
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!













Iris is a 7 yr-old-girl with a history of anxiety and obsessive and compulsive behavior.
Iris was born via cesarean section after her mother was in labor for more than 24 hours and signs of fetal distress were noted. Her apgar was initially a five but improved to a nine with oxygen. She was placed in the neonatal intensive care for a few hours as a precaution and no other issues were noted.
Iris was described as a baby that needed holding and had difficulty sleeping on her own. She had separation anxiety all the way through preschool and needed time before and after drop off to calm down with adult support.
She was resistant to trying new things and only after her siblings did them first. Iris needed cajoling even then.
By age three, Iris began to repeat questions that she knew the answer to and needed reassurance from her parents and later teachers at school. She transitioned well to kindergarten because her cousin was in her class. Her teacher noted that she was shy in class but completed her work.
Her anxiety and compulsive questioning increased in the first grade, especially with increased writing demands. As the year progressed, Iris' perfectionistic tendencies interfered with her ability to turn her work in on time. The school implemented a building plan to put supports in place to reduce her workload but that backfired as Iris just spent more time on making her assignment, “just right.”
Her parents sought therapy at age 6, where at that time Iris was diagnosed with anxiety disorder. She began therapy with a therapist who specialized in kids with anxiety. Therapy focused on teaching Iris and her parents mindfulness based stress reduction techniques and naming her feelings. Iris' behavior worsened so her parents switched therapists and to more of a play-based therapy.
Iris' anxiety improved for a few months with play-based therapy but then she began to regress. Her therapist recommended psychiatric medication for anxiety and a consult with a psychiatrist. After a brief consult with psychiatrist, the physician wanted Iris to begin an SSRI for anxiety. Her parents researched the side effects and decided to look for other treatments and began to question if this was possibly OCD. Iris' aunt had OCD and although it didn't look exactly the same, they were seeing the same irrational compulsive behaviors and obsessive thinking.
Iris' parents found me after a Google search and read my book, “It's Gonna Be OK!” before they booked an intake appointment with a QEEG Brain Map. Not only was her QEEG Brain Map consistent with OCD patterning, so were the clearcut obsessive thinking and compulsive behaviors we compiled during the intake.
Iris had specific fear around her parents and grandmother dying, her work being “wrong,” and that kids didn't like her. She had developed rituals to deal with her fears, including having her parents, caregivers and teachers respond to her questions. They all were inadvertently fed into fears and made the intrusive thoughts worse. This is called a negative reinforcement cycle and the obsessive and compulsive behaviors were actually getting reinforced and worsening as a result.
Even her therapists who had misdiagnosed Iris as having generalized anxiety disorder and not OCD, didn't give Iris the tools she needed to cope with her intrusive thoughts, so her fears grew and became more of an ingrained learning pattern.
Iris' QEEG Brain Map showed high levels of Beta and overstimulated brain communication. This is one of the four common patterns associated with OCD.
Her care plan focused on calming her brain on fire down. We focused on calming her brain through a combination of neurofeedback, PEMF, dietary changes, dietary supplements, gut support, and parent coaching and ERP therapy for OCD.
QEEG Brain Map Comparison from QEEG #1 to #3 after 34 sessions of Neurofeedback,
daily PEMF/BRT therapy and ERP psychotherapy in our BrainBehaviorReset™ Program.
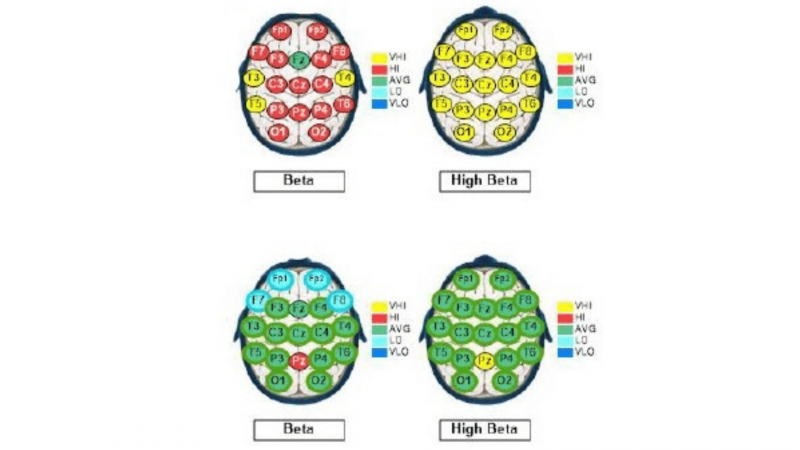
With 34 sessions of neurofeedback, Daily PEMF through a mobile unit, ERP psychotherapy for OCD, Iris' overactive brainwave activity significantly reduced by more than 55%.
In terms of ERP psychotherapy, Iris was resistant at first to even small exposures that challenged her obsessive fears but as her brain quickly calmed down with PEMF, neurofeedback and supplements, she became more responsive to the ERP process. Over time, Iris even began to enjoy the process and was proud of what she was able to do.
After normalizing her intrusive thoughts and reducing anxiety, Iris was noticeably more talkative and social. Her need for reassurance was significantly reduced and Iris was open to parent coaching that supported her stress tolerance and coping skills that she learned in ERP.
Iris and her parents continue to see an ERP therapist on an add needed basis, use supplements that address stress and gut function and use PEMF/BRT to calm her brain.
These case studies are a description of the experiences of our clients. We have changed the names and some details to protect their privacy. Each client experience and protocol is unique in our trademarked BrainBehaviorReset™ Program.

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
