Estimate reading time: 10 minutes
If you’ve watched your child melt down over small things, struggle to calm down after getting upset, or lash out in extreme ways, you’re not alone. Many parents feel helpless when their child’s emotions spiral out of control, affecting everything from family life to school performance.
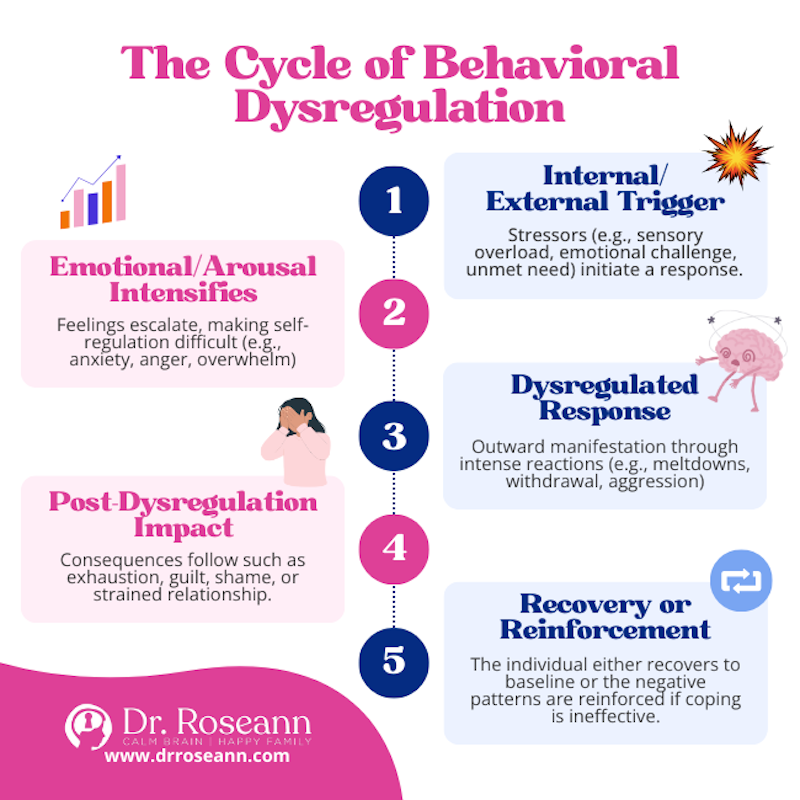
Behavioral dysregulation definition: an inability to control or regulate emotional and behavioral responses, resulting in reactions that are intense, prolonged, and disproportionate to the situation at hand.
Behavioral dysregulation is more than just “bad behavior.” It’s a brain-based symptom where the volume control for emotions doesn’t work properly. Instead of matching their response to the situation, children (and adults) with dysregulation experience emotions at maximum intensity and have trouble dialing them back down.
According to the American Psychological Association, dysregulation involves “any excessive or otherwise poorly managed mechanism or response.” This means the brain’s ability to manage feelings and behaviors isn’t functioning as it should.
What Makes Dysregulation Different From Typical Emotional Ups and Downs
- Intensity – Reactions are much stronger than the situation warrants.
- Duration – Emotions stay heightened long after the triggering event.
- Recovery – Difficulty calming down or returning to a baseline state.
- Impact – Disrupts relationships, school, work, and daily functioning.
Dysregulation can manifest as emotional dysregulation (intense mood swings), behavioral dysregulation (impulsive actions), or autonomic dysregulation (physical symptoms like a racing heart). Often, these overlap.
The good news? Understanding what behavioral dysregulation is represents the first step toward finding effective solutions. Research shows that with the right support, such as Dialectical Behavior Therapy (DBT) and other skill-building strategies, individuals can learn to regulate their emotions more effectively. While it may be linked to conditions like ADHD, Autism Spectrum Disorder, or trauma, dysregulation is treatable.
This guide will walk you through what behavioral dysregulation looks like, why it happens, and what you can do about it.
What Is The Definition of Behavioral Dysregulation?
Understanding the behavioral dysregulation definition is about seeing the gap between an internal feeling and an external action. Imagine an emotional world where the gas pedal is stuck down and the brakes barely work. That’s what dysregulation can feel like.
At its core, dysregulation is a loss of ability to moderate emotional reactions. A response comes on stronger, lasts longer, and feels disproportionate to the event. This disrupts executive functions—the brain skills for planning, focus, and self-control. When emotions take over, clear thinking disappears.
It’s important to know that dysregulation is usually a symptom of an underlying issue, like a mental health condition, a neurodevelopmental difference, or unresolved trauma, not a standalone disorder.
The difference between healthy regulation and dysregulation is clear when compared side-by-side:
| Feature | Healthy Emotional Regulation | Dysregulation |
|---|---|---|
| Emotional Response | Matches the situation’s intensity | Overly intense, disproportionate |
| Duration of Emotion | Recovers relatively quickly | Prolonged, lingers long after the event |
| Behavioral Control | Can choose appropriate responses | Impulsive, difficulty inhibiting maladaptive behaviors |
| Coping Strategies | Uses adaptive, constructive methods | Relies on maladaptive, potentially harmful strategies |
| Impact on Functioning | Maintains daily activities and relationships | Disrupts relationships, work/school, and well-being |
A Clinical Behavioral Dysregulation Definition
The American Psychological Association defines dysregulation as “any excessive or otherwise poorly managed mechanism or response.” In terms of behavior, this appears as poorly managed coping mechanisms. Someone might show explosive anger that doesn’t match the situation or turn to self-harm. These aren’t “bad choices” but maladaptive behaviors that develop without better tools to handle overwhelming emotions. Research on conditions like Borderline Personality Disorder offers valuable insights into these challenges, as detailed in the Components of Emotion Dysregulation in Borderline Personality Disorder: A Review.
The Different Faces of Dysregulation
Dysregulation appears in several overlapping forms:
- Emotional dysregulation: Difficulty managing feelings and the actions they cause. This includes not recognizing, accepting, or having healthy strategies to reduce emotional intensity.
- Autonomic dysregulation: Affects the body’s automatic systems like heart rate and breathing, causing physical symptoms like a racing heart or stomach problems. It’s common in individuals with trauma or ADHD.
- Affect dysregulation: A disconnect between someone’s outward emotional expression and their internal state, such as laughing at sad news.
- Behavioral dysregulation: Emotional struggles translate into problematic actions like self-harm, substance misuse, or explosive anger. These are often misguided attempts to cope with overwhelming feelings.
- Cortisol dysregulation: The body’s stress hormone, cortisol, becomes unbalanced, leading to chronic stress, exhaustion, and other health issues.
What Are The Signs of Behavioral Dysregulation?
Typical childhood meltdowns are one thing, but dysregulation feels different. The reactions are bigger, last longer, and seem to come from nowhere. Recognizing dysregulation means observing consistent patterns of intense, prolonged, and disproportionate emotional responses that impact daily life.
Common signs of behavioral dysregulation include:
- Impulsivity: Acting before thinking, taking risks, or struggling to pause once emotions run high.
- Mood swings: Fast, intense shifts between joy, sadness, or anger that seem to come out of nowhere.
- Relationship difficulties: Frequent conflicts, misunderstandings, and unstable connections with others.
- Perfectionism: Rigid standards that trigger frustration, shame, or shutdown when things aren’t “just right.”
- Avoidance: Skipping situations, people, or tasks that might stir up strong feelings (Sharpe et al., 2022).
- Aggression: Verbal outbursts, physical aggression, or persistent irritability that feels hard to rein in.
- Self-harm: Using behaviors like cutting or hitting oneself to release or numb overwhelming emotion.
- Substance use: Turning to alcohol or drugs to blunt distress or cope with intense states.
Parent story:
I remember Luca’s story, Maria’s 8-year-old son who came home from school one afternoon. She simply asked him to wash his hands before snack—something he’d done for years without issue. Instead, he collapsed to the floor screaming, shaking, and unable to explain what was wrong.
Even after she dimmed the lights and held him gently, he stayed overwhelmed for nearly 30 minutes until he finally whispered, “I don’t know why I got so upset… my brain just got loud.”
In that moment, Maria realized this wasn’t a typical bad mood or big feeling; it was dysregulation—his nervous system simply couldn’t reset without support.

Behavioral Dysregulation in Children
In children, dysregulation can be confusing and is often mistaken for being “difficult.” Their brains haven’t fully developed regulation skills, leading to specific behaviors:
- Extreme impatience: An inability to wait that leads to immediate outbursts.
- Disproportionate anger or upset: Intense reactions to minor inconveniences, like a toy breaking or a change in plans.
- Inconsistent, unstructured outbursts: Meltdowns that seem to come from nowhere, are hard to de-escalate, and continue long after the trigger is gone.
- Difficulty with transitions: Significant distress when moving from one activity to another.
- Refusing to speak or make eye contact: Withdrawing completely as a coping mechanism when overwhelmed.
Research confirms that children with dysregulation show these patterns and often need specialized support.
Behavioral Dysregulation in Teenagers and Adults
In teenagers and adults, dysregulation often transforms into more complex, internalized patterns:
- Intense anxiety in relationships: Constant worry about abandonment, extreme jealousy, or difficulty trusting others.
- Trouble with conflict resolution: Disagreements quickly escalate into destructive arguments.
- Social withdrawal: Avoiding social situations due to fear of rejection or emotional overwhelm.
- Negative self-perception: Persistent feelings of worthlessness, self-hatred, or shame.
- Over- or under-eating: Using food to cope with emotional distress.
- Risky behaviors: Impulsive sexual activity, reckless driving, or other dangerous actions to seek stimulation or escape pain.
These patterns can significantly impact a person’s ability to maintain jobs, succeed academically, and form healthy relationships. Recognizing these signs is the first step toward getting help.
The Root Causes: Why Does Behavioral Dysregulation Happen?
Dysregulation rarely has a single cause. It typically emerges from a combination of factors, including inborn traits, life experiences, and learned behaviors. Some children are born with brains wired to feel emotions more intensely. When combined with challenging experiences or a lack of coping tools, dysregulation can develop. Understanding these root causes helps pinpoint the most effective ways to help.
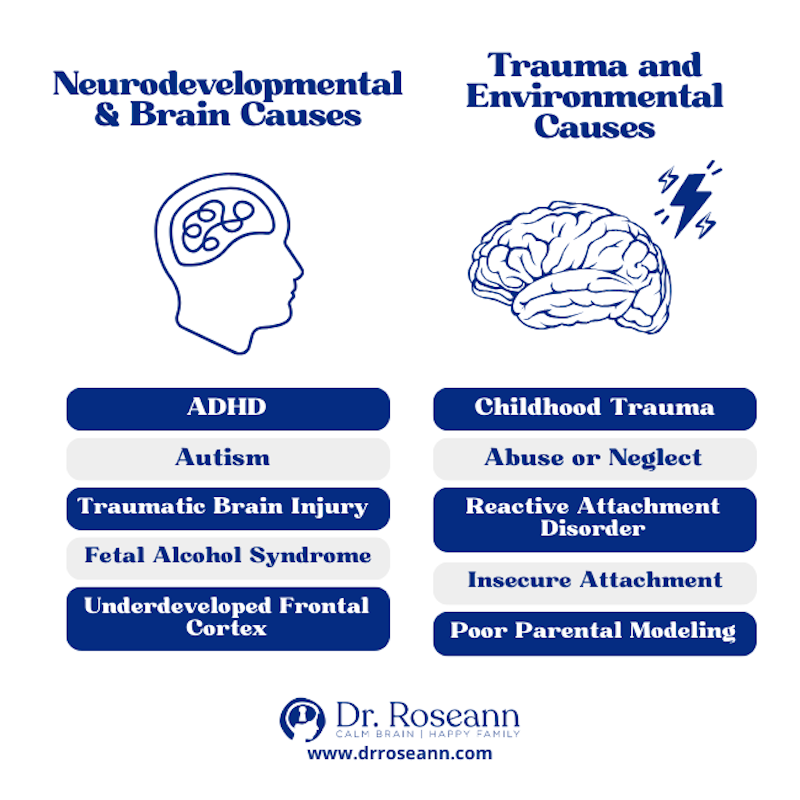
Key contributors include neurodevelopmental factors, brain function, environmental influences, genetic predisposition, and learned behavior.
Neurodevelopmental and Brain Factors
The brain’s architecture plays a major role in emotional regulation. Differences in brain development or function can make managing emotions much harder.
- ADHD: This is one of the most common conditions linked to dysregulation. Individuals with ADHD often experience emotions more and have difficulty calming down (Retz et al., 2014).
- Autism Spectrum Disorder (ASD): Challenges with identifying and expressing emotions, combined with sensory sensitivities, can quickly lead to overwhelm and distress.
- Traumatic Brain Injury (TBI): Injury to the brain, especially the frontal regions responsible for impulse control, can fundamentally change how a person regulates emotions.
- Fetal Alcohol Syndrome: Alcohol exposure before birth can cause lasting changes to brain structure, making emotional and behavioral regulation a lifelong challenge.
- Frontal Cortex: This area acts as the brain’s executive control center. When it develops differently or doesn’t function optimally, emotional regulation is often impaired.
Trauma and Environmental Influences
Our experiences, especially early ones, are powerful in shaping our ability to handle emotions.
- Childhood Trauma: Abuse or neglect can alter brain development, particularly the stress response system, making it harder to cope with everyday challenges (Dunn et al., 2018).
- Abuse or Neglect: Children who experience maltreatment miss critical opportunities to learn healthy coping skills, instead learning that the world is unsafe.
- Reactive Attachment Disorder: This develops when infants fail to form healthy attachments to caregivers, often due to severe neglect, making it incredibly difficult to learn emotional regulation.
- Insecure Attachment: When caregivers are inconsistent or emotionally unavailable, children don’t learn to trust that comfort is available, which can affect emotional stability into adulthood.
- Parental Modeling: Children learn by watching. If parents model poor emotional control, children often adopt these patterns. This is not about blame but about recognizing that regulation is often a family challenge.
Associated Conditions and Impact on Daily Life
Understanding the behavioral dysregulation definition reveals its wide-ranging effects. Dysregulation creates a ripple effect that impacts mental health, relationships, school, work, and overall well-being. It’s a significant risk factor, signaling a vulnerability to other mental health challenges. Daily tasks can feel monumental when emotions are overwhelming and behaviors are unpredictable.
The impact shows up in areas like:
- Social functioning: Difficulty in social situations due to unpredictable reactions.
- Academic and work performance: Suffering due to emotional outbursts or an inability to focus.
- Relationship strain: The people closest to us often bear the brunt of emotional storms.
This culminates in a lower quality of life, not from a lack of effort, but because the internal regulation system needs support.
Mental Health Disorders Linked to Dysregulation
Emotional dysregulation is a core symptom or feature of many mental health and neurodevelopmental conditions.
- Borderline Personality Disorder (BPD): Characterized by intense emotional instability, impulsivity, and unstable relationships rooted in dysregulation.
- Bipolar Disorder: Involves significant mood swings, with difficulty regulating the intensity and duration of emotional states.
- Disruptive Mood Dysregulation Disorder (DMDD): A childhood disorder defined by chronic irritability and frequent, intense temper outbursts.
- Complex PTSD (C-PTSD): Arises from prolonged trauma and involves severe emotional dysregulation.
- Anxiety and Depressive Disorders: Can involve heightened emotional reactivity to stressors and difficulty reducing anxiety or lifting out of depressive states.
- Eating Disorders: Behaviors like bingeing or restricting are often used as maladaptive ways to manage overwhelming emotions.
- ADHD: Commonly involves emotional dysregulation, with more intense and longer-lasting emotional reactions.
- Autism Spectrum Disorders (ASD): Presents unique regulation challenges, often due to sensory sensitivities and difficulty with emotional expression.
- Substance Use and Alcohol Use Disorders: Often linked to dysregulation, as individuals may self-medicate to numb emotional pain.
The Impact on Relationships and Family
Dysregulation is often most painfully felt in close relationships. Unpredictable and intense responses can lead to:
- Frequent arguments: Minor disagreements can quickly escalate into major conflicts.
- Poor boundaries: Difficulty setting or respecting limits can lead to codependency or conflict.
- Empathy challenges: When consumed by one’s own distress, it can be hard to perceive or respond to the emotions of others.
- Intimacy issues: Fear of rejection and mood swings make it difficult to form deep, vulnerable connections.
For parents, raising a child with dysregulation can lead to burnout and stress. The parent-child dynamic is a two-way street; while a hostile environment can contribute to a child’s regulation problems, a child’s dysregulation can also strain a parent’s ability to remain calm and affectionate (Lavi et al., 2021).
Understanding these impacts is crucial. Dysregulation is not a character flaw but a treatable condition that responds to support and intervention.
Building Resilience: Strategies and Treatments
Understanding the behavioral dysregulation definition is the hopeful first step on a journey toward balance. Dysregulation is not a life sentence; it’s a challenge that responds to support, skill-building, and professional intervention. Learning to regulate emotions is like learning a new language—it takes time and practice, but it is achievable.
Professional Treatment Options
Professional help is often the smartest move. Here are some effective approaches:
- Psychotherapy: Talk therapy helps individuals explore the drivers of their emotional struggles and create space for new, healthier patterns.
- Cognitive Behavioral Therapy (CBT): A practical, skills-based approach that teaches individuals to identify, challenge, and reframe the negative thoughts that fuel intense emotions.
- Dialectical Behavior Therapy (DBT): Highly effective for severe dysregulation, DBT teaches four key skills: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. The goal is to find a “Wise Mind” balance between emotion and logic. You can learn more about emotion regulation in therapy here.
- Parent training programs: These programs are game-changers, equipping parents with specific strategies to validate emotions, set boundaries, and co-regulate with their child, improving the entire family dynamic.
- Medication: While not a cure for dysregulation itself, medication can treat underlying conditions like ADHD, anxiety, or depression. This can lower the overall emotional intensity, making it easier to practice new skills.
Practical Coping Skills for Families
Daily routines and coping skills create a foundation for regulation. Here are some practical strategies:
- Mindfulness and deep breathing: Simple practices like deep belly breaths can send a calming signal to the nervous system, interrupting an escalating emotional response.
- Journaling: Writing or drawing feelings provides a safe outlet for intense emotions and can help identify triggers over time.
- Routines: Predictable schedules for meals, bedtime, and transitions provide a sense of safety that anxious nervous systems crave.
- Regular exercise: Physical activity burns off stress hormones, boosts mood, and provides a healthy outlet for intense energy.
- Building emotional literacy: Help your child name their feelings. You can’t regulate what you can’t identify. Start with simple labels like “frustrated” or “disappointed.”
- Validation: Acknowledge your child’s emotion, even if you don’t agree with their behavior. Saying “I can see you’re really angry” helps them feel understood, which is the first step to calming down.
- Modeling healthy regulation: Children learn by watching you. When you model taking deep breaths, talking about your feelings, and using healthy coping strategies, you are teaching them how to do the same.
Going back to Luca and Maria’s experience:
After her realization with Luca, Maria shifted her focus to supporting Luca’s nervous system, not just his behavior.
She built simple routines—two minutes of breathing after school, a quiet snack spot, and a visual schedule to ease transitions.
When she saw his shoulders tense or his breath quicken, they’d pause for a quick “reset” together, like hand squeezes or a slow hallway walk.
Within weeks, meltdowns softened into shorter moments he could recover from, and Luca began saying proudly, “Mom, I got my brain to quiet down”. These small, steady practices didn’t solve everything overnight, but they gave them both a clearer path back to calm.
Dr. Roseann’s Therapist Quick Tip
In my 30+ years of clinical practice, I’ve learned that dysregulated behavior isn’t a child being difficult—it’s a child whose nervous system has gone offline. You can’t teach skills to a brain that isn’t calm enough to receive them.
Try this today:
Use one co-regulation tool—like a calming phrase or slow hand squeezes—before giving any directions.
Why it works:
These cues tell the brain “you’re safe,” allowing the prefrontal cortex to come back online so your child can actually shift and cooperate.
Remember:
Regulation always comes before correction, and your calm helps your child build real emotional skills—not just stop the behavior.
Early intervention is key. The sooner we start building skills through therapies like DBT, CBT, or parent training, the better the outcomes. Emotional regulation is like a muscle; with consistent practice, it grows stronger. Life becomes less about crisis management and more about connection.
You don’t have to steer this alone. Hope and help are available. The path to balance starts with understanding and leads to a calmer life for the whole family.
Frequently Asked Questions
What is the difference between a tantrum and behavioral dysregulation?
A tantrum is typically goal-oriented—a child wants something or is protesting a demand. It usually stops when the goal is met or the child gives up. The storm passes relatively quickly.
Behavioral dysregulation is a true loss of emotional control—not a tactic to get a want. The nervous system is overwhelmed, the thinking brain goes offline, and reactions are disproportionate and can linger. It’s brain-based and needs compassion, not punishment.
Is behavioral dysregulation a formal mental health diagnosis?
No, behavioral dysregulation is not a standalone diagnosis in the DSM-5. Instead, it is considered a core symptom or feature of many other conditions. Think of it as a red flag indicating a deeper issue.
Dysregulation is a prominent feature of disorders like Borderline Personality Disorder (BPD), ADHD, and Disruptive Mood Dysregulation Disorder (DMDD). Identifying significant dysregulation helps clinicians understand what underlying condition may need treatment and support.
Can children outgrow behavioral dysregulation?
Severe dysregulation rarely disappears on its own. The real hope lies not in outgrowing it, but in learning to manage it.
With early, targeted support, children can build lifelong regulation skills. DBT, parent training, and treatment for conditions like ADHD create a practical toolkit. Sensitivity may persist, but emotion and behavior control can improve markedly, easing daily challenges.
We’ve seen countless families transform when they get the right support. At our center, we are committed to providing game-changing solutions that deliver results when other approaches haven’t worked.
Citations
- Lavi, I., Ozer, E., Katz, L., and Gross, J. (2021). The role of parental emotion reactivity and regulation in child maltreatment risk. Clinical Psychology Review., 90. https://doi.org/10.1016/j.cpr.2021.102099
- Dunn, E., Nishimi, K., Gomez, S., Powers, A., and Bradley, B. (2018). Developmental timing of trauma exposure and emotion dysregulation in adulthood: are there sensitive periods when trauma is most harmful. J Affect. Dis. 227:869-877. https://doi.org/10.1016/j.jad.2017.10.045
- Retz, W., Stieglitz, R-D., Corbisiero, S., Retz-Junginger, P., and Rosler, M. (2012). Emotional dysregulation in adult ADHD: what is the empirical evidence? Expert Review of Neurotherapeutics, 12(10):1241-1251. https://doi.org/10.1586/ern.12.109
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!











