Estimated reading time: 12 minutes
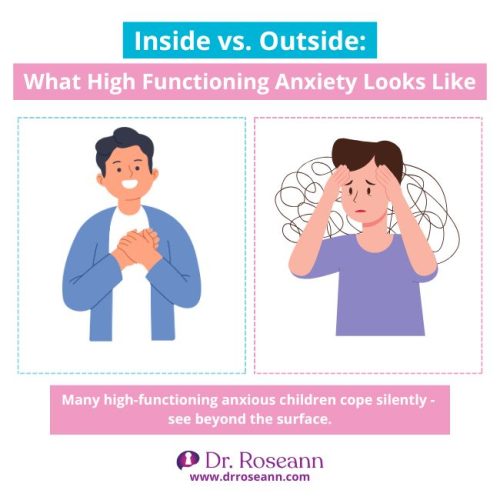
When your teen seems fine on the outside but is crumbling on the inside… It’s more than just stress.
High-functioning anxiety is one of the most misunderstood struggles, especially in kids who look like they’re doing okay. But behind the straight A’s, perfectionism, or people-pleasing can be a child stuck in overdrive, quietly battling worry and overwhelm.
In this blog, we’re pulling back the curtain on what’s really going on in your child’s brain and how you can help them find calm, confidence, and relief.
What you’ll learn:
- How to recognize the hidden signs of high-functioning anxiety in teens
- What this has to do with nervous system dysregulation (and why that matters)
- Simple, real-life ways to support your child without walking on eggshells
- Why it’s not your fault—and how healing is possible
Because once you understand what’s really going on under the surface, everything changes.
What is High Functioning Anxiety in Kids and Teens?
High functioning anxiety isn’t an official diagnosis, it’s when kids or teens excel at school, sports, or activities, yet internally wrestle with unrelenting worry and fear.
Outwardly, they’re the “ideal child”: organized, polite, high-achieving and yet inside?
Racing heart, perfectionism, and endless mental pressure.
For example:
Cristy’s daughter, 15, never missed a homework deadline. She volunteered, led her study group, and smiled through it all. But Cristy noticed she flinched when asked a spontaneous question and always felt “on edge.” That’s the hallmark: calm on the surface, chaos underneath.
Why this matters:
Understanding high functioning anxiety shifts the narrative from “lazy” or “dramatic” to “This is a dysregulated brain in action, not bad parenting.” When we say, “Let’s calm the brain first,” it roots your approach in compassion and practical support.
What are the Symptoms of High Functioning Anxiety?
Kids with high functioning anxiety show symptoms in three main areas:
Physical symptoms
High-functioning anxiety doesn’t just live in your teen’s head—it shows up in the body, too.
Common physical signs of high-functioning anxiety in teens include:
- Stomachaches, especially before school or social events
- Headaches that come and go without a medical cause
- Tight muscles or body tension, even when resting
- Racing heart or palpitations during transitions or pressure
- General fatigue or feeling “off” without a clear reason
You might hear your child say things like, “My stomach always hurts in the morning,” or “I don’t feel right, but I don’t know why.” These are not just excuses—they’re real, physical signs of a dysregulated nervous system that needs support.
Emotional symptoms
While they may seem mature or even “on top of things,” teens with high-functioning anxiety are often fighting a silent emotional battle beneath the surface. Their minds are stuck in a cycle of overthinking, self-criticism, and fear of falling short.
Common emotional symptoms of high-functioning anxiety include:
- Excessive worry about the future, performance, or social acceptance
- Constant “what-if” thinking (e.g., What if I fail? What if they don’t like me?)
- Harsh self-talk and overreaction to even small mistakes
- Perfectionism that drives them to overwork and avoid failure
- Fear of disappointing others, even when expectations aren’t realistic
- Chronic self-doubt, often masked by outward success or compliance
Behavioral symptoms
On the outside, teens with high-functioning anxiety often appear like model students—organized, responsible, and always striving to please. But beneath that polished surface is a nervous system working overtime just to feel safe and in control.
Common behavior patterns include:
- Overachieving in school or activities to avoid criticism or failure
- Perfectionistic tendencies, like overplanning or obsessing over details
- People-pleasing to gain approval and avoid conflict
- Avoidance of uncertainty, change, or anything that feels uncomfortable
- Micromanaging daily tasks to reduce anxiety—even if it drains them
- Suppressing their own needs to maintain peace at home or school
While these behaviors may seem like strengths, they’re often driven by fear. Over time, this constant need to stay “on” can lead to emotional burnout—for your child and for you.

What is the Difference Between High Functioning Anxiety and Typical Anxiety?
Both stem from similar underlying stress, but they present differently in how individuals cope.
Understand the differences below:
| Triggers | Often driven by perfectionism, fear of failure, and a high need for control. | Triggered by identifiable stressors or irrational fears. |
| Signs & Symptoms | - Excessive worry - Restlessness and overthinking - Irritability, tension, and difficulty relaxing - Achieving goals despite anxiety - Physical symptoms: headaches, muscle tension, fatigue |
- Panic attacks or overwhelming fear - Avoidance of anxiety -provoking situations - Excessive sweating, trembling, or heart palpitations - Difficulty concentrating - Physical symptoms: nausea, dizziness, shortness of breath |
| Impact on Daily Life | - Can appear highly successful and organized - May struggle privately with exhaustion and overwhelm - Difficulty enjoying achievements due to constant worry - Reluctance to seek help, as anxiety seems manageable |
- May avoid responsibilities or situations due to intense fear - Visible impact on relationships, work, and social life - More likely to seek help due to visible distress and disruption - Reduced quality of life due to persistent and unmanageable anxiety |
| Common Triggers | - High expectations, both self-imposed and external - Fear of judgment or failure - Significant life changes or responsibilities |
- Specific phobias (e.g., flying, heights) - Social situations - Stressful life events or trauma |
Is There Any High Functioning Anxiety Test?
There’s no official “high functioning anxiety test,” but screening tools can help reveal anxiety patterns:
- Pediatric Symptom Checklist (PSC-17) for internalizing concerns
- Spence Children’s Anxiety Scale (SCAS) details anxiety types in kids aged 8–15
- Generalized Anxiety Disorder 7-item (GAD‑7) for adolescents
Important: These tools are friendly warnings, not diagnoses. If results suggest concern, share them with your pediatrician or psychologist to explore next steps.
Is High Functioning Anxiety Related to Dysregulation?
Yes, it absolutely connects. Dysregulation means the brain is stuck in “fight-flight-freeze,” unable to self-soothe. In high functioning anxiety, it’s masked, the child stays productive but remains constantly activated inside.
When we spot tension before a test or inability to unwind, that is dysregulation showing up. Recognizing it lets us respond with calm strategies, not punish or demand.
Takeaway: Behavior is communication. Masked perfectionism is dysregulation asking for rest and safety.
How to Manage High Functioning Anxiety in Teens and Children
1. Therapy
Evidence-based therapy is often the first and most effective step.
- Cognitive Behavioral Therapy (CBT) helps teens identify anxious thought patterns and reframe them. For example, a child who believes, “If I don’t get an A, I’m a failure” learns to replace that thought with, “Trying my best matters more than perfection.”
- Programs like Coping Cat and the C.A.T. Project are specifically designed for kids and teens with anxiety. They use fun, structured lessons to teach real-world coping skills—so your child not only feels calmer, but also more confident.
📚 Research shows that CBT is highly effective in reducing anxiety symptoms in adolescents (Walkup et al., 2008).
2. Mindfulness & Routine
When we calm the nervous system, we create space for healing.
- Simple tools like deep breathing, 5-4-3-2-1 grounding, and mindful movement help shift the brain out of fight-or-flight and into rest mode.
- Digital boundaries, like turning off screens an hour before bed, support better sleep and reduce overstimulation.
- Daily rhythm matters: consistent sleep, nourishing meals, and regular physical activity (even a 15-minute walk) lower stress hormones like cortisol.
- A 5-minute gratitude practice or journal check-in can rewire the brain toward resilience and optimism.
3. Medication
While not always necessary, medication—usually SSRIs—may be appropriate if:
- Anxiety symptoms are severe or interfering with daily life
- Therapy alone hasn’t helped after a few months
- The teen is experiencing panic attacks or depressive symptoms alongside anxiety
Important: Medication should always be prescribed by a qualified child psychiatrist and paired with therapy for best outcomes.
4. Parental Support
Parents play a crucial role in co-regulating a dysregulated brain.
- Validate first: “I can see this is really hard for you.” Validation calms the nervous system faster than logic.
- Model calm: When your child sees you take a breath or talk kindly to yourself, they learn to do the same.
- Create a “Calm-Down Toolkit” together with your child. Include things like:
- Noise-canceling headphones
- Fidget or sensory tools
- Music playlists or nature sounds
- A favorite scented lotion or essential oil
- Visual calming exercises or guided imagery apps
“It’s not about being perfect—it’s about feeling safe enough to try.”
Let that be your family mantra.
Parent Action Steps
FAQs
What’s the difference between anxiety and dysregulation?
Anxiety is emotional worry; dysregulation happens when the brain is stuck in stress mode physiologically—like shaking alarm bells inside the body.
Can high functioning anxiety lead to burnout?
Yes—without early support, ongoing stress can escalate to exhaustion, mood struggles, or even depression.
When should medication be considered?
When anxiety impairs daily life despite lifestyle and therapy tools—always consult a qualified child psychiatrist.
Citations
- Kendall, P. C., Peterman, J. S., Cummings, C. M., & March, J. S. (2020). Child and adolescent anxiety disorders: Evidence-based treatment and future directions. Journal of Clinical Child & Adolescent Psychology, 49(1), 1–13. https://doi.org/10.1080/15374416.2019.1691714
- Zoogman, S., Goldberg, S. B., Hoyt, W. T., & Miller, L. (2019). Mindfulness interventions with youth: A meta-analysis. Mindfulness, 10(2), 290–302. https://doi.org/10.1007/s12671-018-0978-z
- Walkup, J. T., Albano, A. M., Piacentini, J., Birmaher, B., Compton, S. N., Sherrill, J. T., … & Kendall, P. C. (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359(26), 2753–2766. https://doi.org/10.1056/NEJMoa0804633
Dr. Roseann Capanna-Hodge is a licensed mental health expert that is frequently cited in the media:
- Medium: Elemental The Covid-19 Symptoms No One Talks About: Survivors carry guilt, anxiety, and shame.
- Parade Want to Know How to Overcome Social Anxiety? We’ve got Help!.
- PIX 11 (Video) Election Anxiety
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to provide health advice. It is recommended to consult with a physician before beginning any new wellness program. The effectiveness of diagnosis and treatment varies by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions—so you are in the right place!
©Roseann Capanna-Hodge










