDHD?
No, but symptoms can improve with support, therapy, and regulation strategies.
What’s the best therapy for AuDHD?
It depends on the child. Most benefit from a mix of brain-based, behavioral, and sensory therapies.
How common is AuDHD?
Studies suggest that 30–50% of people with autism also meet ADHD criteria, and vice versa.
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!










