Tics are irregular, non-voluntary, repetitive muscle movements in different body parts.
Movements such as eye-rolling, head jerking, and shoulder shrugging are called motor tics. Involuntary repetitive sounds, including grunting, sniffing, or throat clearing, are known as vocal tics.
Tics are typically classified as either motor or vocal tics. There are common examples of tics:
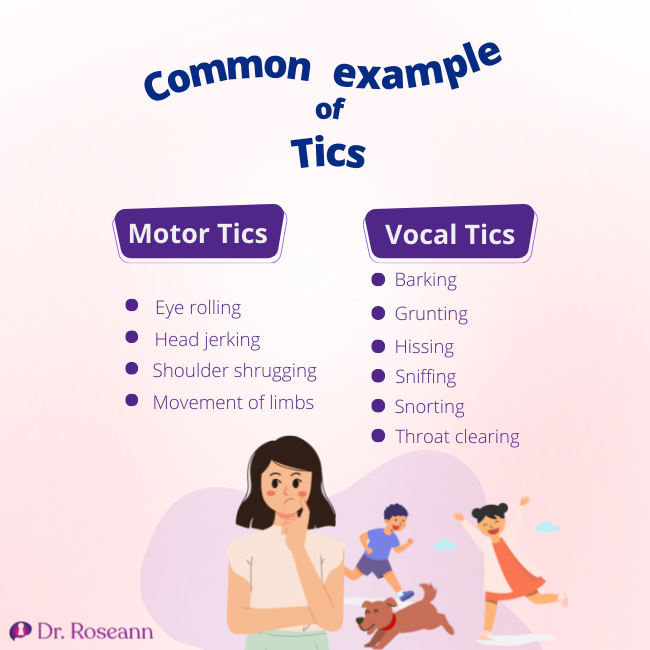
Motor Tics
- Eye rolling
- Head jerking
- Shoulder shrugging
- Movement of limbs
Vocal Tics
- Barking
- Grunting
- Hissing
- Sniffing
- Snorting
- Throat clearing
Causes of Tics
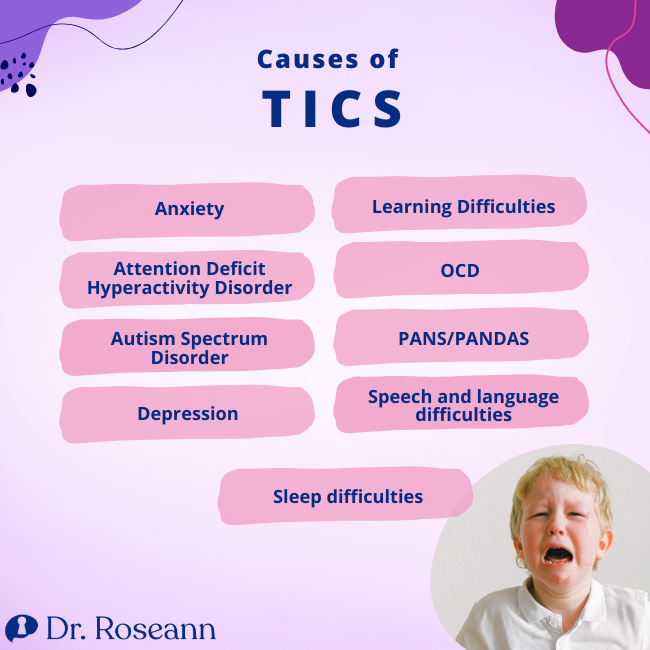
One cause of tics is Tourette's Syndrome. Tics are often seen in children with PANS and PANDAS, which is an infectious disease and toxin triggered disorder that produces sudden and intense psychiatric or cognitive symptoms. Tics are also associated with:
- Anxiety
- Attention Deficit Hyperactivity Disorder
- Autism spectrum disorder
- Depression
- Learning difficulties
- OCD
- PANS/PANDAS
- Speech and language difficulties
- Sleep difficulties
Leah's Story: Tics in PANS/PANDAS
For 5-year-old Leah, PANDAS first manifested in irrational fears.
The family had just arrived in Illinois from a month-long vacation in Arizona when Leah started fearing that someone was going to vomit. And then, she feared that she would vomit, which is called Emetophobia
Leah's fear of vomiting and germs extended to cars and everything else around her — until it quickly took over her life. She was unwilling to ride vehicles and do gymnastics, which is her life's passion.
The condition lasted for months. Her parents coped through going to therapists that focused on anxiety and self-help psychology books, which worked for a while. So, they assumed all was well again. And for a time, it was.
Two years later, Leah had a viral infection. Her fear of vomiting and riding in the car relapsed and things drastically changed. She was overwhelmed with intrusive thoughts about her parents getting into a terrible accident and insisted on being with them at night. Her parents assumed that she was being defiant and would carry her back to her room, but she would not stay.
Afterwards, Leah experienced her first panic attack. She fell on the floor and was kicking and screaming and flailing around.
She also started having tics, which was noticeable in school. Her friends thought she was being rude when she would roll her eyes and jerk her head. Some of her classmates made fun of her.
Leah and her parents went to several doctors and psychologists for the next two years but nothing moved the dial.
Leah experienced more rages, and would last an hour before she went back to normal. Then, she had stopped doing the things she loved, including gymnastics, because of separation anxiety. She felt better and relieved with her parents around.
Finally, they came across a therapist, who had helped kids diagnosed with PANDAS, and thought Leah showed the symptoms.
Leah was tested with a variety of blood tests, including the Cunningham Panel — one of the blood tests that helps doctors identify autoimmune-induced encephalopathy triggered by infections, such as PANS and PANDAS. She also had a clinical intake that looked at her extensive history of symptoms and on and off strep infections.
Leah began treatment for PANDAS. The family immediately started Leah on antibiotics and supplements to help calm her brain and address nutrient deficiencies. With this regime they began to see her symptoms ease.
They also wanted to dig deeper into her bodies' ability to detoxify, since she had on and off strep infections for so long. She had to get over ten vials of blood drawn during this process. The blood tests revealed that Leah has a gene mutation that causes her body not to detox properly.
Her doctor added supplements to support the detoxification and had Leah also use a sauna and PEMF to further aid detoxification.
Today, Leah is better at 11 years old. She is a delightful kid who gladly shares her PANDAS experience whenever it could help people.
While most of her symptoms have gone, the experience has been traumatic for the whole family. She and her family continue to try to lead a healthy lifestyle and moderate stress.
Because of her experiences, Leah has learned to be accepting and considerate of other people because you just don't know what people experience on the inside. She also hopes that more doctors would know about PANDAS.
Based on medical studies, PANS/PANDAS symptoms can eventually disappear with the right treatments and lifestyle changes. However, flares may occur with renewed exposure to other infections and stress.
What is PANS/PANDAS?
PANS/PANDAS are different clinical conditions that result from a misdirected immune response that manifests in sudden onset of OCD, tics, and limited food intake, along with other neuropsychiatric symptoms.
These disorders are lesser-known and often misunderstood. Your child's doctor may not be always familiar with them and often mistake it for other conditions.
If you suspect PANS/PANDAS, it is best to meet with a specialist for diagnosis and treatment otherwise your child and family may not get the critical care they need.
A clinical diagnosis is determined through a clinical intake that looks at medical history, signs, and symptoms. Giving a complete account of your medical history and describing your symptoms in detail is important.
Additional testing for infectious diseases, toxins, etc. can identify pieces of the puzzle that need to be addressed. . There's also a need to rule out other known neurological or medical disorders. It is important to note that there is no one test or set of tests that can give a definitive diagnosis and that a diagnosis can be made with a clinical intake.
Diagnostic Criteria for PANS and PANDAS Syndrome
PANS
The two disorders are different but both have a sudden onset of symptoms.
Pediatric Acute-onset Neuropsychiatric Syndrome
Is noted by an abrupt, acute onset of obsessive-compulsive disorder (OCD) or severely limited food intake
Alongside the presence of at least two of the following behavioral or neurological symptoms of PANS
- Anxiety, Separation Anxiety
- Behavioral Regression, Developmental Regression
- Depression, Emotional Lability
- Motor or Sensory Abnormalities
- Severe Oppositional Behaviors, Aggression, Irritability
- Somatic Symptoms, such as Sleep Disturbances, Enuresis, or Urinary Frequency
- Sudden Deterioration in School Performance
- Symptoms are not explained better by an established neurologic or medical disorder.
- It can occur with any age. Children aged 5-15 are especially vulnerable.
PANDAS
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections
- Presence of OCD and multiple, complex tics
- Age Requirement: onset usually occurs between 3 years of age and puberty
- Acute onset and episodic course (the child can get better for long periods, but the tics return when the child gets strep infection again)
- Association with Neurological Abnormalities
When is Tics a Sign of PANS/PANDAS?
70% of PANDAS cases experience tics, so it is a common occurrence
Comorbid neuropsychiatric symptoms are almost always present in PANDAS. These symptoms are similar to those seen in PANS, another condition that is typified by an abrupt onset or worsening of symptoms.
In addition to the sudden onset, somatic symptoms such as frequent urination, mydriasis, and difficulty sleeping, differentiate PANDAS from Tourette syndrome, other milder tic disorders, or non-PANDAS OCD.
Tic Disorders
Tic disorders are usually noticed in childhood, with onset typically around five years old. The symptoms are more common in boys. Most cases are temporary and resolved within a year. When tics continue longer, most tics resolve around by late teens.
However, one in a hundred individuals with tics develop a chronic disorder.
Tics can be mild to severe and suppressing tics can cause them to build with a release of tics all at once. Stress seems to worsen tics, so moderating stress through lifestyle changes and stress management techniques is critical.
Tourette's Syndrome
Tourette's syndrome (TS) is a neurological disorder that manifests in uncontrollable vocal and motor tics. Although it's the least common type of tic disorder, it can severely affect those suffering from it.
Uncontrolled muscle movements are the most common symptoms. They may occur in the face, hands, neck, shoulders, or torso. Examples include:
- Blinking
- Grimacing
- Head jerking
- Nose-twitching
- Squinting
- Shrugging
- Repeated foot tapping, leg jerking, or scratching
Complex tics
- Kissing
- lip-smacking
- Making rude gestures
- Pinching
- Sticking out the tongue
- Touching behaviors
Tic Disorder includes vocal tics
- Barking
- Echoing sounds or phrases repeatedly
- Grunting
- Gurgling
- Hissing
- Hooting
- Moaning sounds
- Saying rude things
- Sniffing
- Throat clearing, snorting, or coughing
- Tongue clicking
- Spitting
- Squeaking noises
- Whistling
Tic behaviors and symptoms of TS vary in severity over time and in how often they occur. Symptoms improve with age for most patients.
Currently, 0.3 percent of children aged 6 to 17 in the United States have been diagnosed with TS. Although the Centers for Disease Control and Prevention (CDC) reports that the exact number of people with TS is difficult to determine. As much as 50% of the cases are not diagnosed.
TS often manifests alongside other conditions, such as ADHD, autism, and OCD.
The Overlap of PANS/PANDAS and Tourette Syndrome
People with PANS/PANDAS have a different experience from people with OCD or tic disorders. The emerging and concurrent symptoms and the usual severity of OCD set the disorders apart. It is important to note that PANS/PANDAS has a sudden onset and should always be ruled out when tics appear “overnight” or when pre-existing tics worsen dramatically.
Treatment strategies for PANS/PANDAS and Tourette Syndrome are different. Thus, it is essential to get the correct diagnosis.
Unfortunately, PANS/PANDAS being a misunderstood disorder, there is a lack of universal knowledge about the similarities and differences of these disorders.
It can be difficult to set apart PANS/PANDAS from Tourette Syndrome or other tic disorders, and misdiagnosis or underdiagnosis is common.
Some people can be skeptical before they hear from those who have experienced it. They may conclude that the symptoms are only a result of Tourette's or tic disorder.
The PANS/PANDAS community has seen two different scenarios involving tic disorder
First, it is common for someone who meets the diagnostic criteria for PANS/PANDAS to be solely diagnosed with Tourette Syndrome or tic disorder, hindering appropriate treatment.
An even graver scenario, someone previously diagnosed with PANS/PANDAS can meet a new doctor who refutes the earlier diagnosis, sending the family yet down another rabbit hole
Tourette Syndrome and PANS/PANDAS
PANS/PANDAS Syndrome and Tourette Syndrome do share similarities and can sometimes be confused. But they can be set apart by numerous differences.
The items below outline their similarities or differences, although they may not apply to everyone. PANS/PANDAS and Tourette Syndrome are diverse conditions that can impact people differently.
Similarities
Motor and vocal tics can manifest in both Tourette Syndrome and PANS/PANDAS. To be diagnosed with Tourette's, the patient must be experiencing both vocal and motor tics for a year, alongside other criteria.
- Approximately 7 out of 10 people with PANS/PANDAS experience tics.
- Tics and OCD are the dominant PANDAS symptoms, but symptoms detailed in the PANS diagnostic criteria usually occur together. Technically, a PANDAS diagnosis only requires either tics or OCD.
- For a PANS diagnosis, an individual has to report restricted food intake or OCD, and two other comorbid symptoms. However, tics are not a must.
- OCD is a main PANS/PANDAS symptom that can occur with Tourette's Syndrome.
- People with Tourette's Syndrome may experience ADHD symptoms from childhood. Meanwhile, individuals with PANS/PANDAS may experience hyperactivity and lack of focus too but may not have an early history of it
- PANS/PANDAS symptoms can vary from flare to flare. There may not always be hyperactivity or lack of focus. Or symptoms might not start during the same exacerbation as the tics.
- In PANS, one can have obsessive thoughts, tics, and urinary frequency as their main symptoms in one flare but have intrusive thoughts, compulsive behavior, tics, and hyperactivity symptoms in a secondary flare.
- Rage can be present in people with PANS/PANDAS and Tourette's Syndrome.
- All three disorders notably begin in childhood. However, the onset of PANS can happen in adulthood. Despite the Tourette's Syndrome diagnostic criteria declaring that symptoms must begin before 18, there have been records of mild adult-onset. Complex tics can manifests in Tourette Syndrome and PANS/PANDAS
- PANS/PANDAS, OCD, and Tourette's Syndrome impact the Basal Ganglia functioning in the brain, explaining the similarities.
Differences
The cause of Tourette's Syndrome remains unknown although it can run in families. PANDAS, a form of basal ganglia encephalitis, is triggered by strep throat infections. PANS has many etiologies and disease mechanisms.
In some cases, patients with PANS/PANDAS can experience:
- coordination changes
- deterioration in handwriting and math skills
- behavioral and developmental regression
- difficulty swallowing
- dilated pupils, enuresis, frequent urination
- intense brain fog
- low muscle tone
- limited food intake
- memory decline
- personality changes
- psychosis.
These do not typically occur in individuals with Tourette's Syndrome.
No matter the diagnosis, the severe onset of motor or vocal tics can be disruptive and worrying.
PANS/PANDAS symptoms change a patient's personality overnight. Individuals with PANS who experience aggression, brain fog, behavioral regression, defiance, irritability, personality changes, and memory problems describe the experience as “losing themselves.”
Some people with PANS/PANDAS may manifest symptoms such as hyperactivity, tics, and OCD symptoms, so their symptomatic profile will be closer to Tourette's Syndrome. This means that noting the timing of the onset of symptoms and possible triggers such as strep or other infections is important.
The severity of Tourette's Syndrome symptoms can fluctuate. PANS/PANDAS symptoms can disappear for long periods and relapse upon exposure to a new trigger.
It's possible for PANS/PANDAS patients to experience residual symptoms between flares/exacerbations. However, the neuropsychiatric symptoms abruptly return when exposed to a trigger.
The onset of PANS/PANDAS is usually caused by an infection, though PANS may have non-infectious triggers. An infection causes the emergence of Tourette's Syndrome. However, Tourette's syndrome can see a slight worsening in symptoms when ill or stressed.
Antibiotics may relieve infection-triggered PANS symptoms, but not Tourette's Syndrome symptoms.
In Tourette's Syndrome, comorbid conditions may develop independently of the onset of tics. During childhood, someone with Tourette's Syndrome may be hyperactive but then later develop OCD, then in teens, undergo depression.
Whereas, in PANS/PANDAS, tics have a concurrent emergence as the other symptoms. Because someone with PANS/PANDAS can exhibit new comorbid symptoms with each new flare, the difference can initially seem astonishing.
But, again, the new symptoms in PANS/PANDAS are occurring with the onset tics and other symptoms.
For example, a preschooler with PANS/PANDAS may suddenly experience rage, fears, obsessions, separation anxiety, tics, and sensory processing issues. Then, in another flare, suddenly experience tics, OCD, and this time hyperactivity.
Various symptoms have co-occurring sudden onset that distinguishes the gradual emergence of the multiple symptoms someone with Tourette's disorder may get over the years.
The Dangers of Misdiagnosis
A misdiagnosis prevents people from accessing the proper treatment. The interventions that can alleviate PANS/PANDAS differ from the methods used to manage Tourette's Syndrome.
While the common psychotherapeutic strategies to ease tics are sometimes applied in PANS/PANDAS, they may not target the entire medical complexity. PANS/PANDAS treatment merits a five-pronged approach.
1. Address the cause of inflammation
2. Strengthen the dysregulated immune system,
3. Manage manifestations psychotherapeutically, as necessary
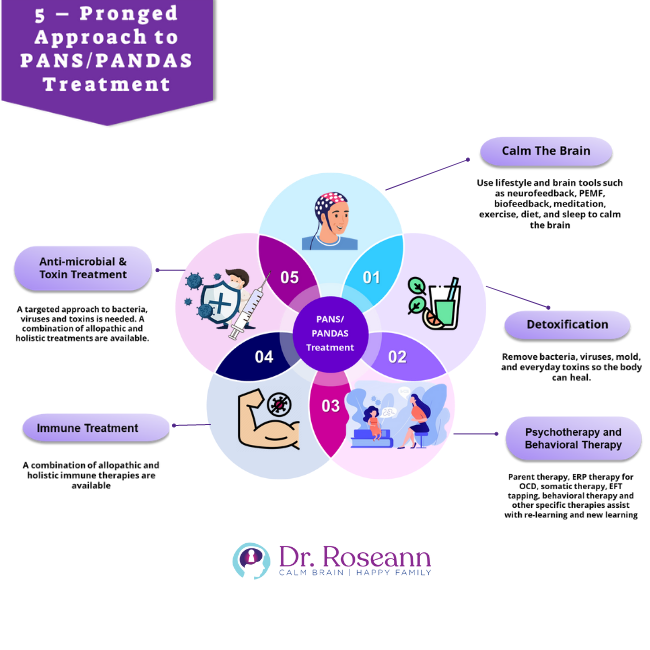
If someone with tics has PANS/PANDAS but remains undiagnosed, then they may experience improvements in their tics from psychotherapeutic intervention. However, the approach may not be enough to totally relieve motor abnormalities, eating disorders, and the other symptoms resulting from neuroinflammation and a dysregulated immune system.
Calming the brain with tools such as PEMF and neurofeedback, as well as improving the body’s detoxification process are needed to recover from
PANS/PANDAS. These same methods can help tic behaviors as well.
Misdiagnosis may cause confusion and frustration during a relapse. The new flare may come with more severe cases and can't be eased by managing tics alone. Having new symptoms out of nowhere can be terrifying for those unfamiliar with PANS/PANDAS.
Worse, PANDAS patients may receive further misdiagnosis. Medical professionals who lack knowledge of PANS/PANDAS may try to fit the symptoms of another flare to the conditions they are somewhat familiar with.
Tourette's Syndrome and PANS PANDAS are serious that can impact a child's future. Early diagnosis can help the child get the best treatment options to recover, live normally, and pursue their dreams.
Finding a doctor who can see the bigger picture is the most important thing you can do for your child.
Citations:
Aspire (2022), PANS PANDAS and Tourette Syndrome – The Overlap
https://aspire.care/families-parents-caregivers/pans-pandas-and-tourette-syndrome-the-overlap/
Medical News Today (2022), What causes different types of tic disorders?
https://www.medicalnewstoday.com/articles/317950
PANDAS Network (2022), PANDAS Signs and Symptoms
https://pandasnetwork.org/understanding-pandas/signs-and-symptoms
Science Direct (2022), Tic Disorder
https://www.sciencedirect.com/topics/medicine-and-dentistry/tic-disorder
Capanna-Hodge, Roseann (2021), It's Gonna Be Okay
https://www.itsgonnabeok.com/book-landing-page1616094622787
Garcia, Hecto and Miralles, Francesc (2017), Ikigai
https://www.goodreads.com/en/book/show/40534545-ikigai
Time (2018), 5 Places Where People Live the Longest and Healthiest Lives
https://time.com/5160475/blue-zones-healthy-long-lives/
Always remember… “Calm Brain, Happy Family™”
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about solutions, so you are in the right place!
There are 3 ways to work with Dr. Roseann:
You can get her books for parents and professionals, including: It’s Gonna Be OK™: Proven Ways to Improve Your Child’s Mental Health, Teletherapy Toolkit™ and Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.
If you are a business or organization that needs proactive guidance to support employee mental health or an organization looking for a brand representative, check out Dr. Roseann’s media page and professional speaking page to see how we can work together.
Dr. Roseann is a Children’s Mental Health Expert and Therapist who has been featured in/on hundreds of media outlets including, CBS, NBC, FOX News, PIX11 NYC, The New York Times, The Washington Post,, Business Insider, USA Today, CNET, Marth Stewart, and PARENTS. FORBES called her, “A thought leader in children’s mental health.”

She is the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann Capanna-Hodge. Dr. Roseann is a Board Certified Neurofeedback (BCN) Practitioner, a Board Member of the Northeast Region Biofeedback Society (NRBS), Certified Integrative Medicine Mental Health Provider (CMHIMP) and an Amen Clinic Certified Brain Health Coach. She is also a member of The International Lyme Disease and Associated Disease Society (ILADS), The American Psychological Association (APA), Anxiety and Depression Association of America (ADAA) National Association of School Psychologists (NASP), International OCD Foundation (IOCDF) International Society for Neurofeedback and Research (ISNR) and The Association of Applied Psychophysiology and Biofeedback (AAPB).
© Roseann-Capanna-Hodge, LLC 2023
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.