
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!















Ben is a 15 yr-old-boy who experienced the sudden onset of medical and mental health issues after having the COVID virus.
He had a normal, uncomplicated birth and a normal childhood. He had a head injury from sports at age 11 but recovered without complication. He had no known medical, attentional, learning, behavioral, or emotional issues until he had COVID.
Within 10 weeks of having COVID, Ben had an onset of diabetes type 1. Signs of anxiety, including repeated questions, difficulty sleeping, and being less willing to try new things began to appear shortly thereafter. Ben’s parents assumed it was related to diabetes diagnosis.
Obsessive thinking and rituals were noticeable and it ramped up very quickly when Ben began to refuse to go to school. His compulsive questioning due to intrusive thoughts and food restricting got in the way of his daily functioning. His parents brought Ben to a psychiatrist who was diagnosed with Generalized Anxiety Disorder (GAD) and Obsessive Compulsive Disorder (OCD). He was prescribed an SSRI, which lessened to some degree Ben’s intrusive thoughts and anxiety but then he became quite depressed and withdrawn.
A series of medication trials were conducted with no symptom relief. Ben also went to three different therapists who used cognitive behavioral therapy and one tried mindfulness activities. His parents reported that while the therapy helped them manage Ben’s behaviors, no noticable changes occured and Ben actually worsened over this 18-month period. Furthermore, he developed depersonalization symptoms.
Ben and his family sought care in our program after a referral from their pediatrician and a referral from a friend and in an attempt to avoid in-patient hospitalization for OCD and depression.
Ben’s QEEG Brain Map showed diffuse low activity across all brain wave activity and in his brain communication. Ben’s brain was extremely understimulated. Having done more than 10,000 brain maps and with a large portion of these brain scans from people infectious disease, it was clear that Ben’s brain’s low activity resulted from a virus.
Ben’s sudden onset of Diabetes 1 and then anxiety and OCD were due to the infection induced autoimmune PANS. Ben went from a typical teen before COVID to one that was anxious, withdrawn, had suicidal thoughts, had intrusive thoughts and feelings of depersonalization that stopped him from connecting with others and going to school.
Phase one of his program focused on taking a deeper look at just what physical damage COVID had done to his brain and body, which started with getting him to a functional PANS-literate physician to run lab work. In our program, we focused on calming his brain first through a combination of neurofeedback, PEMF, dietary changes, dietary supplements, detoxification and gut support, and parent coaching to manage outbursts.
Ben and his parents needed a lot of support and education about how infectious disease affects the brain and behavior and how obsessions, compulsions and rituals easily become a habit. He began exposure and response therapy (ERP) to address Ben’s intrusive thoughts and rituals and his parents participated in the therapy in order to learn the right verbiage to manage the behaviors.
Ben did neurofeedback, PEMF/BRT and psychotherapy intensively for three weeks in order to get his depression and OCD behaviors into a safer and manageable level. We then tapered down sessions.
Phase two focused wellness and nutritional coaching to support his food restricting and sensory aversion behaviors. Once Ben learned how to “talk back to his OCD” and become more emotionally regulated, we worked with Ben and his family to bring stress lowering activities into their daily lives. Ben gradually could go for walks, spend more time with his family and tolerate typical stressors.
Phase two focused on reconnecting Ben to his body in order to reduce his depersonalization experiences. His OCD and anxiety had to be brought under control before this could be attempted.
QEEG Brain Map Comparison from QEEG #1 to #3 after 56 sessions of Neurofeedback,
20 sessions of PEMF/BRT therapy and ERP psychotherapy in our BrainBehaviorReset™ Program.
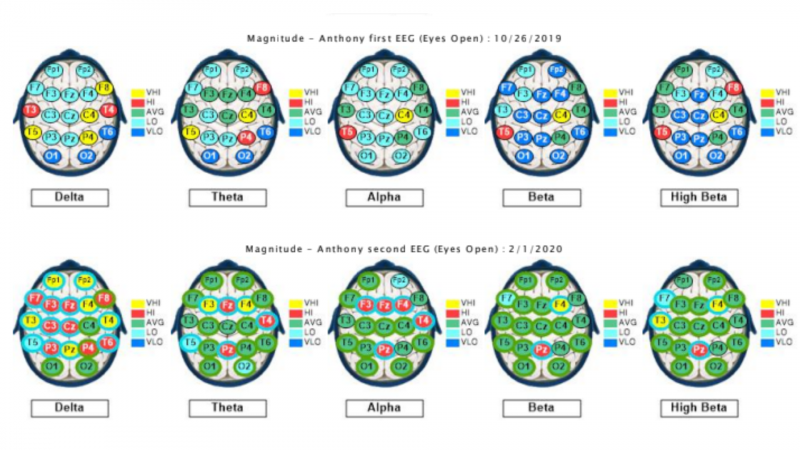
With 56 sessions of neurofeedback, 20 sessions of PEMF combined with biofeedback, ERP psychotherapy for OCD, Ben’s overall brain power went from being in an underactive state diffusely to almost complete normal brain wave functioning.
Ben was able to avoid in-patient hospitalization through a combination of intensive brain-based therapies and psychotherapy. His depression and obsessions and compulsions moved from a debilitating level to a more functional level, which was reflected in positive behavioral changes and a successful return to school.
His lab work showed several nutrient deficiencies and was positive for two childhood viruses that were addressed through his functional physician.
After normalizing his intrusive thoughts and reducing anxiety, Ben was able to overcome his restrictive eating and the addition of a nutrient dense diet furthered his treatment progress. He has become sociable again and Ben and his parents see him as happier at home.
Ben and his parents continue to see a psychotherapist, use supplements that address mood, stress, detoxification, and immune function and use PEMF/BRT to calm his brain.
These case studies are a description of the experiences of our clients. We have changed the names and some details to protect their privacy. Each client experience and protocol is unique in our trademarked BrainBehaviorReset™ Program.

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
