Understanding the difference between typical childhood “moody” behavior and signs of a real mood disorder can feel overwhelming for parents. Some kids are naturally more rigid or negative — that “glass half empty” wiring — while others go through emotional phases as they grow.
But when your child's moods become persistent, intense, or interfere with daily life, it’s time to take a closer look. This guide will help you spot the signs, understand the types of mood disorders, and know when and how to get help.
What Are Mood Disorders?
Mood disorders are clinical conditions where a person struggles to regulate emotions in a typical, healthy way. These are not personality flaws or “bad behavior” — they are signs that a child's nervous system is overwhelmed and needs support.
Mood disorders include persistent sadness, irritability, intense highs and lows, or a loss of interest in everyday activities. Symptoms can look very different between children, with some turning inward (withdrawal, sadness) and others acting outwardly (anger, aggression).
“Mood disorders in children often show up as behavior problems before emotional symptoms are even recognized.” — Dr. Roseann Capanna-Hodge
Mood Dysregulation Spectrum: Internalizing vs. Externalizing Symptoms
| Symptom Type | Internalizing Symptoms | Externalizing Symptoms |
|---|---|---|
| Emotional Signs | Sadness, hopelessness, withdrawal | Anger, irritability, aggression |
| Behavioral Signs | Social withdrawal, tearfulness | Tantrums, defiance, impulsivity |
| Physical Signs | Fatigue, appetite changes, sleep problems | Risk-taking behaviors, hyperactivity |
What Are the Types of Mood Disorders Diagnosed in Children?
Several specific types of mood disorders can affect children and teens, each presenting with its own unique pattern of symptoms and challenges.
Understanding the distinctions between these disorders is crucial because it allows parents, educators, and clinicians to tailor interventions that truly address the child's needs.
Early recognition of the specific mood disorder type can lead to more effective support, targeted therapies, and better long-term outcomes for children struggling with emotional regulation and mental health challenges.
Key Features of Mood Disorders In Children
| Mood Disorder | Key Features |
|---|---|
| Major Depressive Disorder | Persistent sadness, hopelessness, withdrawal |
| Persistent Depressive Disorder | Chronic, low-grade depression for over a year |
| Bipolar Disorder | Cycles of intense highs (mania) and lows (depression) |
| Disruptive Mood Dysregulation Disorder | Severe, frequent temper outbursts, ongoing irritability |
| Premenstrual Dysphoric Disorder | Severe mood changes before menstruation |
| Mood Disorder from Medical Condition | Depression linked to illness (e.g., concussion, chronic disease) |
| Substance-Induced Mood Disorder | Mood symptoms caused by substance use or medication |
“Early identification and intervention are key — children do not simply ‘grow out' of mood disorders without support.” — Dr. Joan Luby
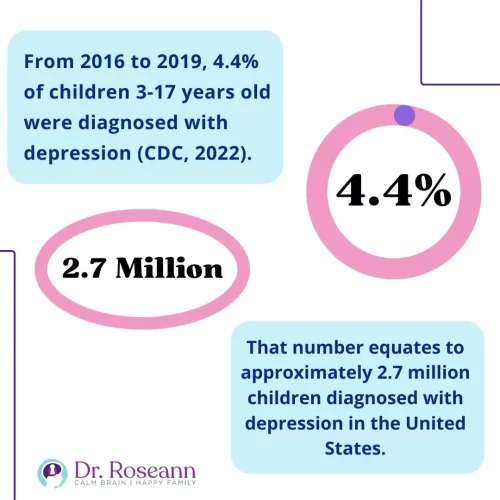
What Are the Statistics on Depression in Children?
Depression and mood disorders are far more common among children and adolescents than most parents realize — and the rates continue to rise at an alarming pace.
Increased awareness is critical because early intervention can dramatically change the trajectory of a child's emotional health.
Understanding these trends helps parents, educators, and clinicians recognize that mood challenges are not isolated or rare, but part of a broader mental health crisis affecting our youth today.
- 4% of U.S. children aged 3-17 were diagnosed with depression (CDC, 2022).
- 1% of adolescents reported a major depressive episode (CDC, 2022).
- 36.7% battled persistent sadness and hopelessness in 2018-2019.
The COVID-19 pandemic intensified mental health challenges:
| Statistic | Before Pandemic | During Pandemic |
|---|---|---|
| Suicide Attempts in Girls (12–17 yrs) | Baseline | Up 50.6% |
| Suicide Attempts in Boys (12–17 yrs) | Baseline | Up 3.7% |
What Are the Symptoms of Mood Disorders in Children and Teens?
Recognizing mood disorder symptoms in children and teens can be tricky and often requires a keen and compassionate eye.
Unlike adults, young people typically lack the emotional vocabulary or self-awareness to verbalize feelings like sadness, hopelessness, or anxiety.
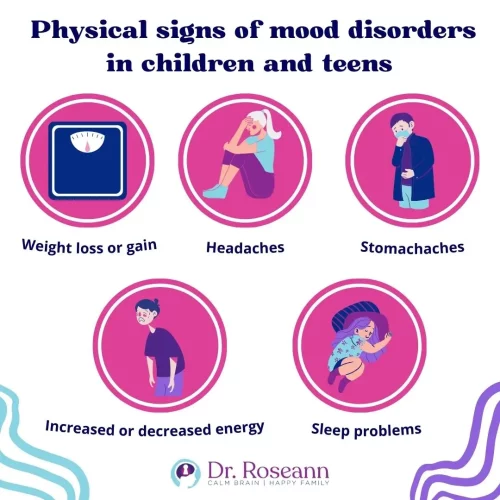
Instead, they tend to express their internal struggles through changes in behavior, declines in academic performance, withdrawal from social activities, or even unexplained physical complaints like stomachaches and headaches.
Understanding these indirect signals is crucial for early identification and intervention, helping to prevent deeper emotional struggles from taking root.
“Children often express depression through irritability and somatic complaints rather than through sadness alone.” — Dr. Mary Fristad
Symptoms of Major Depressive Disorder in Children
| Emotional Signs | Behavioral Signs | Physical Signs |
|---|---|---|
| Irritability | Loss of interest in friends or activities | Sleep changes |
| Persistent sadness | School avoidance or declining grades | Headaches, stomachaches |
| Feelings of hopelessness | Withdrawal from family or friends | Appetite changes |
Symptoms of Major Depressive Disorder in Teens
In addition to the signs above, teens may:
- Engage in risky behavior
- Have frequent angry outbursts
- Experience deep fatigue
- Struggle with decision making
- Withdraw socially
- Exhibit suicidal thoughts or self-harm
Typical Moodiness vs. Childhood Depression
| Typical Moodiness | Childhood Depression |
|---|---|
| Upset about specific events (e.g., bad grade, argument) but recovers quickly | Persistent sadness or irritability lasting weeks or longer |
| Occasional complaints about boredom or frustration | Loss of interest in activities once enjoyed |
| Sleep and appetite mostly stable | Significant changes in sleep and appetite |
| Mood improves with positive events (e.g., fun activities) | Mood remains low even during enjoyable activities |
| Normal ups and downs with development | Mood symptoms interfere with daily life, friendships, or school |
Diagnosing Mood Disorders in Children
A proper diagnosis is essential — but diagnosing children requires a thoughtful, thorough process that goes beyond a single office visit.
It involves gathering information from parents, teachers, and caregivers, observing the child in different environments, and sometimes using standardized assessments to paint a complete picture of the child's emotional and behavioral functioning.
Mood disorders can look very different from one child to another, so a multi-faceted evaluation is key to ensuring that children receive an accurate diagnosis and the right kind of help early on.
Common Diagnostic Tools to Assess Mood Disorders
| Tool | Purpose |
|---|---|
| BDI | Measures depressive symptoms |
| BASC | Multidimensional assessment from parent, teacher, and child |
| CDRS | Rates depression severity |
| CDI | Child’s self-reported depressive symptoms |
| Patient Health Questionnaire-9 | Screens depression in teens |
| CES-DC | Depression scale for children |
A child may smile on the outside but struggle deeply on the inside — that's why thorough evaluation is key.” — Dr. Roseann Capanna-Hodge
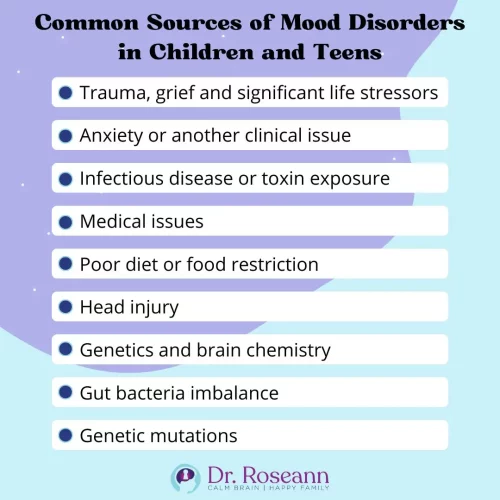
Causes of Mood Disorders in Children and Teens
There’s rarely a single cause behind a mood disorder. Instead, it's often a combination of biological, psychological, environmental, and lifestyle factors that gradually overwhelm a child’s emotional regulation system.
Understanding the possible roots of your child's struggles helps you find the most effective, targeted interventions — and it can also reduce guilt and confusion for parents.
Causes of Mood and Depression Disorders
| Cause | How It Affects Mood |
|---|---|
| Trauma or loss | Triggers emotional dysregulation and persistent sadness |
| Chronic stress (e.g., bullying) | Exhausts coping mechanisms, increases cortisol |
| Anxiety disorders | Long-term hypervigilance can lead to burnout and depression |
| Infections/toxin exposure | Can trigger neuroinflammation affecting mood regulation |
| Poor nutrition/gut imbalance | Disrupts neurotransmitter production (e.g., serotonin) |
| Genetic predisposition | Increases baseline risk but environment can influence outcomes |
The Gut-Brain Connection and Mood
Many parents are surprised to learn that 90–95% of the body's serotonin — a key neurotransmitter for mood regulation — is actually produced in the gut, not the brain.
A disrupted gut microbiome (gut dysbiosis) can reduce serotonin levels, increase systemic inflammation, and worsen emotional regulation.
Supporting gut health isn't just about digestion — it's critical for mental health too.
Ways to improve the gut-brain connection:
- Reducing sugar and processed foods
- Using targeted probiotics
- Eating anti-inflammatory diets (like Mediterranean or Paleo-style)
- Addressing food sensitivities
Mood and Autism
Children on the autism spectrum are at significantly higher risk for developing mood disorders like anxiety and depression.
Their brains are often wired for sensory sensitivity, rigid thinking, and low frustration tolerance, which — without proper support — can spiral into chronic emotional distress.
Challenges that can lead to mood issues in kids with autism:
- Sensory Overload: Triggers emotional shutdown or meltdowns
- Difficulty with Change: Increases anxiety and rigid behaviors
- Social Struggles: Loneliness and peer rejection can fuel sadness
- Communication Barriers: Makes it harder to express distress
Without explicit teaching of coping skills and problem-solving strategies, kids with autism are simply more vulnerable to developing mood dysregulation over time.
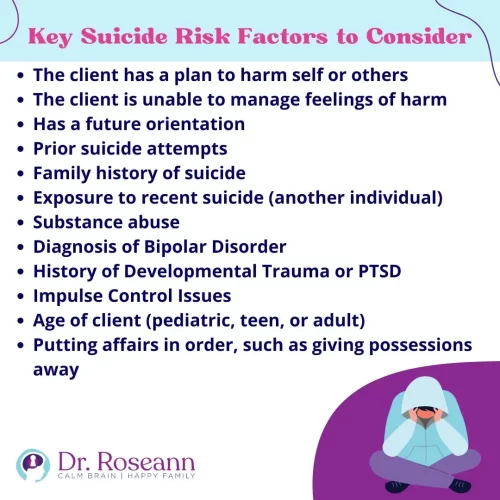
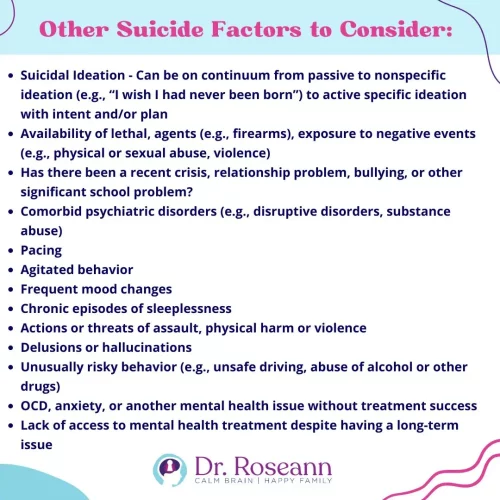
Suicide and Depression in Youth
The link between untreated depression and suicide is tragic but very real.
Suicide is now the second leading cause of death among adolescents aged 10–24, according to the CDC.
Key Risk Factors for Youth Suicide:
| Risk Factor | Why It Matterd |
|---|---|
| Prior suicide attempt | Strong predictor of future attempts |
| Family history of suicide | Increases risk through genetics and modeling |
| Exposure to bullying, trauma, or abuse | Significantly worsens emotional resilience |
| Untreated mood or anxiety disorders | Leaves emotional pain unaddressed |
| Substance use | Impairs judgment and increases impulsivity |
| Lack of mental health support | Barriers to help can escalate hopelessness |
Warning Signs of Suicide in Teens
- Talking about death or expressing hopelessness
- Giving away possessions
- Acting recklessly or withdrawing completely
- Dramatic mood swings
- Sudden calmness after severe distress (a red flag for a decision to attempt suicide)
Treatment for Mood Disorders in Children
The most effective treatments for mood disorders focus on calming the brain first, then building emotional and behavioral skills over time.
Medication may be part of the plan — but it should never be the only plan.
Evidence-Based Treatments for Depression Disorder:
| Treatment | How It Helps |
|---|---|
| Neurofeedback | Regulates brainwaves, reducing anxiety, depression, and irritability |
| PEMF Therapy | Decreases inflammation and improves cellular communication |
| Therapeutic nutrition | Supports neurotransmitter balance and reduces inflammation |
| Targeted supplements | Leaves e.g., Magnesium, Omega-3s) Nourish the nervous system |
| CBT/psychotherapy | Builds coping skills and rewires negative thought patterns |
| Parent coaching | Strengthens co-regulation and emotional modeling at home |
Key Principle: Calm the brain first → Teach coping skills second → Build resilience long-term.
“We must shift from symptom-masking to brain-healing in treating children's mental health challenges.” — Dr. Thomas Insel, Former Director of NIMH
What Parents Should Do to Help a Moody or Depressed Child
Helping a child with mood struggles isn’t about fixing their emotions — it’s about being a steady, calming presence they can rely on.
When children are overwhelmed, they need to “borrow” a caregiver’s calm to help regulate their own nervous system.
Your role is to create emotional safety:
- Stay calm, even when they can’t.
- Validate their feelings before problem-solving.
- Model healthy coping skills over time.
Healing happens through connection, co-regulation, and small, consistent moments of support — not through pressure or punishment.
Supportive Things to Say to a Child with Mood Struggles
- “I can see you’re having a hard time. I'm here for you.”
- “It’s okay to feel what you’re feeling. We’ll work through it together.”
“You’re not alone — and there is help.”
FAQs About Mood Treatment for Children
1. How long does it take to see improvements?
Small changes can appear in a few weeks. Lasting change often takes 6–12 months of consistent support.
2. Can mood disorders be misdiagnosed?
Yes — that's why it's critical to work with professionals experienced in pediatric mood and nervous system issues.
3. What’s the difference between mood swings and mood disorders?
Mood swings are short-term and situational. Mood disorders are persistent, intense, and impair functioning.
4. Are natural treatments enough for mood issues?
Sometimes! Brain-based therapies, nutrition, sleep, and lifestyle changes can make a huge difference — especially when caught early.
5. Should I talk to my child's school?
Yes. Schools can offer accommodations and emotional support plans that make a big difference.
Citations:
American Psychological Association. (n.d.). Beck Depression Inventory (BDI). American Psychological Association. Retrieved June 22, 2022, from https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/beck-depression
Centers for Disease Control and Prevention. (2021, June 17). Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic – United States, January 2019–May 2021. Centers for Disease Control and Prevention. Retrieved June 22, 2022, from https://www.cdc.gov/mmwr/volumes/70/wr/mm7024e1.htm
Centers for Disease Control and Prevention. (2022, April 13). Anxiety and depression in children: Get the facts. Centers for Disease Control and Prevention. Retrieved May 16, 2022, from https://www.cdc.gov/childrensmentalhealth/features/anxiety-depression-children.html
Development and applications of the BASC-3 family of … – txasp.org. (n.d.). Retrieved June 22, 2022, from https://www.txasp.org/assets/conference-materials/2015/basc-3%20three%20hour%20powerpoint.pdf
DiMaria, L. (2020, October 3). Benefits and limitations of the Children's Depression Inventory. Verywell Mind. Retrieved June 22, 2022, from https://www.verywellmind.com/the-childrens-depression-inventory-cdi-1066780
Kluwer, W. (n.d.). Measures used to monitor clinical improvement of depressive symptoms and global functioning in depressed children and adolescents. UpToDate. Retrieved June 22, 2022, from https://www.uptodate.com/contents/image/print?imageKey=PEDS%2F70455&topicKey=PSYCH%2F1231&source=see_link
Lee, H. J., Kim, S. H., & Lee, M. S. (2019). Understanding mood disorders in children. In Y. K. Kim (Ed.), Frontiers in psychiatry (Vol. 1192, pp. 267–280). Springer. https://doi.org/10.1007/978-981-32-9721-0_12
Shanahan, K. M., Zolkowski-Wynne, J., Coury, D. L., Collins, E. W., & O'Shea, J. S. (1987). The Children's Depression Rating Scale for normal and depressed outpatients. Clinical Pediatrics, 26(5), 245–247. https://doi.org/10.1177/000992288702600506
Stanford Children's Health. (n.d.). Mood disorders in children and adolescents. Lucile Packard Children's Hospital Stanford. Retrieved May 18, 2022, from https://www.stanfordchildrens.org/en/topic/default?id=overview-of-mood-disorders-in-children-and-adolescents-90-P01634
The Children's Hospital of Philadelphia. (2014, August 24). Mood disorders in children and adolescents. Children's Hospital of Philadelphia. Retrieved June 22, 2022, from https://www.chop.edu/conditions-diseases/mood-disorders-children-and-adolescents
The Recovery Village Drug and Alcohol Rehab. (2021, July 1). Mood disorders in children: Types and symptoms. The Recovery Village. Retrieved May 18, 2022, from https://www.therecoveryvillage.com/mental-health/mood-disorders/mood-disorders-in-children/
Types of mood disorders in children. (n.d.). Patient Care at NYU Langone Health. Retrieved May 18, 2022, from https://nyulangone.org/conditions/mood-disorders-in-children/types
U.S. Department of Health and Human Services. (n.d.). Disruptive mood dysregulation disorder: The basics. National Institute of Mental Health. Retrieved May 18, 2022, from https://www.nimh.nih.gov/health/publications/disruptive-mood-dysregulation-disorder
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
© Roseann-Capanna-Hodge, LLC 2025