
Counter your overwhelm and reset your nervous system in 7 days
7 Days to
Self Regulation
Challenge starts on April 22!
ADHD is a commonly misunderstood or misdiagnosed mental health condition. People often think that children or teens with attention difficulties always have the brain-based disorder ADHD. But there are many things that can interfere with our focus and attention.
Other mental health conditions, such as anxiety and obsessive-compulsive thinking and even bad sleeping habits, can make it difficult for children and teens to focus or pay attention. So, just because your child can’t focus, doesn’t mean that they have ADHD. It’s important to look at the actual cause of the problem to find the right solutions to make your child or teen successful in school, at home, and in social situations.
TABLE OF CONTENTS
ADHD isn’t simply the inability to stay focused. Attention-Deficit Hyperactivity Disorder (ADHD) is a mental health condition affecting millions of teens and children all over the world. This chronic condition can persist into adulthood, which is why early diagnosis is important.
A child with ADHD tends to show different symptoms, particularly hyperactivity, impulsivity, and difficulty sustaining focus and attention. They also exhibit below-average executive functioning skills, and challenges to their everyday performance. Estimates show that 1 out of every 10 children is diagnosed with ADHD, making it rank as the second most common mental health issue among children.
A lot of people think that a child with ADHD can’t focus, but that’s not entirely correct. These children can focus and even hyperfocus if they’re doing a task that interests them. Some parents assume that since their kid can focus, he can’t have ADHD. What they don’t realize is that their child is in hyperfocus mode, which means their brain is getting stimulated by doing the task, holding their interest and excitement.
What are the Types of ADHD?
There are three subtypes of ADHD and a child may be classified under one of them based on their symptoms. Such symptoms should be present before they reach 12 years old and should occur for over six months.
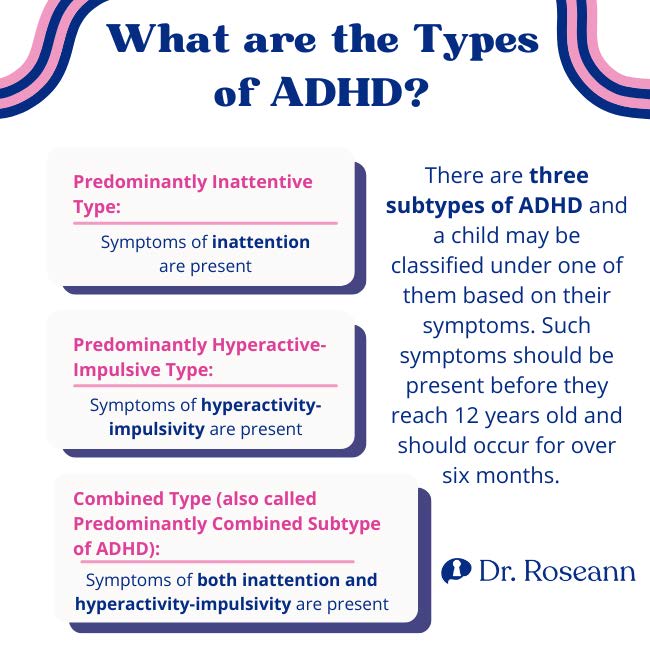
Predominantly Inattentive
The predominantly inattentive presentation is generally not as disruptive as the other ADHD type. An ADHD child classified until this type exhibits problems with inattention and sustained attention.
As a result, these kids have the tendency to zone out or daydream. They can follow instructions and abide by the rules but will need adequate support and constant reminders to start and finish their tasks. Without guidance, they’ll likely make mistakes.
These kids may possess high-level verbal and cognitive skills despite the inattention issues, making the condition even harder to diagnose. When these kids enter middle school, they’ll have to do more intensive schoolwork. That’s when their condition becomes apparent because they tend to have more pronounced social and organizational issues than other children.
Predominantly Hyperactive-Impulsive
Children diagnosed as hyperactive-impulsive are easy to recognize, mainly because their behavior can be disruptive. These kids are generally described by their primary school teachers as poor listeners and handsy. They also have trouble transitioning or staying in their seats.
Because of their impulsiveness, these kids may experience social issues. Their unruly behavior may wear out friendships. Neurotypical children struggle in managing the dysregulation of other children with ADHD.
Since the hyperactive and impulsive behaviors of these kids are very apparent, they tend to get diagnosed early. However, some teachers may still confuse an ADHD child's hyperactivity and impulsivity with normal high-energy behaviors, especially for boys.
Combined Type
Children diagnosed with the combined presentation exhibit symptoms classified under the two other types. It means they are hyperactive-impulsive and inattentive. Their symptoms are evenly balanced, meaning they show at least six symptoms from the inattentive type and six from the hyperactive-impulsive type.
Because all of the symptoms of ADHD are present in these kids, their behaviors are different from what you might expect in a child of their developmental age. These children require more care because aside from ADHD, they may have other issues, particularly low self-esteem, and frequent mood swings.
What are the Statistics on ADHD in Children?
Research shows that 1 in 10 children ages 2-17 have been diagnosed with ADHD. According to a CDC study in 2020, about 6.1 million children in the United States (9.4 percent) between ages 2 to 17 are estimated to have ever been diagnosed with attention deficit hyperactivity disorder (CDC, 2020).
Additionally, 64% of children with ADHD also had another mental, emotional, or behavioral disorder. Boys are also more likely to have ever been diagnosed with ADHD than girls (12.9 percent and 5.6 percent (Danielson et al., 2018).

What are the Symptoms of ADHD?
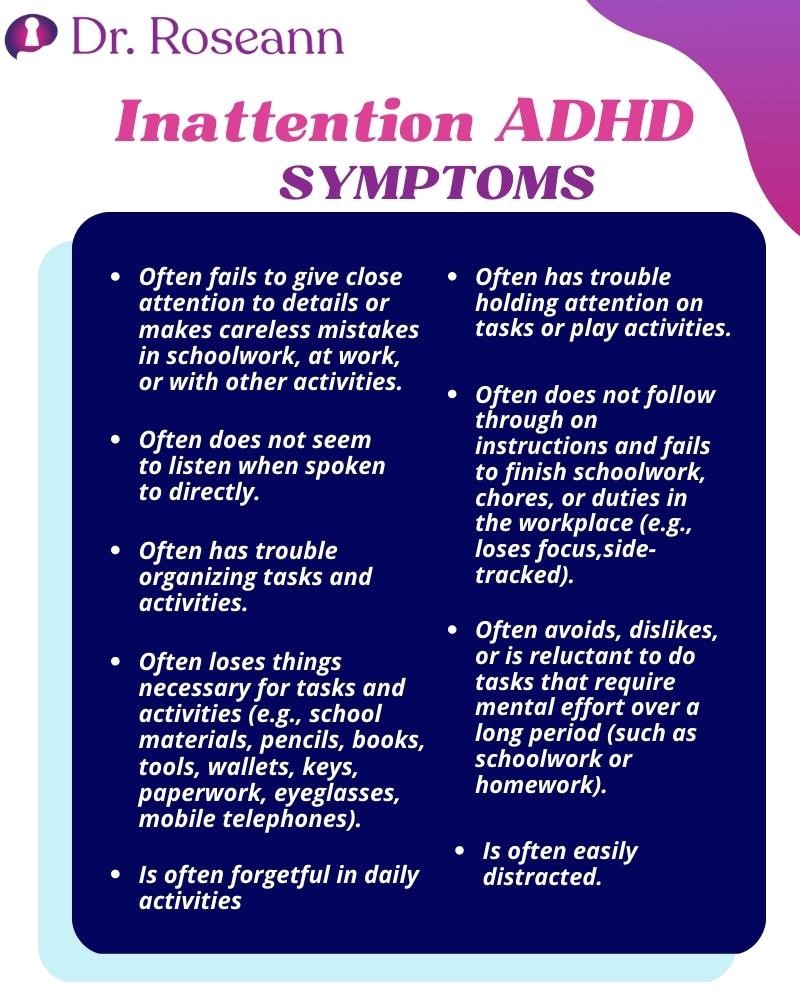
When determining ADHD in children, physicians or psychologists have to determine if the DSM criteria are met. ADHD symptoms should be present in the child before age 12 and should present in a persistent pattern.
The child’s hyperactivity/impulsivity or inattention issues should interfere with their development and functioning in multiple settings. There should be clear evidence that the child’s symptoms reduce the quality of or interfere with their social or school functioning. Symptoms must be present in more than one setting.
The DSM criteria specify that their symptoms can’t be explained by any other mental health disorder, such as anxiety disorder, personality disorder, mood disorder, or dissociative disorder. The symptoms must also not occur only during a psychotic disorder like schizophrenia. These are the DSM-5 criteria for ADHD:
To determine if the child (16 and under) is of the inattentive ADHD type, at least six of the symptoms below have occurred. For teens 17 years old and above, including adults, five or more symptoms should appear. These symptoms should persist for at least 6 months, and they are inappropriate for developmental level:

Six or more symptoms of hyperactivity-impulsivity occurring for children up to age 16, or five or more for adolescents 17 and older or adults; symptoms of hyperactivity-impulsivity have been present for at least 6 months, to the extent that is disruptive and inappropriate for the person’s developmental level:
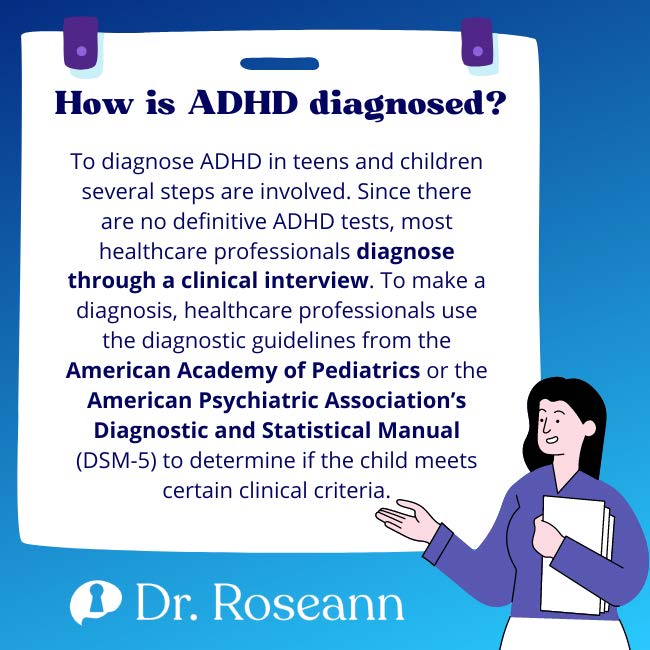
How is ADHD diagnosed?
To diagnose ADHD in teens and children several steps are involved. Since there are no definitive ADHD tests, most healthcare professionals diagnose through a clinical interview. To make a diagnosis, healthcare professionals use the diagnostic guidelines from the American Academy of Pediatrics or the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-5) to determine if the child meets certain clinical criteria.
Schedule a consultation with a mental health professional to determine if your child has ADHD. To arrive at a clinical diagnosis, information is gathered from several sources, such as teachers, caregivers, and parents. Pediatricians can diagnose if a child has ADHD after caring for them or using behavioral rating scales.
As pediatricians are considered generalists, there’s a need for more specific ADHD guidance. For this purpose, a psychologist, psychiatrist, or neurologist can help. Psychologists can give an ADHD diagnosis and work with your child through parent coaching and psychotherapy.
The clinical intake is a meeting with a mental health or medical professional to gather information to determine if a child has ADHD. The professionals will attempt to have a better picture of who the child is and what his needs and strengths are.
After the interview process and through observation, issues are identified. The healthcare provider will then determine if those issues are clinical issues or developmental lags. Expect these meetings to be long, as they can last for an hour or even more. Healthcare professionals will collect the following information:
Testing is the next step after diagnosis. Healthcare providers use questionnaires or rating scales to test how specific attention issues and behaviors impact the child at home and in school. The provider will compare the child’s behavior with kids of the same age.
To document their behaviors, standardized rating scales will be used. Direct measures of attention and executive functioning may be applied as well. Rating scales aren’t perfect tools but they can offer essential information about the child’s behavior to identify their diagnostic criteria and guide their therapy.
When a child presents with executive functioning, processing, and attentional issues that get in the way of their academic performance, a neuropsychological or psychoeducational evaluation is required. These are more comprehensive evaluations that consist of several hours of individually administered standardized tests in behavioral, academic, and cognitive areas.
Not all children with ADHD need this comprehensive evaluation. But for those who are struggling academically, the evaluation will be useful in identifying key areas where they need more support at school via a 504 Accommodation Plan or Individual Education Plan (IEP).
QEEG brain mapping is more effective in assessing a child’s ADHD issues compared to using rating scales or doing a clinical interview. This process is short and simple, as it only requires a 15-minute meeting.
The symptoms of ADHD in kids may look similar to children diagnosed with depression, anxiety, PTSD, OCD, sensory processing, autism, birth trauma, genetic issues, nutritional deficiencies, and learning difficulties. This is because they are all likely to struggle with controlling impulses and focusing.
Some children and teens don’t even have clinical issues and are merely reacting to the wrong peer or classroom environment or developmentally inappropriate school work. All these considerations must be ruled out prior to giving an ADHD diagnosis to identify the right form of treatment.
Healthcare providers should understand all the factors that may cause the child’s behavior before diagnosing ADHD. Some children may show ADHD symptoms in comorbidity to other conditions.
These conditions include bipolar disorder, depression, anxiety/PTSD/OCD, sensory integration dysfunction, autism, dyslexia or other learning disabilities, CAPD, metabolic issues or nutrient deficits, Lyme/tick-borne illnesses, and other chronic medical conditions.
All these conditions have to be ruled out before giving an ADHD diagnosis. While an ADHD child may also have other clinical issues, knowing whether ADHD is their primary or secondary condition is a great way to effectively provide treatment. For example, if the child’s main concern is not ADHD but anxiety, providing treatment for ADHD may exacerbate the problem.
ADHD in Girls
Girls are at risk for ADHD as much as boys. However, research shows that girls are more likely to have inattentive ADHD than the hyperactive/impulsive or combined type. This also means that girls often go undiagnosed compared to boys because they don’t exhibit disruptive behavioral problems.
Girls with ADHD can cope with their studies early on, however, when they get to middle school where school work becomes more intensive, they struggle with meeting expectations because of their poor executive function skills. As healthcare professionals learn more about ADHD, a lot more girls get diagnosed with the disorder.
What are the Causes of ADHD?
The functions of the nervous system get affected by ADHD, which means medical tools can help arrive at a definitive diagnosis. One researcher discovered that people with ADHD have “cortical slowing” characterized by a reduction of higher-frequency beta waves and elevation of low-frequency theta waves in the prefrontal cortex.
While the medical community is still studying the exact causes of ADHD, they are looking at the involvement of environmental and genetic factors. Furthermore, they see functional and structural differences in the brains of children with ADHD.
Structurally, a child with ADHD shows cortical thinning, delayed cortical development, and reduced gray and white matter volume. Functionally, the differences include reduced connectivity of neurons in the cerebellum, prefrontal cortex, and basal ganglia. The frontal brain waves of children with ADHD don’t have enough fast-wave activity but too much slow-wave activity for them to stay engaged.
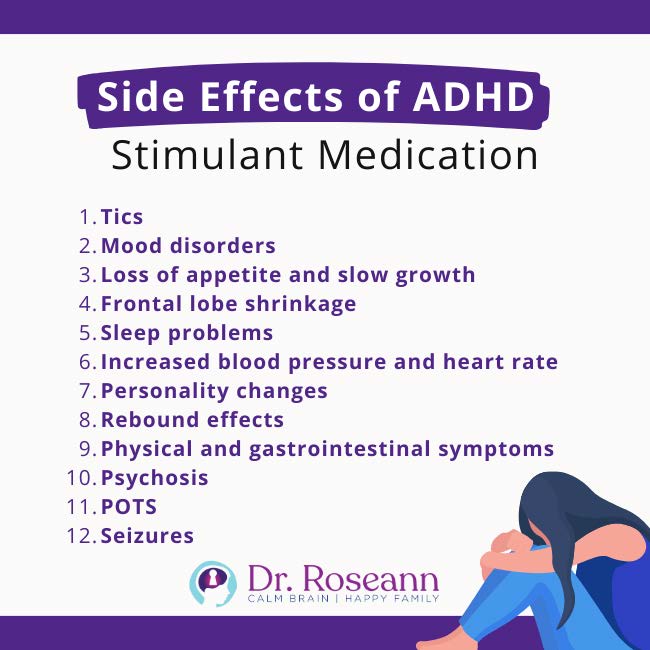
Side Effects of ADHD Stimulant Medication
While a lot of parents are willing to tolerate the short-term side effects of ADHD medications, many are not aware of their long-term side effects. Here are some of them:
Many children and teens taking stimulants to suppress ADHD symptoms develop tics. Tics are habitual muscle spasms evident in the face and body. Tics can be motor or vocal in nature, and they’re easily observable.
Having tics can further create feelings of inadequacy for children and teens. Tics may become a social obstacle because others don’t know what to make of them, encouraging awkwardness in a social setup.
Another long-term effect seen in children and teens taking ADHD medicines is the development of depression, disruptive mood disorder, and bipolar disorder. When stimulant medications like Adderall were given to teens and children in a very high dose, or if the drug failed to work for them, depressive symptoms are observed.
Loss of appetite is among the most common side effects of ADHD medication. Children and teens tend to receive insufficient calories for their bodies due to these medicines. The failure to eat enough during their transformative years will have a long-term effect on their health.
Some studies found correlations between stunted growth and ADHD medications in different individuals. It is due to the fact that ADHD causes appetite suppression and decreased calorie intake. These factors result in slower growth.
Children and teens taking ADHD medications have reduced brain volume, with the left hippocampus most affected. The frontal lobe controls executive functioning and attention. Executive functions are the brain’s job manager, which helps children get things done independently.
ADHD medications will also affect one’s sleeping patterns. It is because these medicines have brain-stimulating effects. As a result, kids and teens may complain about trouble falling asleep or staying asleep.
ADHD medications may increase blood pressure and heart rate. Physical tensions, anxiety, and a heightened emotional state are commonly observed. Children and teens may describe it as if their hearts and minds are racing too fast.
ADHD medications tend to decrease creativity and flatten personalities. Children and teens with ADHD are generally creative, divergent thinkers. These medications diminish that. Some teens and kids taking these medications may lose their unique awesomeness.
Once the medications wear off, ADHD kids and teens may experience a temporary worsening of their symptoms. This is also known as the rebound effect. It means increased hyperactivity, emotional lability, unfocused behaviors, and even aggression after being medically constrained.
It’s not uncommon for children and teens to suffer from gastrointestinal symptoms like nausea, bloating, abdominal pain, and gas after taking ADHD medications. The other physical symptoms they experience are dizziness, headache, chest pain, fever, Joint pain, skin rashes, hives, and tremor, among others.
When in psychosis a person may break away from reality in single or multiple episodes. During such a state, their thought patterns, verbal communication, and behaviors may be unpredictable and irrational. In extreme cases, they can cause harm to themselves and others.
Postural tachycardia syndrome or POTS is a type of condition affecting blood flow. ADHD medications may cause increased heart rate with movement, such as from sitting down to standing up. It may result in fainting, which is dangerous, as it may lead to head injury or death due to a fall.
There’s some evidence that methylphenidate in ADHD medications may initiate seizures. Overdosing on methylphenidate leads to seizures and many other side effects. Intentional overuse or improper dosing is harmful to kids and teens.
While many parents think medication is a valuable tool in treating ADHD symptoms, it isn’t the only option. Parents who don’t want to use chemicals to address ADHD may consider natural solutions. Using pharmaceutical medications may have parents concerned about their plethora of possible adverse side effects. Some parents think that having their children rely on high-priced pharmaceuticals for wellness isn't a viable long-term solution.
On top of what you may have heard or been offered by your child’s healthcare provider or school counselor, there are several science-backed ways to help reduce and even reverse ADHD symptoms in children. These are
Instead of taking mind-altering medication, neurofeedback is a tool that is very effective at retraining brain waves. The brain produces certain types of waves based on whether the mind is in an active, focused state or not.
Neurofeedback teaches the brain to efficiently shift into a concentration state by learning how to produce brain waves associated with focus. With neurofeedback, the brain learns to act in a healthy, more flexible way. It increases focus and motivation while reducing distractibility and impulse control.
Over time, neurofeedback training teaches the brain how to self-regulate. It will soon get trained to produce a healthy combination of brainwaves, which results in long-term changes that make children and teens feel calmer, more attentive, and in better control of their whole selves.

PEMF or Pulsed Electro-Magnetic Field therapy helps calm the brain so kids and teens can think clearly, pay attention, and take action. This tool is a great treatment for attention, executive function issues, and anxiety because it improves cellular communication, calms the body to free it up for other action, and stabilizes more functional brainwave activity.
PEMF helps ease the nervous system into the parasympathetic state, where brainwaves are more regulated. Also at that state, the number of excitatory neurotransmitters decreases, while healthy brain chemicals like endorphins, GABA, and serotonin increase. These healthy chemicals can ease mental health conditions such as ADHD, anxiety, and mood disorders.
If your child struggles with attention, impulse control, and focus it’s often caused by issues with nervous system regulation and nutrient deficiencies. Nutrient supplementation can go a long way in improving the functions of the brain so that your child can think clearer, listen to instructions, and get things done. These supplements effectively keep the nervous system healthy and help the brain regain focus.
Other Natural Remedies For ADHD
Low Magnesium Levels and ADHD
Low levels of magnesium is associated with a number of physical and mental health issues, making it an important nutrient. Prioritizing getting magnesium through food or direct supplementation is needed for all kids, but especially with ADHD.
There are a number of studies that highlight how low magnesium levels affect behavior. WA deficiency in magnesium is associated with callous or unemotional traits in children (Portnoy, 2021). Along with B6, magnesium is involved in neurochemical processes implicated in modulating antisocial behavior and callous or unemotional traits.
In the Journal of Medical Human Genetics, a 2016 found that (72%) of ADHD children in the study had a magnesium deficiency.
Inattentiveness, feeding problems, and low dietary intake due to psychostimulant medication side effects are just some of the reasons why children with ADHD have low magnesium levels.
On the flip side, studies show having good levels of magnesium is related with lower levels of anxiety, depression, and ADHD symptoms.
Executive functioning is a central process involved in providing order and organization to our behavior and actions. It acts as the brain’s control center allowing us to perform complex cognitive functions.
Think of it as the brain’s task manager, which is involved in all cognitive processes. Executive functioning includes strategic thinking and planning for the future. It also controls the body’s ability to delay or inhibit responding.
Executive function also handles self-regulation, initiating behavior, and shifting flexibly between activities. If your child is having issues with executive functioning, all tasks that require planning, organization, flexible thinking, memory, and time management become a challenge.
Psychologists and psychiatrists can help support children and teens through direct skill set education and therapeutic executive function coaching. They may also use the latest neuroscience research to show how to get your child’s brain to alert differently for better executive functioning.

What Should Parents Do to Help an ADHD Child or Teen?
It can be frustrating at times to parent an ADHD child. These kids tend to have problems starting and completing tasks that don’t interest them, and have what seems to be limitless energy. Here’s what you can do to support them:
The best way to support a teen or child with ADHD is to know how it affects the brain. It’s not easy to understand the brain workings of ADHD children and what they struggle with. But if you clearly understand your child’s abilities, it’s easier to harness their strengths and better support them for the future.


Parents should understand that they’re not alone and that there are healthcare professionals that can support them too. Find a trusted mental health provider who specializes in ADHD and can give you solutions and tools that can provide positive, lasting effects on your child.
It’s important to choose solutions that are effective and safe for your kids. There are alternatives to mind-altering ADHD medications such as psychotherapy, PEMF, neurofeedback, magnesium supplements, and nutrition. These solutions are backed by science to work on children and teens.


It’s not easy to support kids with special needs and as parents, we get exhausted too. It’s important to be around people who can help you take care of your child and ease the stress of doing it alone. Parents need to take a break once in a while to manage their own stress levels and put themselves in the best position to parent effectively.
Centers for Disease Control and Prevention. (2020, June 15). Data and Statistics on Children's Mental Health. https://www.cdc.gov/childrensmentalhealth/data.html
Danielson, M. L., Bitsko, R. H., Ghandour, R. M., Holbrook, J. R., Kogan, M. D., & Blumberg, S. J. (2018). Prevalence of Parent-Reported ADHD Diagnosis and Associated Treatment Among U.S. Children and Adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. https://doi.org/10.1080/15374416.2017.1417860
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Always remember… “Calm Brain, Happy Family™”
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”
She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2022

The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.

Counter your overwhelm and reset your nervous system in 7 days
Challenge starts on April 22!
147 Therapist-Endorsed
Self-Regulation Strategies
for Children
A Practical Guide For Parents
